Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (21): 3293-3298.doi: 10.12307/2024.077
Previous Articles Next Articles
Finite element mechanical analysis of different screw-rod internal fixation methods in lateral lumbar fusion
Tang Fubo, Zhong Yuanming, Li Zhifei
- First Affiliated Hospital, Guangxi University of Chinese Medicine, Nanning 530001, Guangxi Zhuang Autonomous Region, China
-
Received:2023-04-20Accepted:2023-06-16Online:2024-07-28Published:2023-09-27 -
Contact:Li Zhifei, Master, Chief physician, Professor, First Affiliated Hospital, Guangxi University of Chinese Medicine, Nanning 530001, Guangxi Zhuang Autonomous Region, China -
About author:Tang Fubo, Associate chief physician, First Affiliated Hospital, Guangxi University of Chinese Medicine, Nanning 530001, Guangxi Zhuang Autonomous Region, China -
Supported by:National Natural Science Foundation of China, No. 81760874, 82260942 (to ZYM); Guangxi Key Research & Development Plan Project, No. Guike AB20159018 (to ZYM); Guangxi Key Discipline Construction Project of Traditional Chinese Medicine, No. GZXK-Z-20-21 (to ZYM); Guangxi Zhuang Autonomous Region Traditional Chinese Medicine Administration Plan Project, No. GXZYA20220025 (to TFB); General Project of Guangxi Natural Science Foundation, No. 2023GXNSFAA026101 (to LZF); Guangxi TCM Clinical Excellent Talent Training Target, No. Guangxi TCM[2022]14 (to LZF)
CLC Number:
Cite this article
Tang Fubo, Zhong Yuanming, Li Zhifei. Finite element mechanical analysis of different screw-rod internal fixation methods in lateral lumbar fusion[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(21): 3293-3298.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
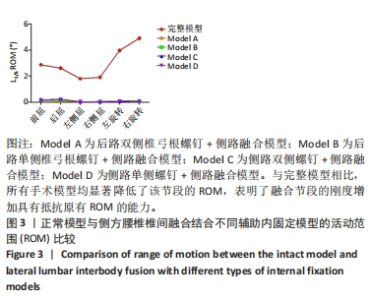
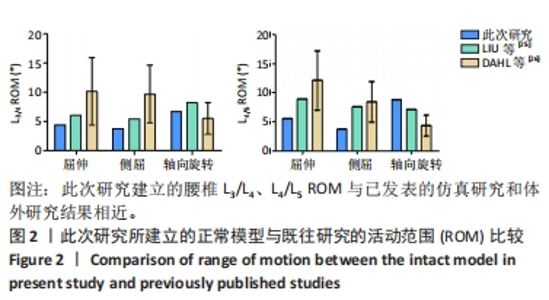
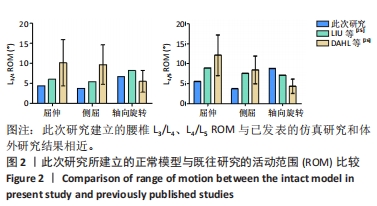
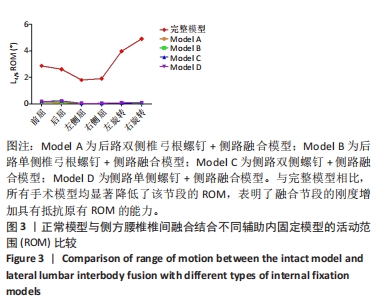
2.2 不同侧路融合的内固定置入重建模型在不同生理应力下 ROM的比较 从图3可见,与完整模型相比,所有手术模型均显著降低了L4-L5节段的ROM。在屈伸ROM方面,Model A和Model B较正常模型降低了95.81%和94.16%,而Model C和Model D则分别降低了92.35%和92.53%。在侧屈ROM方面,由于为右侧置钉,Model C和Model D的右侧屈ROM限制最多,分别降低了97.56%和97.59%的活动度。在轴向旋转ROM的比较中,Model A和Model B通过脊柱三柱的固定,分别降低了98.53%和98.31%的ROM。在4个内固定模型的单独比较中,Model A和Model B在屈伸工况下较Model C和Model D多21.85%-45.26%的ROM限制;而后者在侧屈工况限制最多,较前者增加了约5.26%的ROM限制;在轴向旋转工况的比较中,Model A和Model B在屈伸工况下较Model C和Model D多6.17%-23.26%的ROM限制,见图4。"
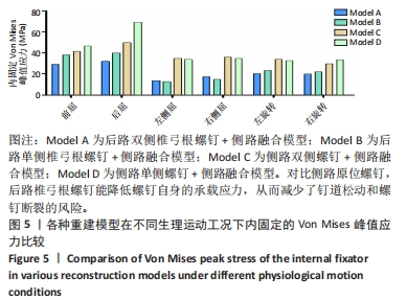
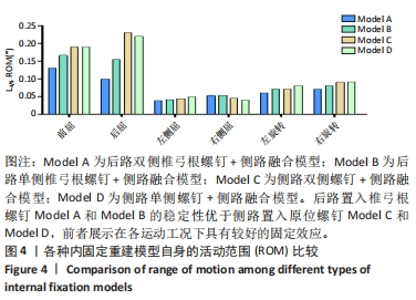
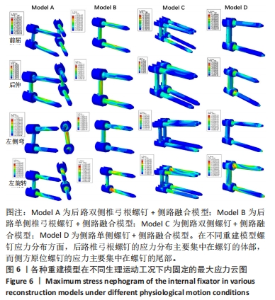
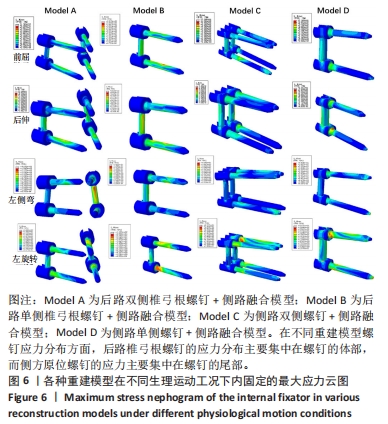
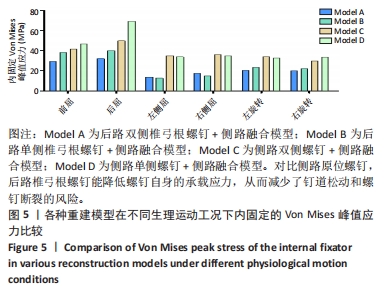
2.3 各种内固定重建模型的螺钉von Mises峰值应力比较 从图5可见,后路椎弓根螺钉和侧路原位螺钉的von Mises峰值应力均发生在所有模型的屈伸运动工况中,后路椎弓根螺钉的峰值应力与侧路原位螺钉的峰值应力比较差异超过67.74 MPa。其中,Model A在屈伸工况的峰值应力最小为61.47 MPa,分别较Model B减少了21.24%、较Model C减少了32.80%以及较Model D减少了46.91%的峰值应力。螺钉最大的Von Mises峰值应力出现在Model D的后伸工况,达到69.25 MPa。在侧屈的运动工况中,后路椎弓根螺钉的峰值应力与侧路原位螺钉的峰值应力比较差异超过80.10 MPa,前者较后者少负载54.15%-60.73%的螺钉峰值应力。然而,单侧和双侧的螺钉固定在侧屈工况比较中差异并不显著,如Model A和Model B的螺钉应力差异为3.71 MPa,以及Model C和Model D的螺钉应力差异为2.05 MPa。在轴向旋转的运动工况比较中发现,后路椎弓根螺钉的峰值应力与侧路原位螺钉的峰值应力比较差异为43.95 MPa,前者较后者少负载30.58%-38.70%的螺钉峰值应力。单侧和双侧的螺钉固定在此工况比较中差异也并不显著。在螺钉应力分布云图的比较中发现,Model A和Model B螺钉的应力分布主要集中在椎弓根螺钉的体部,而Model C和Model D的峰值应力主要集中在原位螺钉的尾部,详见图6。"
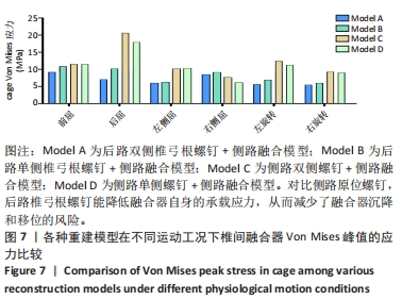
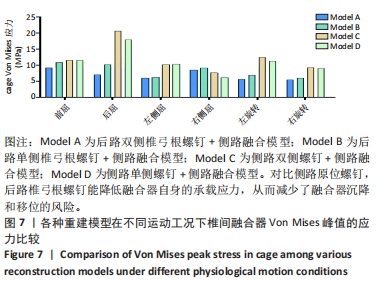
2.4 各种内固定重建模型的螺钉的椎间融合器Von Mises 峰值应力比较 不同重构模型在各种运动工况下椎间融合器Von Mises峰值应力比较见图7。总体来说,后路椎弓根螺钉固定较侧路原位螺钉固定承载的融合器峰值应力小,椎间融合器最大的Von Mises峰值应力出现在Model C和Model D的后伸工况。在屈伸运动工况的比较中,前者较后者少承载39.37%的峰值应力;在侧屈、轴向旋转的运动工况中,前者较后者少承载13.01%和42.86%的峰值应力。在右侧屈的运动工况中显示,右侧置入螺钉的Model C和Model D的椎间融合器较后路置入螺钉的Model A和Model B少承载9.65%-32.57%峰值应力;而左侧屈的工况相反,前者较后者多39.24%-41.39%的峰值应力。"
| [1] MARCHI L, ABDALA N, OLIVEIRA L, et al. Radiographic and clinical evaluation of cage subsidence after stand-alone lateral interbody fusion. J Neurosurg Spine. 2013;19(1): 110-118. [2] TOWERS WS, KURTOM KH. Stand-alone LLIF Lateral Cage Migration: A Case Report. Cureus. 2015;7(10):e347. [3] RATHBONE J, RACKHAM M, NIELSEN D, et al. A systematic review of anterior lumbar interbody fusion (ALIF) versus posterior lumbar interbody fusion (PLIF), transforaminal lumbar interbody fusion (TLIF), posterolateral lumbar fusion (PLF). Eur Spine J. 2023; 32(6):1911-1926. [4] ISSA TZ, LEE Y, LAMBRECHTS MJ, et al. Comparing Posterior Lumbar Decompression and Fusion and Transforaminal Lumbar Interbody Fusion in Lumbar Degenerative Spondylolisthesis as Assessed by the CARDS Classification System. World Neurosurg. 2023:S1878-8750(23)00520-X. [5] CHANBOUR H, STEINLE AM, TANG AR, et al. In Single-Level, Open, Posterior Lumbar Fusion, Does Transforaminal Lumbar Interbody Fusion or Posterolateral Fusion Lead to Better Outcomes? Neurosurgery. 2023; 92(1):110-117. [6] HIYAMA A, SAKAI D, SATO M, et al. The analysis of percutaneous pedicle screw technique with guide wire-less in lateral decubitus position following extreme lateral interbody fusion. J Orthop Surg Res. 2019;14(1):304. [7] JI Y, ZHANG Q, SONG Y, et al. Biomechanical characteristics of 2 different posterior fixation methods of bilateral pedicle screws: A finite element analysis. Medicine (Baltimore). 2022;101(36):e30419. [8] XU L, LIN X, WU C, et al. Is unilateral pedicle screw fixation as effective as bilateral pedicle screw fixation in transforaminal lumbar interbody fusion: a meta-analysis of randomized controlled trials. Eur Spine J. 2023;32(2):700-711. [9] WU J, HAN Y, XU H, et al. Biomechanical comparison of spinal column shortening - a finite element study. BMC Musculoskelet Disord. 2022;23(1):1122. [10] CHOI YH, KWON SW, MOON JH, et al. Lateral Lumbar Interbody Fusion and in Situ Screw Fixation for Rostral Adjacent Segment Stenosis of the Lumbar Spine. J Korean Neurosurg Soc. 2017;60(6):755-762. [11] KUBOTA G, ORITA S, UMIMURA T, et al. Insidious intraoperative ureteral injury as a complication in oblique lumbar interbody fusion surgery: a case report. BMC Res Notes. 2017;10(1):193. [12] WONG CE, HU HT, HUANG YH, et al. Optimization of Spinal Reconstructions for Thoracolumbar Burst Fractures to Prevent Proximal Junctional Complications: A Finite Element Study. Bioengineering (Basel). 2022;9(10):491. [13] ZHANG J, CHEN W, WENG R, et al. Biomechanical effect of endplate defects on the intermediate vertebral bone in consecutive two-level anterior cervical discectomy and fusion: a finite element analysis. BMC Musculoskelet Disord. 2023;24(1):407. [14] LIANG Z, CUI J, ZHANG J, et al. Biomechanical evaluation of strategies for adjacent segment disease after lateral lumbar interbody fusion: is the extension of pedicle screws necessary? BMC Musculoskelet Disord. 2020;21(1):117. [15] CASAROLI G, GALBUSERA F, JONAS R, et al. A novel finite element model of the ovine lumbar intervertebral disc with anisotropic hyperelastic material properties. PLoS One. 2017;12(5):e0177088. [16] DAMM N, ROCKENFELLER R, GRUBER K. Lumbar spinal ligament characteristics extracted from stepwise reduction experiments allow for preciser modeling than literature data. Biomech Model Mechanobiol. 2020;19(3):893-910. [17] WANG W, PAN F, WANG P, et al. Biomechanical Response of Four Roussouly’s Sagittal Alignment Lumbar to Degeneration of Different Parts of Intervertebral Disc: Finite Element Model Analysis. IRBM. 2023;44(4):100772. [18] LIANG Z, XU G, LIU T, et al. Quantitatively biomechanical response analysis of posterior musculature reconstruction in cervical single-door laminoplasty. Comput Methods Programs Biomed. 2023;233:107479. [19] XU M, YANG J, LIEBERMAN IH, et al. Lumbar spine finite element model for healthy subjects: development and validation. Comput Methods Biomech Biomed Engin. 2017; 20(1):1-15. [20] HADDAS R, XU M, LIEBERMAN I, et al. Finite Element Based-Analysis for Pre and Post Lumbar Fusion of Adult Degenerative Scoliosis Patients. Spine Deform. 2019;7(4):543-552. [21] MENGONI M. Biomechanical modelling of the facet joints: a review of methods and validation processes in finite element analysis. Biomech Model Mechanobiol. 2021; 20(2):389-401. [22] KLUCK DG, FARNSWORTH CL, JEFFORDS ME, et al. Spinal rod gripping capacity: how do 5.5/6.0-mm dual-diameter screws compare? Spine Deform. 2020;8(1):25-32. [23] HAN ML, HE WH, HE ZY, et al. Anatomical characteristics affecting the surgical approach of oblique lateral lumbar interbody fusion: an MR-based observational study. J Orthop Surg Res. 2022;17(1):426. [24] WU J, FENG Q, YANG D, et al. Biomechanical evaluation of different sizes of 3D printed cage in lumbar interbody fusion-a finite element analysis. BMC Musculoskelet Disord. 2023;24(1):85. [25] LIU X, MA J, PARK P, et al. Biomechanical comparison of multilevel lateral interbody fusion with and without supplementary instrumentation: a three-dimensional finite element study. BMC Musculoskelet Disord. 2017;18(1):63. [26] DAHL MC, ELLINGSON AM, MEHTA HP, et al. The biomechanics of a multilevel lumbar spine hybrid using nucleus replacement in conjunction with fusion. Spine J. 2013;13(2): 175-183. [27] VERMA V, AGRAWAL U SR. Lumbar Pedicle Morphometry of Dry Vertebral Columns in Relation to Transpedicular Fixation: A Cross-Sectional Study From Central India. Cureus. 2023;15(4):e38108. [28] PIERZCHAJLO N, STEVENSON TC, HUYNH H, et al. Augmented Reality in Minimally Invasive Spinal Surgery: A Narrative Review of Available Technology. World Neurosurg. 2023;176:35-42. [29] ZHONG R, XUE X, WANG R, et al. Safety and efficacy of unilateral and bilateral pedicle screw fixation for lumbar degenerative diseases by transforaminal lumbar interbody fusion: An updated systematic review and meta-analysis. Front Neurol. 2022;13:998173. [30] WONG CE, HU HT, KAO LH, et al. Biomechanical feasibility of semi-rigid stabilization and semi-rigid lumbar interbody fusion: a finite element study. BMC Musculoskelet Disord. 2022;23(1):10. [31] YANG S, XIA H, CONG M, et al. Unilateral pedicle screw fixation of lumber spine: A safe internal fixation method. Heliyon. 2022;8(11):e11621. [32] DUJIC MK, RECNIK G, MILCIC M, et al. MRI Assessment of the Early Disc Degeneration Two Levels above Fused Lumbar Spine Segment: A Comparison after Unilateral and Bilateral Transforaminal Lumbar Interbody Fusion (TLIF) Procedure. J Clin Med. 2022; 11(14):3952. [33] BOUSTANI HN, ROHLMANN A, VAN DER PUT R, et al. Which postures are most suitable in assessing spinal fusion using radiostereometric analysis? 2012;27(2):111-116. [34] MURRAY G. Handbook of Materials Selection for Engineering Applications: Taylor & Francis, 1997. [35] EL-KADI M, DONOVAN E, EL HALABI T, et al. Risk Factors for Pedicle Screw Fracture in the Lumbar Spine. Contemporary Neurosurg. 2014;36(16):1-5. |
| [1] | Li Zhifei, Yang Yin, Chen Hualong, Liang Qinqiu, Zhong Yuanming, Zhang Yisheng. Finite element analysis of the correlation between tilt angle of titanium cage and postoperative subsidence of titanium cage after anterior subtotal cervical corpectomy, decompression and fusion [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1313-1319. |
| [2] | Ouyang Beiping, Ma Xiangyang, Luo Chunshan, Zou Xiaobao, Lu Tingsheng, Chen Qiling. Three-dimensional finite element analysis of a new horizontal screw-screw crosslink in posterior atlantoaxial internal fixation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1320-1324. |
| [3] | Chen Mengmeng, Bao Li, Chen Hao, Jia Pu, Feng Fei, Shi Guan, Tang Hai. Biomechanical characteristics of a novel interspinous distraction fusion device BacFuse for the repair of lumbar degenerative disease [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1325-1329. |
| [4] | Liang Cheng, Zhang Linqi, Wang Guan, Li Wen, Duan Ke, Li Zhong, Lu Xiaobo, Zhuo Naiqiang. Finite element and biomechanical analysis of different implants in repair for unilateral unstable pelvic posterior ring injury [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1336-1341. |
| [5] | Guo Sutong, Feng Dehong, Guo Yu, Wang Ling, Ding Yujian, Liu Yi, Qian Zhengying, Li Mingyang. Construction and finite element analysis of normal and osteoporotic hip models [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1342-1346. |
| [6] | Yang Junliang, Lu Tan, Xu Biao, Jiang Yaqiong, Wang Fucheng. Three-dimensional finite element analysis of effects of partial anterior cruciate ligament rupture on knee joint stress [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1347-1353. |
| [7] | Li Chaojie, Gulati•Maitirouzi, Aierxiding•Abulaiti, Zheng Hui, Tu Hudi. Finite element analysis of medial patellofemoral ligament reconstruction at different flexion angles [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1359-1364. |
| [8] | Xi Jintao, Lu Qilin, Wang Yang, Wang Xiaojuan, Lyu Peng, Chen Long, Shi Zhen, Xie Wei, Zhu Yiliang, Li Xugui. Risk factors for cage retropulsion following transforaminal lumbar interbody fusion [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1394-1398. |
| [9] | Niu Hegang, Yang Kun, Zhang Jingjing, Yan Yizhu, Zhang Yinshun. Design of a new posterior atlas fracture reduction and internal fixation system [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1399-1402. |
| [10] | Wang Menghan, Qi Han, Zhang Yuan, Chen Yanzhi. Three kinds of 3D printed models assisted in treatment of Robinson type II B2 clavicle fracture [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1403-1408. |
| [11] | Weng Rui, Lin Dongxin, Guo Haiwei, Zhang Wensheng, Song Yuke, Lin Hongheng, Li Wenchao, Ye Linqiang. Abnormal types of intervertebral disc structure and related mechanical loading with biomechanical factors [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1436-1442. |
| [12] | Xiaheida·Yilaerjiang, Nijiati·Tuerxun, Reyila·Kuerban, Baibujiafu·Yelisi, Chen Xin. Three-dimensional finite element analysis of the distribution pattern of stress in bone tissues with different characteristics [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1277-1282. |
| [13] | Wang Qiang, Li Shiyun, Xiong Ying, Li Tiantian. Biomechanical changes of the cervical spine in internal fixation with different anterior cervical interbody fusion systems [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 821-826. |
| [14] | Wei Yuanbiao, Lin Zhan, Chen Yanmei, Yang Tenghui, Zhao Xiao, Chen Yangsheng, Zhou Yanhui, Yang Minchao, Huang Feiqi. Finite element analysis of effects of sagittal cervical manipulation on intervertebral disc and facet joints [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 827-832. |
| [15] | Zhang Rui, Wang Kun, Shen Zicong, Mao Lu, Wu Xiaotao. Effects of endoscopic foraminoplasty and laminoplasty on biomechanical properties of intervertebral disc and isthmus [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 833-839. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||