| [1] |
Zhang Lichuang, Gao Huali, Wang Jingchao, Lin Huijun, Wu Chonggui, Ma Yinghui, Huang Yunfei, Fang Xue, Zhai Weitao.
Effect of tendon manipulation with equal emphasis on muscles and bones on accelerating the functional rehabilitation of quadriceps femoris after total knee arthroplasty
[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1383-1389.
|
| [2] |
Shao Zichen, Li Huanan, Gu Bing, Zhang Xiaoyun, Sun Weikang, Liu Yongqian, Gan Bin.
MicroRNA, long non-coding RNA and circular RNA mediate the mechanism of decreasing uric acid, anti-inflammation and regulating bone metabolism in gout
[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(5): 765-771.
|
| [3] |
Lu Huixiu, Cao Haiyu, Lou Dan, Li Jianying, Liu Hongyuan, Sun Jing.
Imiquimod combined with photodynamic therapy for hypertrophic scars: immune response and prognosis
[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(5): 690-694.
|
| [4] |
Wei Bo, Yao Qingqiang, Tang Cheng, Li Xuxiang, Xu Yan, Wang Liming.
Advantage of medial pivot prosthesis in total knee arthroplasty via medial subvastus approach
[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 552-557.
|
| [5] |
Wan Guoli, Shi Chenhui, Wang Weishan, Li Ang, Shi Xunda, Cai Yi.
Retrospective analysis of the influencing factors of chronic pain after total knee arthroplasty
[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 558-564.
|
| [6] |
Gu Mingxi, Wang Bo, Tian Fengde, An Ning, Hao Ruihu, Wang Changcheng, Guo Lin.
Comparison of early efficacy and safety of simultaneous and staged bilateral total knee arthroplasty
[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 565-571.
|
| [7] |
Zhang Jinbiao, Li Xiaoming, Xing Wanlin, Ma Fei, Yu Qiaoya, Dai Rongqin.
Early warning efficacy of thrombus molecular markers after total knee arthroplasty in patients complicated with venous thromboembolism
[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 572-577.
|
| [8] |
Xu Xiangjun, Wang Chao, Song Qunshan, Li Bingyan, Zhang Jichao, Wang Guodong, Dong Yuefu.
Optimal angle for prosthesis implantation in total knee arthroplasty
[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 612-618.
|
| [9] |
Xu Yangyang, He Peiliang, Meng Qingqi, Li Siming.
A meta-analysis of the effects of continuous adductor canal block and continuous femoral nerve block on early activity after knee arthroplasty
[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 640-645.
|
| [10] |
Chai Hao, Yang Deyong, Zhang Lei, Shu Li.
3D printing personalized osteotomy guide technology versus conventional total knee arthroplasty on the accuracy of lower limb force alignment: a meta-analysis
[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 646-654.
|
| [11] |
Hu Wei, Yan Xianke .
Effect of posterior cruciate ligament preserving knee prosthesis on gait and lower extremity venous return in varus knee arthroplasty
[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(22): 3503-3507.
|
| [12] |
Shao Zhuce, Hu Peng, Bi Shuxiong.
Establishment and validation of prediction models of affected limb swelling after primary unilateral total knee arthroplasty
[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(22): 3508-3513.
|
| [13] |
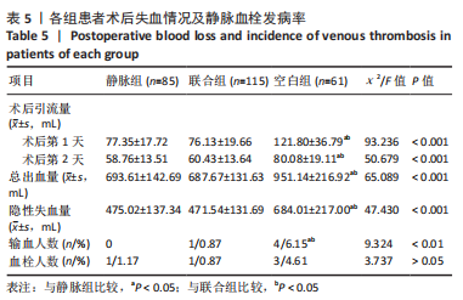
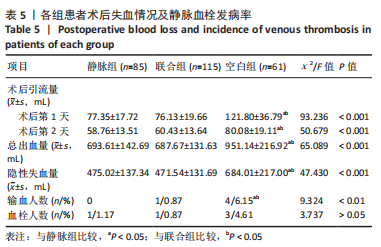
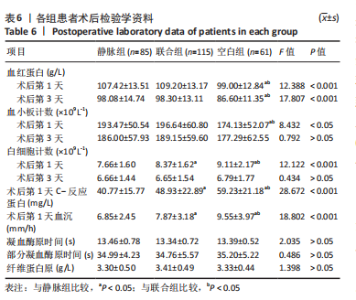
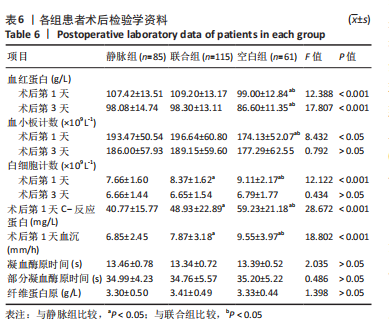
Qiu Hao, Zhu Yun, Weng Zheng, Liu Dun, Chen Shimou, Jin Guorong, Chen Yu.
Application of tranexamic acid in elderly patients with femoral intertrochanteric fracture
[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(22): 3550-3554.
|
| [14] |
Huang Huida, Huang Yongming, Zhou Junde, Liu Wenbo, Lin Yuewei, Su Haitao.
Comparison of two techniques in locating tibial prosthesis during total knee arthroplasty of varus knee
[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(13): 2038-2043.
|
| [15] |
Wu Qian, Liu Lingfeng, Li Lisong, Lu Yingjie, Zhou Liyu, Xu Wu, Huang Lixin, Jiang Dinghua.
Deep vein thrombosis distribution and risk factors after total knee arthroplasty during enhanced recovery after surgery
[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(13): 2044-2050.
|