Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (17): 2660-2666.doi: 10.12307/2022.531
Previous Articles Next Articles
Effects of zoledronic acid on alveolar bone metabolism and nucleotide-binding oligomerization domain-like receptor protein 3 inflammasome in the alveolar bone of ovariectomized osteoporosis rats
Huo Hua, Liu Guanjuan, Song Na, Zhou Qian, Cheng Yuting, Luo Shanshan, Liao Jian
- Stomatological Hospital of Guizhou Medical University, Guiyang 550004, Guizhou Province, China
-
Received:2021-03-26Revised:2021-04-01Accepted:2021-05-07Online:2022-06-18Published:2021-12-24 -
Contact:Liao Jian, MD, Professor, Chief physician, Stomatological Hospital of Guizhou Medical University, Guiyang 550004, Guizhou Province, China -
About author:Huo Hua, Master candidate, Stomatological Hospital of Guizhou Medical University, Guiyang 550004, Guizhou Province, China -
Supported by:the National Natural Science Foundation of China, No. 82060207 (to LJ)
CLC Number:
Cite this article
Huo Hua, Liu Guanjuan, Song Na, Zhou Qian, Cheng Yuting, Luo Shanshan, Liao Jian. Effects of zoledronic acid on alveolar bone metabolism and nucleotide-binding oligomerization domain-like receptor protein 3 inflammasome in the alveolar bone of ovariectomized osteoporosis rats[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(17): 2660-2666.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

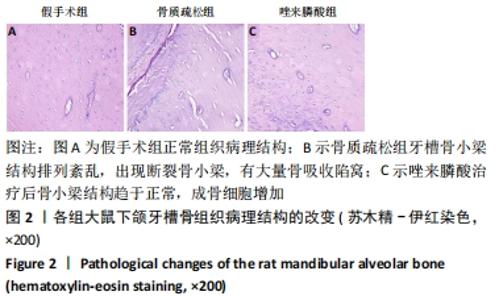
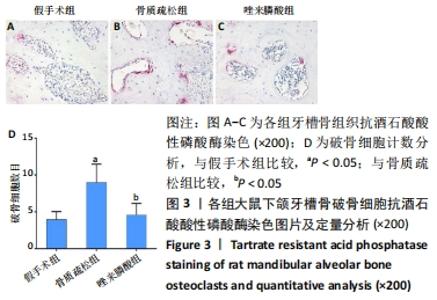
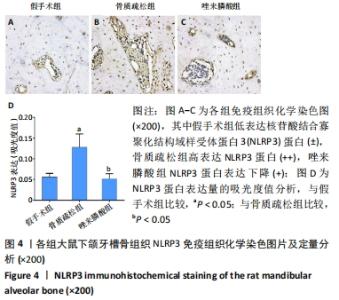
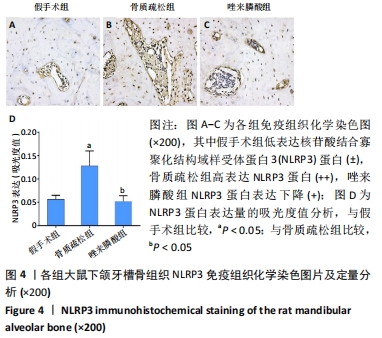
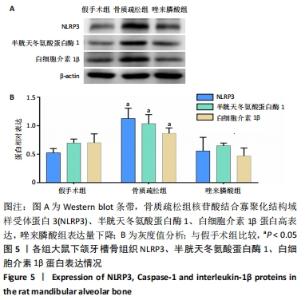
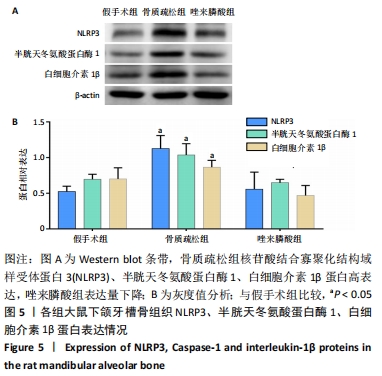
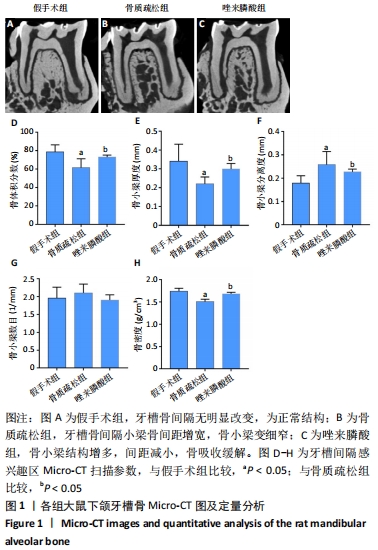
2.1 实验动物数量级分析 实验选用36只大鼠,分为3组,全部进入结果分析,无脱失。 2.2 动物大体情况 最初各组大鼠体质量、体型相似,体质量在(255.67±7.73) g范围内,毛发自然光亮。卵巢摘除术后3个月,相较于假手术组的(320.33±11.08) g,去卵巢组体质量明显增加,为(391.00±18.09) g,差异有显著性意义(P < 0.05);去卵巢组大鼠体型臃肿,毛发稀疏暗淡。 2.3 唑来膦酸对大鼠下颌牙槽骨骨吸收的影响 右侧下颌第一磨牙根尖隔牙槽骨区域,假手术组下颌牙槽骨骨小梁致密,排列整齐;骨质疏松组卵巢摘除后骨量丢失,骨小梁变细窄,小梁骨间离散程度增加;唑来膦酸组给予20 μg/kg唑来膦酸治疗4周后,恢复了骨量,可见骨小梁数目增加,排列稍致密,离散程度减小。通过Micro-CT扫描分析感兴趣区域得出牙槽骨骨微结构参数,与假手术组比较,骨质疏松组大鼠牙槽骨骨体积分数、骨小梁厚度、骨密度降低,骨小梁分离度增加,差异均有显著性意义(P < 0.05),同时也说明骨质疏松模型造模成功;与骨质疏松组相比,20 μg/kg唑来膦酸组骨体积分数、骨小梁厚度、骨密度升高,骨小梁分离度降低(P < 0.05),4周的短期治疗骨小梁数目与其他两组比较差异无显著性意义,见图1。"
| [1] ZENG Q, LI N, WANG Q, et al. The Prevalence of Osteoporosis in China, a Nationwide, Multicenter DXA Survey. J Bone Miner Res. 2019;34(10): 1789-1797. [2] SIPILÄ S, TÖRMÄKANGAS T, SILLANPÄÄ E, et al. Muscle and bone mass in middle-aged women: role of menopausal status and physical activity. J Cachexia Sarcopenia Muscle. 2020;11(3):698-709. [3] CHEN CH, WANG L, SERDAR TULU U, et al. An osteopenic/osteoporotic phenotype delays alveolar bone repair. Bone. 2018;112:212-219. [4] WAGNER F, SCHUDER K, HOF M, et al. Does osteoporosis influence the marginal peri-implant bone level in female patients? A cross-sectional study in a matched collective. Clin Implant Dent Relat Res. 2017;19(4): 616-623. [5] JEFFCOAT MK, LEWIS CE, REDDY MS, et al. Post-menopausal bone loss and its relationship to oral bone loss. Periodontol 2000. 2000;23:94-102. [6] ORYAN A,SAHVIEH S. Effects of bisphosphonates on osteoporosis: Focus on zoledronate. Life Sci. 2021;264:118681. [7] ZHOU W, LIU Y, GUO X, et al. Effects of zoledronic acid on bone mineral density around prostheses and bone metabolism markers after primary total hip arthroplasty in females with postmenopausal osteoporosis. Osteoporos Int. 2019;30(8):1581-1589. [8] EVANGELATOS G, FRAGOULIS GE, ANASTASILAKIS AD, et al. Zoledronic acid is effective in the management of migratory osteoporosis unresponsive to conservative treatment and risedronate: A case report. J Musculoskelet Neuronal Interact. 2021;21(1):138-141. [9] LIU Z, LI CW, MAO YF, et al. Study on Zoledronic Acid Reducing Acute Bone Loss and Fracture Rates in Elderly Postoperative Patients with Intertrochanteric Fractures. Orthop Surg. 2019;11(3):380-385. [10] GAO SY, ZHENG GS, WANG L, et al. Zoledronate suppressed angiogenesis and osteogenesis by inhibiting osteoclasts formation and secretion of PDGF-BB. PLoS One. 2017;12(6):e0179248. [11] PAN WL, CHEN PL, LIN CY, et al. Strontium ranelate treatment in a postmenopausal woman with osteonecrosis of the jaw after long-term oral bisphosphonate administration: a case report. Clin Interv Aging. 2017;12:1089-1093. [12] HAIDAR A, JøNLER M, FOLKMAR TB, et al. Bisphosphonate (zoledronic acid)-induced osteonecrosis of the jaw. Scand J Urol Nephrol. 2009; 43(6):442-444. [13] 程余婷, 伍超, 黄晓林, 等. 低剂量唑来膦酸对去势拔牙大鼠破骨及成骨细胞的影响[J]. 中国组织工程研究,2020,24(17):2686-2693. [14] 黄晓林, 廖健, 洪伟, 等. 破骨细胞形成过程中唑来膦酸的作用途径及机制[J]. 中国组织工程研究,2019,23(17):2716-2721. [15] HUANG XL, HUANG LY, CHENG YT, et al. Zoledronic acid inhibits osteoclast differentiation and function through the regulation of NF-kappaB and JNK signalling pathways. Int J Mol Med. 2019;44(2):582-592. [16] YOUM YH, GRANT RW, MCCABE LR, et al. Canonical Nlrp3 inflammasome links systemic low-grade inflammation to functional decline in aging. Cell Metab. 2013;18(4):519-532. [17] WANG L, HAUENSTEIN AV. The NLRP3 inflammasome: Mechanism of action, role in disease and therapies. Mol Aspects Med. 2020;76: 100889. [18] MURAKAMI T, TAKAHATA Y, HATA K, et al. Role of interleukin-1 and inflammasomes in oral disease. J Oral Biosci. 2020;62(3):242-248. [19] OHORI F, KITAURA H, OGAWA S, et al. IL-33 Inhibits TNF-α-Induced Osteoclastogenesis and Bone Resorption. Int J Mol Sci. 2020;21(3):1130. [20] ARITA Y, YOSHINAGA Y, KANEKO T, et al. Glyburide inhibits the bone resorption induced by traumatic occlusion in rats. J Periodontal Res. 2020;55(3):464-471. [21] BAUERNFEIND FG, HORVATH G, STUTZ A, et al. Cutting edge: NF-kappaB activating pattern recognition and cytokine receptors license NLRP3 inflammasome activation by regulating NLRP3 expression. J Immunol. 2009;183(2):787-791. [22] ALIPPE Y, WANG C, RICCI B, et al. Bone matrix components activate the NLRP3 inflammasome and promote osteoclast differentiation. Sci Rep. 2017;7(1):6630. [23] EPSLEY S, TADROS S, FARID A, et al. The effect of inflammation on bone. Front Physiol. 2020;11:511799. [24] KELLEY N, JELTEMA D, DUAN Y, et al. The NLRP3 Inflammasome: An Overview of Mechanisms of Activation and Regulation. Int J Mol Sci. 2019;20(13):3328. [25] YOUSEFZADEH N, KASHFI K, JEDDI S, et al. Ovariectomized rat model of osteoporosis: a practical guide. Excli J. 2020;19:89-107. [26] 许良中,杨文涛. 免疫组织化学反应结果的判断标准[J].中国癌症杂志,1996,6(4):229-231. [27] ZHOU L, FENG Y, JIN Y, et al. Verbascoside promotes apoptosis by regulating HIPK2-p53 signaling in human colorectal cancer. BMC Cancer. 2014;14:747. [28] RUCHLEMER R, AMIT-KOHN M, TVITO A, et al. Bone loss and hematological malignancies in adults: a pilot study. Support Care Cancer. 2018;26(9): 3013-3020. [29] DEREKA X, CALCIOLARI E, DONOS N, et al. Osseointegration in osteoporotic-like condition: A systematic review of preclinical studies. J Periodontal Res. 2018;53(6): 933-940. [30] GIRO G, CHAMBRONE L, GOLDSTEIN A, et al. Impact of osteoporosis in dental implants: A systematic review. World J Orthop. 2015;6(2):311-315. [31] SCHULZ MC, KOWALD J, ESTENFELDER S, et al. Site-Specific Variations in Bone Mineral Density under Systemic Conditions Inducing Osteoporosis in Minipigs. Front Physiol. 2017;8:426. [32] JOHNSTON BD,WARD WE. The ovariectomized rat as a model for studying alveolar bone loss in postmenopausal women. Biomed Res Int. 2015;2015:635023. [33] EVANGELATOS G, FRAGOULIS GE, ZAMPELI E, et al. Zoledronic acid is effective and safe in migratory osteoporosis. Rheumatology (Oxford). 2020;59(2):439-440. [34] MARUOTTI N, CORRADO A, NEVE A, et al. Bisphosphonates: effects on osteoblast. Eur J Clin Pharmacol. 2012;68(7):1013-1018. [35] 李颉颃, 苏志飞, 白璇, 等. 唑来膦酸对大鼠骨髓间充质干细胞增殖及成骨分化的作用研究[J]. 华西口腔医学杂志,2019,37(3):242-247. [36] TENENBAUM HC, TORONTALI M,SUKHU B. Effects of bisphosphonates and inorganic pyrophosphate on osteogenesis in vitro. Bone. 1992; 13(3):249-255. [37] OCHIAI H, OKADA S, SAITO A, et al. Inhibition of insulin-like growth factor-1 (IGF-1) expression by prolonged transforming growth factor-β1 (TGF-β1) administration suppresses osteoblast differentiation. J Biol Chem. 2012;287(27):22654-22661. [38] REID IR, HORNE AM, MIHOV B, et al. Anti-fracture efficacy of zoledronate in subgroups of osteopenic postmenopausal women: secondary analysis of a randomized controlled trial. J Intern Med. 2019; 286(2):221-229. [39] GHAZALI N, COLLYER JC,TIGHE JV. Hemimandibulectomy and vascularized fibula flap in bisphosphonate-induced mandibular osteonecrosis with polycythaemia rubra vera. Int J Oral Maxillofac Surg. 2013;42(1):120-123. [40] ANASTASILAKIS AD, PAPAPOULOS SE, POLYZOS SA, et al. Zoledronate for the Prevention of Bone Loss in Women Discontinuing Denosumab Treatment. A Prospective 2-Year Clinical Trial. J Bone Miner Res. 2019; 34(12):2220-2228. [41] YING G, BO L, YANJUN J, et al. Effect of a local, one time, low-dose injection of zoledronic acid on titanium implant osseointegration in ovariectomized rats. Arch Med Sci. 2016;12(5):941-949. [42] TüRKER M, ASLAN A, ÇıRPAR M, et al. Histological and biomechanical effects of zoledronate on fracture healing in an osteoporotic rat tibia model. Eklem Hastalik Cerrahisi. 2016;27(1):9-15. [43] ZHU K, ZHANG J, ZHANG C, et al. Therapeutic efficacy of zoledronic acid combined with calcitriol in elderly patients receiving total hip arthroplasty or hemiarthroplasty for osteoporotic femoral neck fracture. Osteoporos Int. 2021;32(3):559-564. [44] LEE C, LEE JH, HAN SS, et al. Site-specific and time-course changes of postmenopausal osteoporosis in rat mandible: comparative study with femur. Sci Rep. 2019;9(1):14155. [45] CHENG YT, LIAO J, ZHOU Q, et al. Zoledronic acid modulates osteoclast apoptosis through activation of the NF-κB signaling pathway in ovariectomized rats. Exp Biol Med (Maywood). 2021;246(15):1727-1739. [46] NAPETSCHNIG J, WU H. Molecular basis of NF-κB signaling. Annu Rev Biophys. 2013;42:443-468. [47] ZANG Y, SONG JH, OH SH, et al. Targeting NLRP3 Inflammasome Reduces Age-Related Experimental Alveolar Bone Loss. J Dent Res. 2020;99(11):1287-1295. [48] SHIRATORI T, KYUMOTO-NAKAMURA Y, KUKITA A, et al. IL-1β Induces Pathologically Activated Osteoclasts Bearing Extremely High Levels of Resorbing Activity: A Possible Pathological Subpopulation of Osteoclasts, Accompanied by Suppressed Expression of Kindlin-3 and Talin-1. J Immunol. 2018;200(1):218-228. |
| [1] | Zhu Chan, Han Xuke, Yao Chengjiao, Zhou Qian, Zhang Qiang, Chen Qiu. Human salivary components and osteoporosis/osteopenia [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1439-1444. |
| [2] | Jiang Huanchang, Zhang Zhaofei, Liang De, Jiang Xiaobing, Yang Xiaodong, Liu Zhixiang. Comparison of advantages between unilateral multidirectional curved and straight vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1407-1411. |
| [3] | Li Wei, Zhu Hanmin, Wang Xin, Gao Xue, Cui Jing, Liu Yuxin, Huang Shuming. Effect of Zuogui Wan on bone morphogenetic protein 2 signaling pathway in ovariectomized osteoporosis mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1173-1179. |
| [4] | Wang Jing, Xiong Shan, Cao Jin, Feng Linwei, Wang Xin. Role and mechanism of interleukin-3 in bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1260-1265. |
| [5] | Xiao Hao, Liu Jing, Zhou Jun. Research progress of pulsed electromagnetic field in the treatment of postmenopausal osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1266-1271. |
| [6] | Gao Yujin, Peng Shuanglin, Ma Zhichao, Lu Shi, Cao Huayue, Wang Lang, Xiao Jingang. Osteogenic ability of adipose stem cells in diabetic osteoporosis mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 999-1004. |
| [7] | Peng Kun. Improvement of the treatment effect of osteoporotic fractures: research status and strategy analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 980-984. |
| [8] | Hu Weifan, Zheng Li, Li Dadi, Sun Yang, Zhao Fengchao. Overexpression of miR-25 downregulates titanium particle-induced osteoclast differentiation through the NFATc1 signaling pathway [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 682-687. |
| [9] | Shen Song, Xu Bin. Diffuse distribution of bone cement in percutaneous vertebroplasty reduces the incidence of refracture of adjacent vertebral bodies [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 499-503. |
| [10] | Ou Liang, Kong Dezhong, Xu Daoqing, Ni Jing, Fu Xingqian, Huang Weichen. Comparative clinical efficacy of polymethyl methacrylate and self-solidifying calcium phosphate cement in vertebroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 649-656. |
| [11] | Zhong Yuanming, He Bingkun, Wu Zhuotan, Wu Sixian, Wan Tong, Zhong Xifeng. Meta-analysis of efficacy and safety of Jack kyphoplasty for osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 487-492. |
| [12] | Cai Feng, Yu Bo, Zeng Duo, Chen Qincan, Liao Qi. Cortical bone trajectory in elderly patients with osteoporosis of lumbar disease [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 403-407. |
| [13] | Wu Saixuan, Zhang Mi, Dong Ming, Lu Ying, Niu Weidong. Regulatory role of Keap1/Nrf2/ARE signaling pathway in bone homeostasis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(2): 271-275. |
| [14] | Sun Youqiang, Ma Chao, Liang Mengmeng, Xin Pengfei, Zhang Hua, Xiang Xiaobing. The pivotal role of autophagy in bone cells: bone-related cell activity and bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(2): 276-282. |
| [15] | Fan Danyang, Fu Runze, Mi Jiajing, Liu Chunyan. Expression and role of cannabinoid receptors during bone remodeling [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(2): 283-288. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||