Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (2): 225-231.doi: 10.12307/2022.037
Previous Articles Next Articles
Electroacupuncture intervenes with changes of mitogen-activated protein kinase pathway in a rat model of cerebral ischemia/reperfusion due to middle cerebral artery occlusion
Lai Han1, Wang Jiao1, Dong Miaomiao1, Luo Meng1, Wang Wenhao1, Zhou Guoping1, 2
- 1Hospital of Integrated Traditional Chinese Medicine and Western Medicine, Southern Medical University, Guangzhou 510315, Guangdong Province, China; 2School of Traditional Chinese Medicine, Southern Medical University, Guangzhou 510515, Guangdong Province, China
-
Received:2020-09-17Revised:2020-09-17Accepted:2020-10-30Online:2022-01-18Published:2021-10-27 -
Contact:Zhou Guoping, Chief physician, Doctoral supervisor, Hospital of Integrated Traditional Chinese Medicine and Western Medicine, Southern Medical University, Guangzhou 510315, Guangdong Province, China; School of Traditional Chinese Medicine, Southern Medical University, Guangzhou 510515, Guangdong province, China -
About author:Lai Han, Master candidate, Hospital of Integrated Tranditonal Chinese Medicine and Western Medicine, Southern Medical University, Guangzhou 510315, Guangdong Province, China -
Supported by:the National Natural Science Foundation of China, No. 81674048 (to ZGP)
CLC Number:
Cite this article
Lai Han, Wang Jiao, Dong Miaomiao, Luo Meng, Wang Wenhao, Zhou Guoping. Electroacupuncture intervenes with changes of mitogen-activated protein kinase pathway in a rat model of cerebral ischemia/reperfusion due to middle cerebral artery occlusion[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(2): 225-231.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
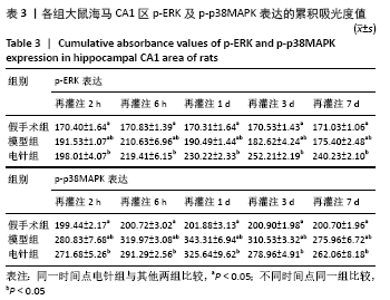
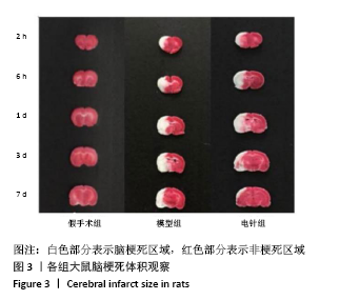
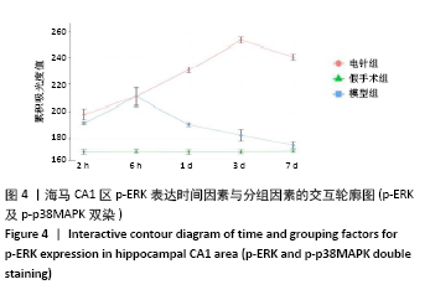
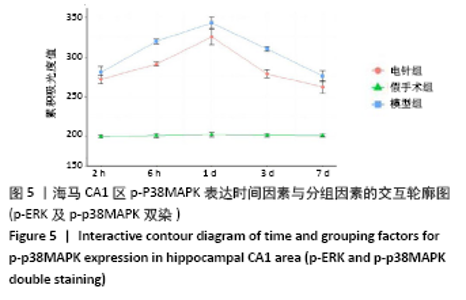
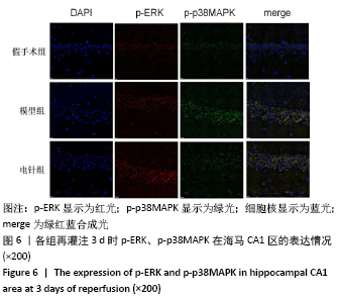
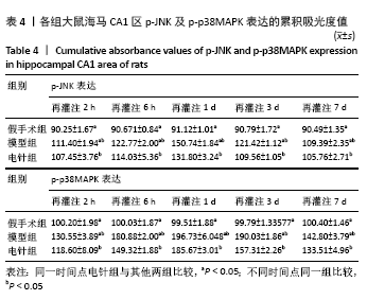
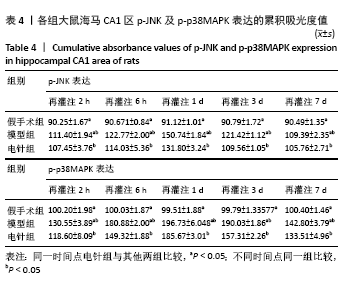
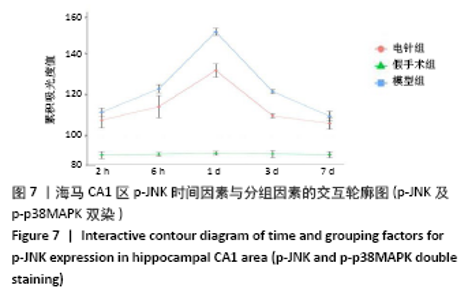
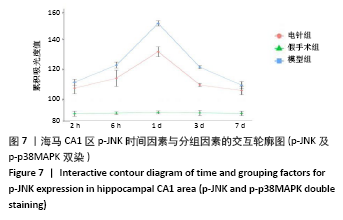
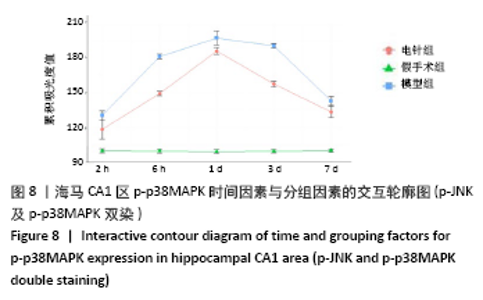
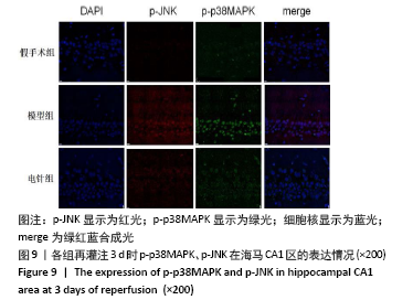
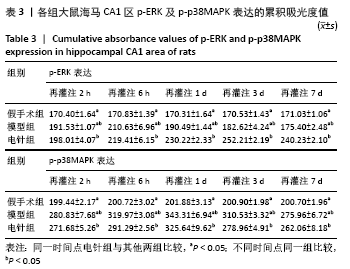
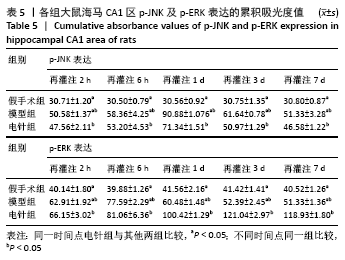
2.4 各组大鼠海马CA1区p-ERK、p-p38MAPK、p-JNK累积吸光度值的比较 2.4.1 p-ERK及p-p38MAPK双染结果的比较 假手术组中各时间亚组p-ERK、p38MAPK均有少量表达,组间表达水平比较无差异(P > 0.05)。模型组、电针组与假手术组比较差异有显著性意义(P < 0.05)。模型组p-ERK、p-p38MAPK两种指标在脑缺血再灌注2 h时表达均有升高趋势,p-ERK在6 h迅速到达峰值后逐渐回落;p-p38MAPK在3 d时达高峰(P < 0.05)。与模型组比较,脑缺血再灌注2 h时,电针组即出现p-ERK表达的上调(P < 0.05),1,3 d时间亚组上调明显,差异显著(P < 0.05);电针组p-p38MAPK表达水平与模型组相比较均有所下降,在6 h、3 d时间亚组较明显(P < 0.05)。见表3及图4,5。"

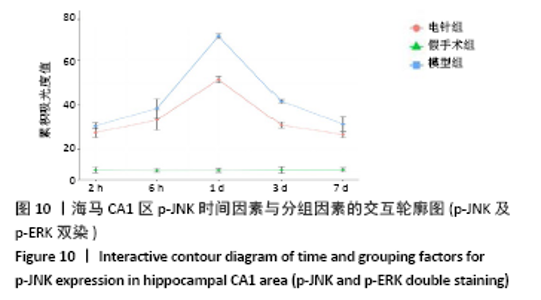
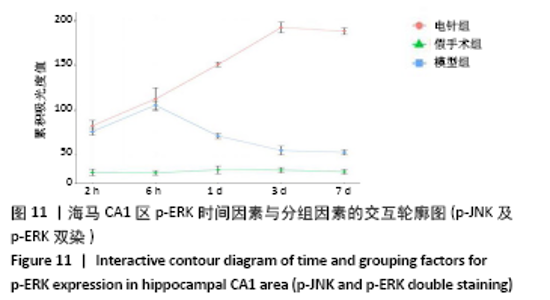
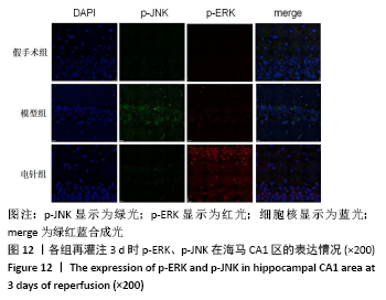
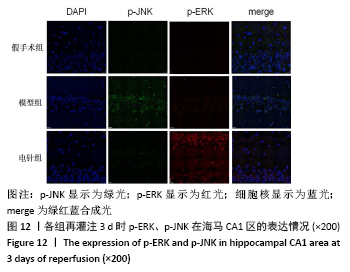
2.4.3 p-JNK及p-ERK双染结果的比较 假手术组各时间亚组p-ERK、p-JNK均有少量表达,各时间亚组间表达水平无统计学差异(P > 0.05)。模型组、电针组与假手术组比较差异有统计学意义(P < 0.05)。模型组p-ERK在2 h出现上调,在6 h迅速到达峰值后逐渐回落;p-JNK约在1 d时表达量达高峰后呈下降趋势。与模型组比较,脑缺血再灌注2 h时电针组即出现p-ERK表达的上调(P < 0.05)以及p-JNK表达的下调(P < 0.05),其中1 d、3 d时间亚组p-ERK上调明显(P < 0.05),而p-JNK的下调1 d、3 d亚组更显著(P < 0.05)。见表5,图10, 11。"
| [1] ZHOU DZ, ZHANG MM, MIN L, et al. Cerebral ischemia-reperfusion is modulated by macrophage-stimulating 1 through the MAPK-ERK signaling pathway. J Cell Physiol. 2020;235(10):7067-7080. [2] SIMÃO F, USTUNKAYA T, CLERMONT AC, et al. Plasma kallikrein mediates brain hemorrhage and edema caused by tissue plasminogen activator therapy in mice after stroke. Blood., 2017;129(16):2280-2290. [3] 邰先桃,黄学平,陈奇刚 ,等.电针对脑卒中后偏瘫患者上肢运动功能影响的研究[J].时珍国医国药,2018,29(12):2948-2950. [4] 姚书琦,易玮,刘荣,等.近5年电针预处理及电针治疗脑缺血大鼠的机制研究进展[J].针刺研究,2019,44(5):383-387. [5] WU CX, WANG J, LI C, et al. Effect of Electroacupuncture on Cell Apoptosis and ERK Signal Pathway in the Hippocampus of Adult Rats with Cerebral Ischemia-Reperfusion. Evid Based Complement Alternat Med. 2015;2015:414965. [6] LIU NN, DONG ZL, HAN LL. MicroRNA-410 inhibition of the TIMP2-dependent MAPK pathway confers neuroprotection against oxidative stress-induced apoptosis after ischemic stroke in mice. Brain Res Bull. 2018;143:45-57. [7] 李嫚,王梦嵽,梅元武,等. 不同时间窗电针治疗对脑梗死大鼠Bcl-2和BDNF表达的影响[J].中风与神经疾病杂志,2009,26(5):603-605. [8] 王占奎,倪光夏,刘坤,等. 脑缺血再灌注大鼠白细胞介素-1受体与肿瘤坏死因子-α受体变化及针刺干预的时效性研究[J].中国针灸,2012,32(11):1012-1018. [9] 陈卫伟,杨留才,潘施文,等.线栓法制备SD大鼠局灶性脑缺血再灌注损伤模型[J].中国组织工程研究与临床康复,2011,15(50):9377-9380. [10] 张艾嘉,王爽,王萍,等.缺血性脑卒中的病理机制研究进展及中医药防治[J].中国实验方剂学杂志,2020,26(5):227-240. [11] LONGA EZ, WEINSTEIN PR, CARLSON S, et al. Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke. 1989;20(1):84-91. [12] YANG ZX, XIE JH, LIU YP, et al. Systematic review of long-term Xingnao Kaiqiao needling effcacy in ischemic stroke treatment. Neural Regen Res. 2015;10(4):583-588. [13] 李菲,孙琦,邵晓梅,等. 电针配合PNF调节脑卒中患者下肢本体感觉及运动功能:随机对照研究[J].中国针灸,2019,39(10):1034-1040. [14] WANG T, WANG F, YU L, et al. Nobiletin alleviates cerebral ischemic-reperfusion injury via MAPK signaling pathway. Am J Transl Res. 2019;11(9):5967-5977. [15] XIE WJ, ZHOU P, SUN YF, et al. Protective Effects and Target Network Analysis of Ginsenoside Rg1 in Cerebral Ischemia and Reperfusion Injury: A Comprehensive Overview of Experimental Studies. Cells. 2018;7(12):270. [16] WU C, LI C, ZHOU J, et al. Effects of electroacupuncture on the cortical extracellular signal regulated kinase pathway in rats with cerebral ischaemia/reperfusion. Acupunct Med. 2017;35(6):430-436. [17] WU CX, FENG YH, YANG L, et al. Electroacupuncture exerts neuroprotective effects on ischemia/reperfusion injury in JNK knockout mice: the underlying mechanism. Neural Regen Res. 2018;13(9):1594-1601. [18] LIU HL, LIU SW, TIAN XC, et al. Bexarotene Attenuates Focal Cerebral Ischemia-Reperfusion Injury via the Suppression of JNK/Caspase-3 Signaling Pathway. Neurochem Res. 2019;44(12):2809-2820. [19] LIANG YJ, YANG WX. Kinesins in MAPK cascade: How kinesin motors are involved in the MAPK pathway? Gene. 2019;684:1-9. [20] YONG YX, YANG H, LIAN J, et al. Up-regulated microRNA-199b-3p represses the apoptosis of cerebral microvascular endothelial cells in ischemic stroke through down-regulation of MAPK/ERK/EGR1 axis. Cell Cycle. 2019;18(16):1868-1881. [21] PENG WN, MO XY, LI LH, et al. PAQR3 protects against oxygen-glucose deprivation/reperfusion-induced injury through the ERK signaling pathway in N2A cells. J Mol Histol. 2020;51(3):307-315. [22] XING Y, YANG DS, WANG MM, et al. Electroacupuncture Alleviated Neuronal Apoptosis Following Ischemic Stroke in Rats via Midkine and ERK/JNK/p38 Signaling Pathway. J Mol Neurosci. 2018;66(1):26-36. [23] LIU J, WANG Q, YANG SL, et al. Electroacupuncture Inhibits Apoptosis of Peri-Ischemic Regions via Modulating p38, Extracellular Signal-Regulated Kinase (ERK1/2), and c-Jun N Terminal Kinases (JNK) in Cerebral Ischemia-Reperfusion-Injured Rats. Med Sci Monit. 2018;24:4395-4404. |
| [1] | Wang Jianping, Zhang Xiaohui, Yu Jinwei, Wei Shaoliang, Zhang Xinmin, Xu Xingxin, Qu Haijun. Application of knee joint motion analysis in machanism based on three-dimensional image registration and coordinate transformation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(在线): 1-5. |
| [2] | Zhang Haobo, Zhao Yunan, Yang Xuejun. Role and therapeutic implications of pyroptosis in intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1445-1451. |
| [3] | Jing Jinpeng, Zhang Yue, Liu Xiaomin, Liu Yi. Traditional Chinese medicine injection for promoting blood circulation in prevention of deep vein thrombosis after orthopedic surgery: network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1467-1476. |
| [4] | Li Huo, Wang Peng, Gao Jianming, Jiang Haoran, Lu Xiaobo, Peng Jiang. Relationship between revascularization and internal microstructure changes in osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1323-1328. |
| [5] | Bao Xianguo, Gao Zengxin, Wu Zhanpo, Chen Youmin, Cheng Qinghua, Lu Haitao, Guo Changzheng, Xu Shuai. Correlation between lumbar posterior muscle and local kyphosis in patients with degenerative thoracolumbar kyphosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1418-1423. |
| [6] | Zhu Chan, Han Xuke, Yao Chengjiao, Zhang Qiang, Liu Jing, Shao Ming. Acupuncture for Parkinson’s disease: an insight into the action mechanism in animal experiments [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1272-1277. |
| [7] | Gu Zhengqiu, Xu Fei, Wei Jia, Zou Yongdi, Wang Xiaolu, Li Yongming. Exploratory study on talk test as a measure of intensity in blood flow restriction training [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1154-1159. |
| [8] | Kong Yamin, Yan Juntao, Ma Bingxiang, Li Huawei. Massage vibration intervenes with MyoD expression and proliferation and differentiation of muscle satellite cells in rats with sciatic nerve injury [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1160-1166. |
| [9] | Wu Cong, Jia Quanzhong, Liu Lun. Relationship between transforming growth factor beta1 expression and chondrocyte migration in adult articular cartilage after fragmentation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1167-1172. |
| [10] | Li Zhiyi, He Pengcheng, Bian Tianyue, Xiao Yuxia, Gao Lu, Liu Huasheng. Bibliometric and visualized analysis of ferroptosis mechanism research [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1202-1209. |
| [11] | Xiang Xinjian, Liu Fang, Wu Liangliang, Jia Daping, Tao Yue, Zhao Zhengnan, Zhao Yu. High-dose vitamin C promotes the survival of autologous fat transplantation in rats [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1242-1246. |
| [12] | Xiao Yang, Gong Liqiong, Fei Jing, Li Leiji. Effect of electroacupuncture on nerve growth factor and its receptor expression in facial nerve nucleus after facial nerve injury in rabbits [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1253-1259. |
| [13] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [14] | Wang Jifang, Bao Zhen, Qiao Yahong. miR-206 regulates EVI1 gene expression and cell biological behavior in stem cells of small cell lung cancer [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1027-1031. |
| [15] | Zhu Bingbing, Deng Jianghua, Chen Jingjing, Mu Xiaoling. Interleukin-8 receptor enhances the migration and adhesion of umbilical cord mesenchymal stem cells to injured endothelium [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1045-1050. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||