Chinese Journal of Tissue Engineering Research ›› 2021, Vol. 25 ›› Issue (27): 4415-4420.doi: 10.12307/2021.206
Previous Articles Next Articles
Meta-analysis of complications and functional recovery of the hip after total hip arthroplasty in patients with systemic lupus erythematosus
Hong Xuezhi, Liu Lei, Yao Yunqian, Jiang Yuxin, Xu Jia, Mo Hanyou
- Department of Rheumatology, Affiliated Hospital of Guilin Medical College, Guilin 541000, Guangxi Zhuang Autonomous Region, China
-
Received:2020-09-28Revised:2020-09-30Accepted:2020-11-19Online:2021-09-28Published:2021-04-10 -
Contact:Mo Hanyou, Master, Chief physician, Department of Rheumatology, Affiliated Hospital of Guilin Medical College, Guilin 541000, Guangxi Zhuang Autonomous Region, China -
About author:Hong Xuezhi, Master, Attending physician, Department of Rheumatology, Affiliated Hospital of Guilin Medical College, Guilin 541000, Guangxi Zhuang Autonomous Region, China -
Supported by:the National Natural Science Foundation of China, No. 81760298 (to MHY);the Natural Science Foundation of Guangxi Zhuang Autonomous Region, No.2020GXNSFBA297149 (to HXZ)
CLC Number:
Cite this article
Hong Xuezhi, Liu Lei, Yao Yunqian, Jiang Yuxin, Xu Jia, Mo Hanyou. Meta-analysis of complications and functional recovery of the hip after total hip arthroplasty in patients with systemic lupus erythematosus[J]. Chinese Journal of Tissue Engineering Research, 2021, 25(27): 4415-4420.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
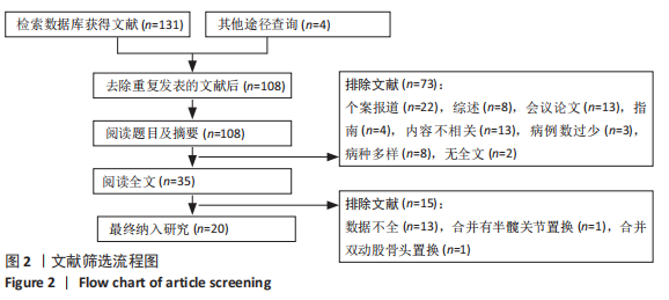
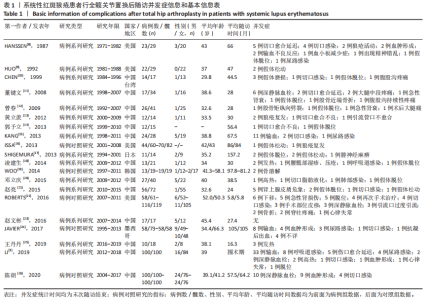
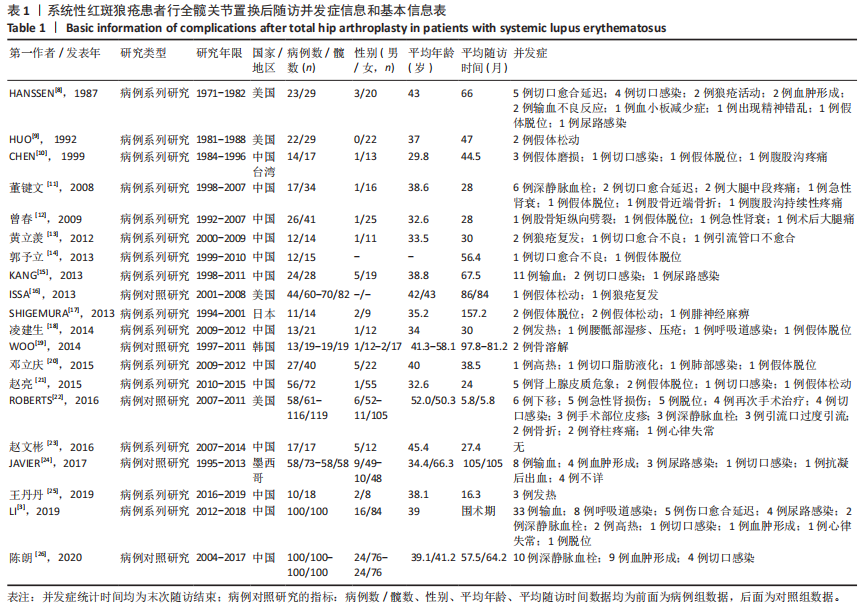
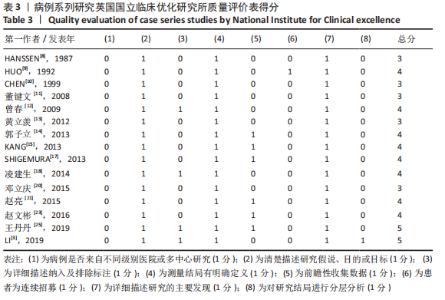
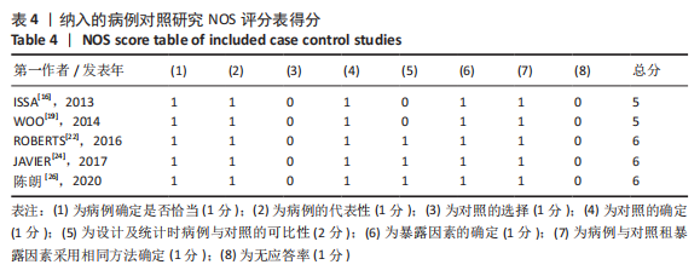
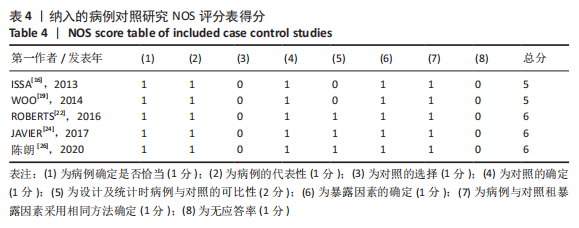
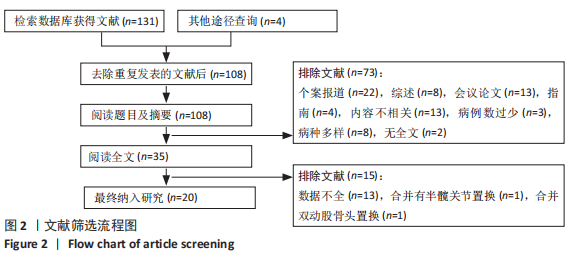
2.1 文献筛选及质量评估结果与研究基本特征 文章共检索获得135篇文献,去重后剩余108篇;经阅读标题、摘要及全文的方式进行筛选见图2,最终纳入20篇进行研究[3, 8-26],见表1,文献质量评价显示10篇文献为高质量[3,9,12,14-15,17-18,21,23,25],有5篇文献为中等质量[16,19,22,24,26],5篇为低质量研究[8,10-11,13,20],见表2-4。有5篇文献设置了对照组[16,19,22,24,26],见表2,有2篇文献未提供具体性别例数[14,16]。共纳入系统性红斑狼疮患者657例,男84例,女性517例;共行全髋关节置换802处(置换关节个数),其中手术患者最小年龄16岁,最大年龄87岁;平均随访时间为53.3个月。"
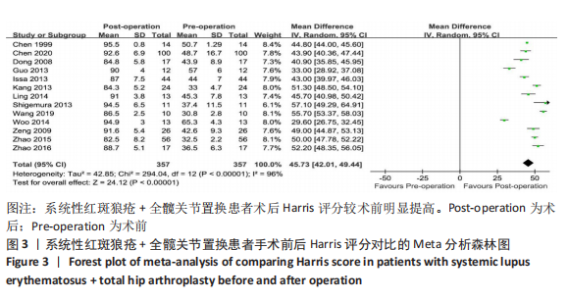
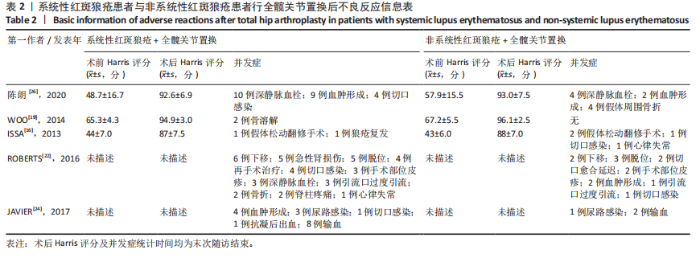
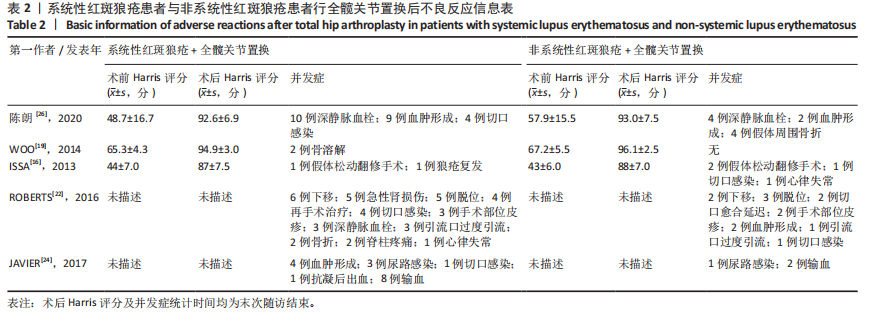
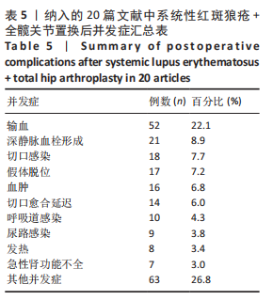
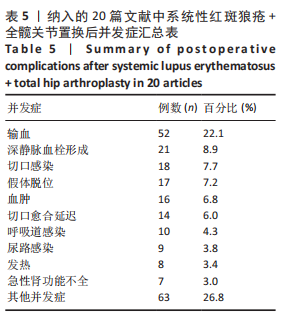
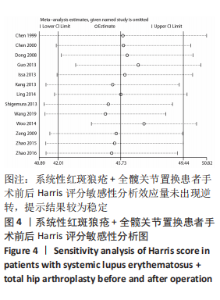
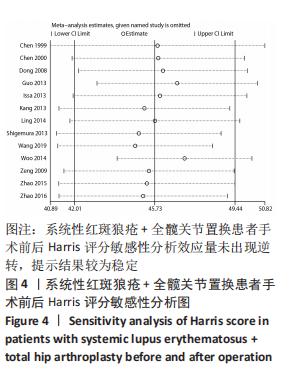
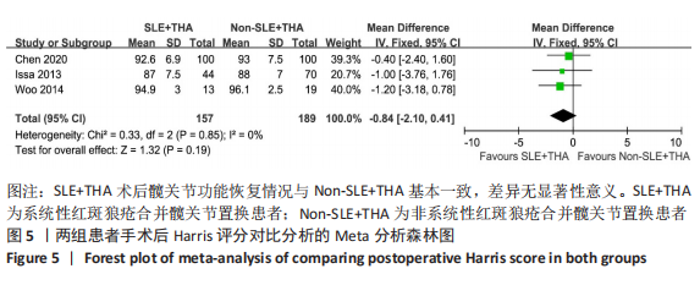
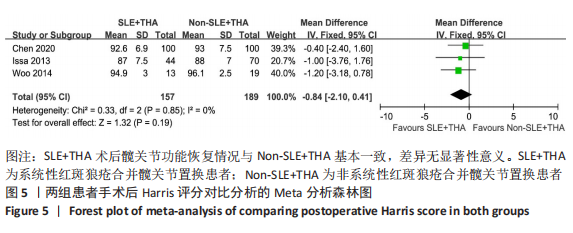
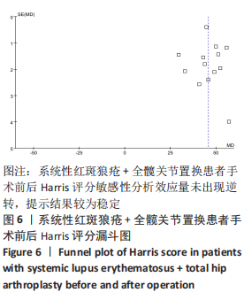
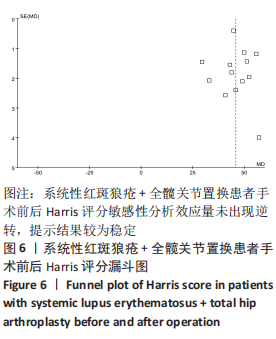
2.3 纳入研究不良事件发生率比较 所有文献中有12篇描述了系统性红斑狼疮+全髋关节置换后不良反应发生率[3,8-9,12,14-16,19-20,24-26];其不良反应发生率为3.3%-44.8%。在合并对照组的研究中,系统性红斑狼疮+全髋关节置换组313例髋关节置换中不良反应86次;非系统性红斑狼疮+全髋关节置换组378例髋关节置换中不良反应30次,卡方检验(χ2=46.78,P < 0.001,OR=4.7,95%CI:2.81-6.88)。 2.4 Meta分析结果 2.4.1 系统性红斑狼疮患者行全髋关节置换手术前后Harris评分比较的Meta分析 在20篇文献中有13篇对所有系统性红斑狼疮患者手术前后Harris评分进行详细描述[10-12,14-19,21,23,25-26]。结果显示有一定异质性(P < 0.01,I2=96%),随机效应模型结果显示差异有显著性意义(MD = 45.73,95% CI:42.0-49.4,P < 0.01),见图3,敏感性分析中效应量结果未出现逆转,提示结果较为稳定,见图4。Harris平均评分从术前的43.7分提高到最后随访的89.5分,提示全髋关节置换手术后系统性红斑狼疮患者髋关节功能得到明显改善。"

| [1] ZUCCHI D, ELEFANTE E, CALABRESI E, et al. One year in review 2019: systemic lupus erythematosus. Clin Exp Rheumatol. 2019;37(5):715-722. [2] KENNEDY JW, KHAN W. Total hip arthroplasty in systemic lupus erythematosus:a systematic review. Int J Rheumatol. 2015;2015:475-489. [3] LI Z, DU Y, XIANG S, et al. Risk factors of perioperative complications and transfusion following total hip arthroplasty in systemic lupus erythematosus patients. Lupus. 2019;28(9):1134-1140. [4] MERTELSMANN-VOSS C, LYMAN S, PAN TJ, et al. Arthroplasty rates are increased among US patients with systemic lupus erythematosus: 1991-2005. J Rheumatol. 2014;41(5):867-874. [5] AZIZ KT, BEST MJ, SKOLASKY RL, et al. Lupus and perioperative complications in elective primary total hip or knee arthroplasty. Clin Orthop Surg. 2020;12(1):37-42. [6] 郑晗晗,江学良.粪便菌群移植治疗艰难梭菌感染有效性和安全性的Meta分析[J].中国全科医学,2016,19(2):199-205. [7] STANG A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603-605. [8] HANSSEN AD, CABANELA ME, MICHET CJ JR. Hip arthroplasty in patients with systemic lupus erythematosus. J Bone Joint Surg Am. 1987;69(6): 807-814. [9] HUO MH, SALVATI EA, BROWNE MG, et al. Primary total hip arthroplasty in systemic lupus erythematosus. J Arthroplasty. 1992;7(1):51-56. [10] CHEN YW, CHANG JK, HUANG KY, et al. Hip arthroplasty for osteonecrosis in patients with systemic lupus erythematosus. Kaohsiung J Med Sci. 1999;15(12):697-670. [11] 董健文,黄冬梅,戎利民,等.Ⅰ期双侧全髋关节置换治疗系统性红斑狼疮合并股骨头坏死的早中期疗效[J].中华损伤与修复杂志,2008, 6(3):705-711. [12] 曾春,宋炎成,蔡道章,等.系统性红斑狼疮合并股骨头坏死行全髋关节置换术的特点及其并发症的防治[J].中华关节外科杂志,2009,4(3): 454-458. [13] 黄立羡,练克俭,郭林新,等.系统性红斑狼疮激素治疗后股骨头坏死行人工全髋关节置换术围术期处理[J].临床骨科杂志,2012,6(15):607-609. [14] 郭予立,胡奕山,林本丹.合并系统性红斑狼疮的股骨头坏死患者行全髋关节置换术的疗效评估[J].广东医学,2013,19(34):2984-2986. [15] KANG Y, ZHANG ZJ, ZHAO XY, et al. Total hip arthroplasty for vascular necrosis of the femoral head in patients with systemic lupus erythematosus: a midterm follow-up study of 28 hips in 24 patients. Eur J Orthop Surg Traumatol. 2013;23(1):73-79. [16] ISSA K, NAZIRI Q, RASQUINHA VJ, et al. Outcomes of primary total hip arthroplasty in systemic lupus erythematosus with a proximally-coated cementless stem. J Arthroplasty. 2013;28(9):1663-1666. [17] SHIGEMURA T, KISHIDA S, IIDA S. Cementless total hip arthroplasty for osteonecrosis of the femoral head in systemic lupus erythematosus: a study with 10–16 years of follow-up. European Orthopaedics and Traumatology. 2013;1(4):15-20. [18] 凌建生.人工全髋关节置换治疗系统性红斑狼疮合并股骨头坏死围术期处理及临床疗效分析[D].长春:吉林大学,2014. [19] WOO MS, KANG JS, MOON KH. Outcome of total hip arthroplasty for avascular necrosis of the femoral head in systemic lupus erythematosus. J Arthroplasty. 2014;29(12):2267-2270. [20] 邓立庆,康鹏德,裴福兴,等.系统性红斑狼疮合并股骨头坏死行全髋关节置换术围术期处理[J].华西医学,2015,5(30):865-868. [21] 赵亮,史哲,吴宣平,等.系统性红斑狼疮合并股骨头坏死全髋关节置换术的围术期治疗[J].中华关节外科杂志,2015,9(4):463-467. [22] ROBERTS JE, MANDL LA, SU EP, et al. Patients with systemic lupus erythematosus have increased risk of short-term adverse events after total hip arthroplasty. J Rheumatol. 2016;43(8):1498-1502. [23] 赵文彬.合并骨质疏松的系统性红斑狼疮患者行全髋关节置换术的疗效评估[J].中国伤残医学,2016,19(24):28-30. [24] MERAYO-CHALICO J, GÓNZALEZ-CONTRERAS M, ORTÍZ-HERNÁNDEZ R, et al. Total hip arthroplasty outcomes: an 18-year experience in a single center: is systemic lupus erythematosus a potential risk factor for adverse outcomes? J Arthroplasty. 2017;32(11):3462-3467. [25] 王丹丹.黄芪寄生汤配合全髋关节置换术治疗系统性红斑狼疮合并股骨头坏死的临床疗效分析[D].济南:山东中医药大学,2019. [26] 陈朗,冯辉雄,李宏超,等.系统性红斑狼疮患者行全髋关节置换术治疗股骨头坏死的疗效研究[J].中华骨与关节外科杂志,2020,2(13):143-147. [27] 朱东明,张振,张杰,等.全髋关节置换后假体脱位危险因素的最新进展[J].中国组织工程研究,2020,36(24):5864-5870. [28] ITO H, MATSUNO T, HIRAYAMA T, et al. Health-related quality of life in patients with systemic lupus erythematosus after medium to long-term follow-up of hip arthroplasty. Lupus. 2007;16(5): 318-323. [29] ANDRIOLO L, MERLI G, Tobar C, et al. Regenerative therapies increase survivorship of avascular necrosis of the femoral head: a systematic review and meta-analysis. Int Orthop. 2018;42(7):1689-1704. [30] 黄鑫,孔渝菡,余和平.激素相关性股骨头坏死非手术治疗研究进展[J].现代医药卫生,2020, 8(36):1179-1182. |
| [1] | Wang Jianping, Zhang Xiaohui, Yu Jinwei, Wei Shaoliang, Zhang Xinmin, Xu Xingxin, Qu Haijun. Application of knee joint motion analysis in machanism based on three-dimensional image registration and coordinate transformation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(在线): 1-5. |
| [2] | Tan Xinfang, Guo Yanxing, Qin Xiaofei, Zhang Binqing, Zhao Dongliang, Pan Kunkun, Li Yuzhuo, Chen Haoyu. Effect of uniaxial fatigue exercise on patellofemoral cartilage injury in a rabbit [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(在线): 1-6. |
| [3] | Xue Yadong, Zhou Xinshe, Pei Lijia, Meng Fanyu, Li Jian, Wang Jinzi . Reconstruction of Paprosky III type acetabular defect by autogenous iliac bone block combined with titanium plate: providing a strong initial fixation for the prosthesis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1424-1428. |
| [4] | Zhuang Zhikun, Wu Rongkai, Lin Hanghui, Gong Zhibing, Zhang Qianjin, Wei Qiushi, Zhang Qingwen, Wu Zhaoke. Application of stable and enhanced lined hip joint system in total hip arthroplasty in elderly patients with femoral neck fractures complicated with hemiplegia [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1429-1433. |
| [5] | Zhang Lichuang, Xu Hao, Ma Yinghui, Xiong Mengting, Han Haihui, Bao Jiamin, Zhai Weitao, Liang Qianqian. Mechanism and prospects of regulating lymphatic reflux function in the treatment of rheumatoid arthritis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1459-1466. |
| [6] | Jing Jinpeng, Zhang Yue, Liu Xiaomin, Liu Yi. Traditional Chinese medicine injection for promoting blood circulation in prevention of deep vein thrombosis after orthopedic surgery: network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1467-1476. |
| [7] | Bai Zixing, Cao Xuhan, Sun Chengyi, Yang Yanjun, Chen Si, Wen Jianmin, Lin Xinxiao, Sun Weidong. Construction and biomechanical analysis of ankle joint finite element model in gait cycle [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1362-1366. |
| [8] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [9] | Wu Bingshuang, Wang Zhi, Tang Yi, Tang Xiaoyu, Li Qi. Anterior cruciate ligament reconstruction: from enthesis to tendon-to-bone healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1293-1298. |
| [10] | Liu Gang, Ma Chao, Wang Le, Zeng Jie, Jiao Yong, Zhao Yi, Ren Jingpei, Hu Chuanyu, Xu Lin, Mu Xiaohong. Ankle-foot orthoses improve motor function of children with cerebral palsy: a Meta-analysis based on 12 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1299-1304. |
| [11] | Wang Xinmin, Liu Fei, Xu Jie, Bai Yuxi, Lü Jian. Core decompression combined with dental pulp stem cells in the treatment of steroid-associated femoral head necrosis in rabbits [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1074-1079. |
| [12] | Li Jie, Zhang Haitao, Chen Jinlun, Ye Pengcheng, Zhang Hua, Zhou Bengen, Zhao Changqing, Sun Youqiang, Chen Jianfa, Xiang Xiaobing, Zeng Yirong. Anterior cruciate ligament rupture and patellofemoral joint stability before sagittal and axial measurement using MRI [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 969-972. |
| [13] | Xu Kuishuai, Zhang Liang, Chen Jinli, Ren Zhongkai, Zhao Xia, Li Tianyu, Yu Tengbo. Effect of force line changes on lower limb joints after medial open wedge high tibial osteotomy [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 821-826. |
| [14] | Shao Yangyang, Zhang Junxia, Jiang Meijiao, Liu Zelong, Gao Kun, Yu Shuhan. Kinematics characteristics of lower limb joints of young men running wearing knee pads [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 832-837. |
| [15] | Huang Hao, Hong Song, Wa Qingde. Finite element analysis of the effect of femoral component rotation on patellofemoral joint contact pressure in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 848-852. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||