中国组织工程研究 ›› 2013, Vol. 17 ›› Issue (48): 8419-8428.doi: 10.3969/j.issn.2095-4344.2013.48.020
• 骨与关节临床实践 clinical practice of the bone and joint • 上一篇 下一篇
同种异体骨复合自体红骨髓移植治疗关节周围骨折
孔志刚,陈永宝,孙 磊
- 河北医科大学第三医院骨伤科,河北省骨科生物力学重点实验室,河北省石家庄市 050051
-
出版日期:2013-11-26发布日期:2013-11-26 -
通讯作者:孔志刚,河北医科大学第三医院骨伤科,河北省骨科生物力学重点实验室,河北省石家庄市 050051 -
作者简介:孔志刚,男,1962年生,1984年河北医科大学毕业,教授,硕士生导师。 -
基金资助:河北省卫生厅科研基金资助项目(20090417)*
Allograft cancellous bone combined with autologous red marrow for treatment of periarticular fractures
Kong Zhi-gang, Chen Yong-bao, Sun Lei
- Department of Orthopedics, the Third Affiliated Hospital of Hebei Medical University, Hebei Orthopaedic Biomechanics Laboratory, Shijiazhuang 050051, Hebei Province, China
-
Online:2013-11-26Published:2013-11-26 -
Contact:Kong Zhi-gang, Professor, Master’s supervisor, Department of Orthopedics, the Third Affiliated Hospital of Hebei Medical University, Hebei Orthopaedic Biomechanics Laboratory, Shijiazhuang 050051, Hebei Province, China kzg2005@tom.com -
About author:Kong Zhi-gang, Professor, Master’s supervisor, Department of Orthopedics, the Third Affiliated Hospital of Hebei Medical University, Hebei Orthopaedic Biomechanics Laboratory, Shijiazhuang 050051, Hebei Province, China kzg2005@tom.com -
Supported by:the Scientific and Technological Research Program of Hebei Provincial Health Bureau, No. 20090417*
摘要:
背景:关节周围骨折复位后常出现骨缺损,需进行植骨填充骨缺损以早期支撑关节面以防止关节面塌陷及移位。同种异体骨是治疗骨缺损的移植材料,但成骨能力差。自体红骨髓有成骨能力,但同种异体骨复合自体红骨髓移植治疗关节周围骨折的临床效果有待评定。 目的:采用锁定板固定、同种异体骨复合自体红骨髓移植治疗关节周围骨折的临床效果。 方法:纳入河北医科大学第三医院骨伤科治疗关节周围骨折患者43例。采用切开解剖复位关节面、将红骨髓与同种异体骨颗粒复合体植于骨缺损处,植骨完成后常规解剖锁定板内固定。胫骨平台骨折采用内侧、外侧或双侧锁定板固定。桡骨远端骨折采用背侧或掌侧锁定板固定,胫骨远端骨折采用胫骨远端内侧或外侧板锁定内固定。 结果与结论:患者43例共随访12个月至6年,平均4.3年。X射线片及CT复查结果显示,43例患者达骨性愈合,塌陷骨折复位良好。其中新鲜骨折愈合时间2-6个月,平均4个月;陈旧骨折愈合时间3-7个月,平均5.5个月。植骨后43例患者无明显免疫排斥反应,2例患者切口渗液较多,经换药2周愈合。切口感染患者1例,经引流换药4周伤口愈合,随访4年1个月至今感染未复发。根据Mankin和Komender标准评定,同种骨移植满意患者40例,占93%;不满意患者3例,占7%。结果证实,在锁定板支撑固定下,异体松质骨与自体红骨髓复合体移植治疗周围关节骨折可以起到近期支撑作用,防止关节面塌陷及骨折移位,并为关节周围骨折骨缺损提供骨重建材料,远期可以达到骨折愈合的目的。
中图分类号:
引用本文
孔志刚,陈永宝,孙 磊. 同种异体骨复合自体红骨髓移植治疗关节周围骨折[J]. 中国组织工程研究, 2013, 17(48): 8419-8428.
Kong Zhi-gang, Chen Yong-bao, Sun Lei. Allograft cancellous bone combined with autologous red marrow for treatment of periarticular fractures[J]. Chinese Journal of Tissue Engineering Research, 2013, 17(48): 8419-8428.
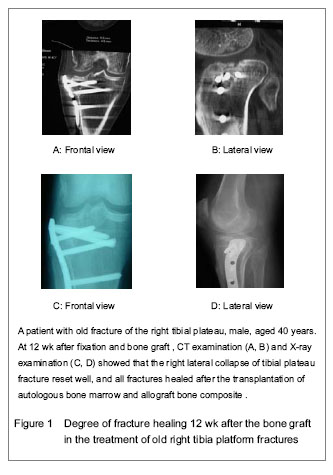
Evaluation criteria of X-ray radiography for bone fusion between the graft and the host bone[12]: the bone graft and the host bone get fused well, which is defined as fracture healing; the bone graft and the host bone are not fused, which is defined as nonunion; the transplant bone is absorbed > 30%, which is defined as transplanted bone resorption; the bone mineral density around the transplantation bone decreases, which is defined as osteoporosis; the bone mineral density around the transplantation bone increases, which is defined as osteosclerosis. Results found that the fresh fracture healing time was 2-6 months, an average of 4 months; the old fracture healing time was 3 to 7 months, an average of 5.5 months.
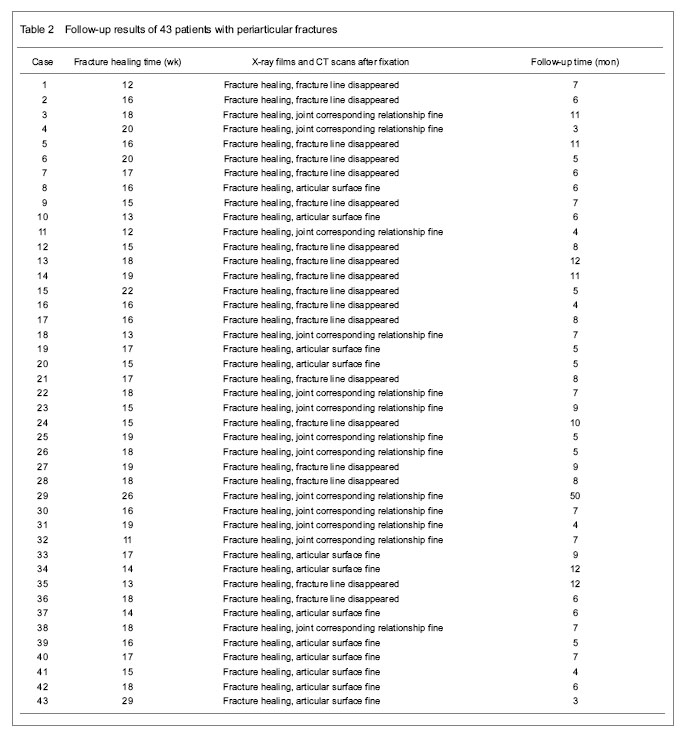
According to the scoring criteria of the result of allograft taken by Mankin[13] and Komender[14], the results were classified as: (1) Satisfaction: incision is healed well after fixation; presence of transient fever and a small amount of effusion; X-ray shows no absorption of graft bone; fracture is completely healed; no tumor recurrence; limb local strength and function return to normal or mildly limited, no pain, normal daily activities recover without complications. (2) Dissatisfaction: apparent rejection, a large number of effusion, wound delayed union or fistula formation; X-ray shows all bone graft absorbed ahead of time; local pain, limited daily activities; complications such as infection and nonunion, or tumor recurrence, bone graft taken out, even amputation. Finally, according to the results of 43 patients, 40 cases were satisfied with the bone allograft, accounted for 93%; three cases were not satisfied, accounting for 7%.
| [1] Rimondini L, Nicoli-Aldini N, Fini M, et al. In vivo experimental study on bone regeneration in critical bone defects using an injectable biode-gradable PLA/PGA copolymer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99(2):148-154. [2] Kon E, Muraglia A, Corsi A, et al. Autologus bone marrow stromal, cells loaded onto porous hydroxyapatite ceramic accelerate bone repair in critical-size defects of sheep long bones. J Biomed Mater Res. 2000;49(3):328-337. [3] Zasacki W. The efficacy of application of lyophilized, radiation sterilized bone graft in orthopaedic surgery. Clin Orthop Relat Res. 1991;272:82-87. [4] Zhang L, Xu ZH, Yang ZL. Transplantation combined with autologous bone marrow to repair non-infected nonunion. Zhongguo Xiufu Chongjia Waike Zazhi. 2005;19(7):590-591. [5] Hernigou P, Poignard A, Manicom O, et al. The use of percutaneous autologous bone marrow transplantation in nonunion and avascular necrosis of bone. J Bone Joint Surg (Br). 2005;87(7):896-902. [6] Burwell RG. The function of bone marrow in the corporation of a bone graft. Clin Orthop Relat Res. 1985;200(2):125-141. [7] Burwell RG. Studies in transplantation of bone. Clin Orthop Relat Res. 1999;(367 Suppl):S5-11;discussion S2-4. [8] Zhao JJ, Li QZ. The preparation of the grafting material of homologous cancellus/autologous red marrow and clinical applicarion. Shiyong Guke Zazhi. 2005(2):123-125. [9] Kong ZG, Tian DH. Treatment of traumatic bone defect with graft material of allogenic cancellus combined with autologous red marrow. Zhongguo Xiufu Chongjia Waike Zazhi. 2008;(10):1251-1254. [10] Yin WF, Chen S. Allogeneic bone combined with autologous concentrated red bone marrow graft for treatment of benign bone tumors and tumor-like lesions. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2009;16(24):3149-3152. [11] Sudkamp N, Bayer J, Hepp P, et al. Open reduction and internal fixation of proximal humeral fractures with use ofthe locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Joint Surg (Am). 2009;91(6):1320-1328. [12] Andersen JR, Detlie T, Griffiths HJ. The radiology of bone allografts. Radiol Clin North Am. 1995;33(2):391-400. [13] Mankin HJ, Gebhardt MC, Tomford WW. The use of frozen cadaveric allografts in the management of patients with bone Tumors of the extremities. Orthop Clin North Am. 1987;18(2):275-289. [14] Komender J, Malczewska H, Komender A. Therapeutic effects of transplantation of lyophilized and radiation- sterilized, allogeneic bone. Clin Orthop Relat Res. 1991; (272):38-49. [15] Huang JJ, Zhang JM, Zhuo XL, et al. Treatment of senile Colles fracture with anatomic locking plate combined with allogeneic bone transplantation. Zhongguo Gu yu Guanjie Sunshang Zazhi. 2011;26(1):78-79. [16] Bennett WF, Browner B. Tibial plateau fractures: a study of associated soft tissue injuries. J OrthopTrauma. 1994;8(3): 183-185. [17] Feng W, Fu L, Liu JG. Bone allograft for tibial plateau fractures in 22 cases. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2009;13(15):2984-2987. [18] Cao Y, Yuan ZM, Yan P, et al. Characteristics of nano-artificial bone grafr in treatment of tibial plateau fracture. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2011;15(38):7189-7192. [19] Laurencin C, Khan Y, El-Amin SF. Bone graft substitutes. Expert Rev Med Deviecs. 2006;3(1):49-57. [20] Wraighte PJ, Howard PW. Femoral impaction bone allografting with an Exeter cemented collarless, polished, tapered stem in revision hip replacement: a mean follow-up of 10.5 years. J Bone Joint Surg (Br). 2008;90(8): 1000-1004. [21] De Long WG Jr, Einhorn TA, Koval K, et al. Bone grafts and bone graft substitutes in orthopaedic trauma surgery. J Bone Joint Surg (Am). 2007;89(3):649-658. [22] Jerosch J, Muchow H, Clahsen H. Stability of human bone cortex following various preservation and sterilization methods. Z Orthop Ihre Grenzgeb. 1991;129(4):295-301. [23] Wang ZQ, Wang Q, Su LX, et al. Clinical application of morselized allogeneic bone processed by lyophilization and radiation. Zhonghua Guke Zazhi. 2004;24(10):590-596. [24] Song HP, Wang ZQ. Study on the application of allogeneic bone transplantation. Zhongguo Xiufu Chongjia Waike Zazhi. 2006;20(1):77-80. [25] Xu ST. Practical Orthopedics. 2nd ed. Beijing: People’s Medical Publishing House. 2002. [26] Hernigou P, Poignard A, Beaujean F, et al. Percutaneous autologous bone-marrow grafting for nonunions. In uence of the number and concentra-tion of progenitor cells. J Bone Joint Surg (Am). 2005;87(7):1430-1437. [27] Yang GS, Xu YB. Bone mesenchymal stem cells and their utilization advances. Zhonghua Chuangshang Guke Zazhi. 2004;6(7):824-827. [28] Gu ZC, Li QH. An experimental study on the marrow stromal cells and biomaterial composites in repair of segmental defects of rabbit ulna. Zhonghua Chuangshang Guke Zazhi. 2004;6(6):651-656. [29] Cao JT, Li QJ, Song HP, et al. Study of the biocompatibility on allogeneic freeze-dried bone particles and bone marrow stromal cells-derived osteoblasts in vitro. Zhongguo Jiaoxing Waike Zazhi. 2010;18(12):1023-1026. [30] Fu M, Liang HX. Treatment of bone defect bone allograft with bone marrow stem cell in animal experiment. Zhongshan Daxue Xuebao (Medical Sciences). 2007;28(5): 515-519. [31] Zhang SQ, Liu AQ, Xiao DM, et al. Unicameral bone cysts treated by percutaneous injection of autologous bone marrow and allogeneic bone powder grafting. Zhongguo Guzhongliu Gubing. 2006;5(5):273-275. [32] Li B, Chen J, Que XY, et al. Massive bone allograft combined with autologous bone marrow transplantation for proximal femoral defects resulting from tumor resection. Zhongguo Zuzhi Gongcheng Yanjiu. 2012;16(5):831-834. [33] Lin JP, Song SF, Li ZM, et al. Treatment of bone defects with autologous bone marrow transplantation combined with bone allograft. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2011;15(26):4891-4894. [34] Wei JR, Zhang Y, Lin YL, et al. Xenogeneic cancellous bone for repairing segmental defects in rabbit radius. Zhongguo Zuzhi Gongcheng Yanjiu. 2012;16(29):5379- 5381. [35] Fang ZH, Tan JH, Zeng XT, et al. Effect of bone marrow mesenchymal stem cells combined with various scaffold materials: a systematic review. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2011;49(15): 9249-9253. [36] Yi HC, Tang LH, Zhang XP. Experimental study on bone defected by combined autologous bone marrow transplantation, cut-tebone, and sodium hyaluronate. Zhongguo Zhongxiyi Jiehe Zazhi. 2011;31(8):1122-1126. [37] State Council of the People’s Republic of China. Administrative Regulations on Medical Institution. 1994-09-01. |
| [1] | 崔可赜, 郭 祥, 韩贵斌, 陈元良, 刘亦恒, 钟海波. MAKO机器人辅助后外侧入路全髋关节置换的学习曲线及临床早期效果[J]. 中国组织工程研究, 2020, 24(9): 1313-1317. |
| [2] | 米尔阿里木•木尔提扎, 赵 巍, 瓦热斯江•尼牙孜, 袁 宏, 王 利. 直接前侧入路与前外侧入路全髋关节置换的差异:基于置换后早期患者主观感受的比较[J]. 中国组织工程研究, 2020, 24(9): 1318-1323. |
| [3] | 赵维彪, 何子微, 李 季, 李 毅. 3D打印导板在以SuperPATH技术行老年髋关节置换中的应用价值:回顾性研究和文献检索证据分析[J]. 中国组织工程研究, 2020, 24(9): 1324-1330. |
| [4] | 尹健东, 王鑫灵, 左 彪, 李秾杙. 全膝关节置换过程中挤压驱血和抬腿驱血与置换后并发症的关系[J]. 中国组织工程研究, 2020, 24(9): 1331-1336. |
| [5] | 周 祺, 高 益, 魏 康, 黎 俊, 徐建达, 蒋 阳, 瞿玉兴. 全膝关节置换治疗类风湿关节炎:关节功能及相关生化指标的变化[J]. 中国组织工程研究, 2020, 24(9): 1337-1341. |
| [6] | 余 彬, 彭银虓, 薛 力, 秦 辉, 梁益建. 零切迹椎间融合固定器与传统颈前路钢板Cage融合内固定治疗双节段颈椎病的比较[J]. 中国组织工程研究, 2020, 24(9): 1342-1347. |
| [7] | 张志伟, 李 利, 黄兹谕, 吴多艺, 甘发荣, 叶宝飞, 张 岩, 张泰标, 胡万钧. 单、双侧椎弓根入路及单侧椎弓根外入路椎体成形治疗胸腰段椎体压缩性骨折:骨水泥灌注量与渗漏率[J]. 中国组织工程研究, 2020, 24(9): 1353-1358. |
| [8] | 刘 炎, 葛鸿庆, 管 华, 陈文治. 内侧柱缺失型肱骨近端骨折不同固定方式的有限元分析[J]. 中国组织工程研究, 2020, 24(9): 1384-1389. |
| [9] | 林 旺, 王盈盈, 林伟民, 许胜贵, 黄其龙, 郭卫中, 林成寿. 新型胸锁关节钩状板的研发与生物力学测定[J]. 中国组织工程研究, 2020, 24(9): 1395-1399. |
| [10] | 何晓宇, 王朝强, 周之平, 张中宁, 赖草生, 阮康明, 李雪丽, 赵德伟. 三维有限元方法构建足部健康骨骼与常见疾病模型及生物力学分析[J]. 中国组织工程研究, 2020, 24(9): 1410-1415. |
| [11] | 钟远鸣, 罗 满, 唐福波, 唐 成. 骨质疏松性胸腰椎骨折MRI STIR黑色线性信号与外力程度的关系[J]. 中国组织工程研究, 2020, 24(9): 1400-1404. |
| [12] | 邓必勇, 邓必祥. 髋关节置换髋臼相关参数在CT水平面与CT真骨盆平面上的差异[J]. 中国组织工程研究, 2020, 24(9): 1405-1409. |
| [13] | 赵燕旭, 张 钊, 罗 东, 李芒来, 汪 靖, 方 杰, 蒋 雯, 冯 勇, 彭 江, 许文静, 王 玉, 汪爱媛, 张民泽. 下肢应力性骨折相关风险因素及未来的研究方向[J]. 中国组织工程研究, 2020, 24(9): 1422-1429. |
| [14] | 颜 威, 蒋 涛, 吴昌桂, 孔 博, 奚小冰. 桡骨远端骨折固定夹板外观、材质、固定带等研究的新进展[J]. 中国组织工程研究, 2020, 24(9): 1430-1434. |
| [15] | 赵春涛, 卿明松, 余浪波, 彭笳宸. 运动学对线和机械力学对线指导全膝关节置换效果的Meta分析[J]. 中国组织工程研究, 2020, 24(9): 1435-1442. |
Totally 43 patients included 25 males and 18 females, aged 19-68 years with an average of 40 years. There were 18 cases of tibial plateau fractures, 17 cases of distal radius fractures, and eight cases of distal tibial fractures. Of all the 43 cases, 22 cases were confirmed as having fresh fractures, and 21 as having old fractures. Time from fresh fractures to surgery after injury was 5-12 days, an average of 8 days. Time from old fractures to surgery after injury was 1-5.5 months, an average of 2.5 months (Table 1).
.jpg)
Temperature change after the bone graft; seepage and infection of incision, immunological rejection, fracture healing, fusion level of bone graft with the host bone.
1 同种异体骨是治疗骨缺损的移植材料,但成骨能力差。自体红骨髓有成骨能力,同种异体骨复合自体红骨髓移植治疗关节周围骨折的临床效果有待评定。 2 实验应用锁定加压板固定、异体松质骨颗粒复合自体红骨髓移植治疗关节周围骨折患者43例,结果证实,在锁定板支撑固定下,异体松质骨与自体红骨髓复合体移植治疗周围关节骨折可以起到近期支撑作用,防止关节面塌陷及骨折移位。为关节周围骨折骨缺损提供骨重建材料,远期可以达到骨折愈合的目的。 基金资助: 河北省卫生厅科研基金资助项目(20090417)*
有研究表明,锁定加压钢板经临床多中心研究证明具有明显优势。锁定螺钉成角固定在骨质疏松和粉碎骨折中具有较好的抗拉力和锚合力,防止内固定物松动。同种异体骨作为骨髓的载体,并具有组织相容性好。以小块松质骨作为载体复合骨髓制成复合植骨材料。充分利用骨髓这种活跃的成骨能力,正好补充了单纯异体骨植骨成骨能力的不足。同种异体松质骨复合自体红骨髓移植充填骨缺损,利用同种异体松质骨与自体骨相当支撑力以期早期进行关节功能锻炼。利用骨髓这种活跃的成骨能力尽早实现骨缺损的重建。这种充填材料具有骨传导,骨诱导及成骨作用。以异体松质骨颗粒复合自体红骨髓移植充填骨缺损在关节关节周围骨折骨的效果是大家关注的问题。实验应用锁定加压板固定、异体松质骨颗粒复合自体红骨髓移植治疗关节周围骨折患者43例,效果满意。
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||