Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (15): 3810-3819.doi: 10.12307/2026.151
Previous Articles Next Articles
Biomechanical finite element analysis of lumbar degeneration based on radiological imaging
Gao Sheng1, Xin Shimin2, Liu Xingquan1, Kang Liqing3, Ren Baolin1, Wang Haiyan4
- ¹Department of Medical Imaging, Hohhot Hospital of Traditional Chinese and Mongolian Medicine, Hohhot 010000, Inner Mongolia Autonomous Region, China; ²Department of Health and Medical Sciences, Qitaihe Vocational College, Qitaihe 154600, Heilongjiang Province, China; 3Sterilization Supply Center, the Fourth Hospital of Inner Mongolia Autonomous Region, Hohhot 010000, Inner Mongolia Autonomous Region, China; 4Department of Anatomy, School of Basic Medical Sciences, Inner Mongolia Medical University, Hohhot 010110, Inner Mongolia Autonomous Region, China
-
Accepted:2025-03-24Online:2026-05-28Published:2025-11-05 -
Contact:Wang Haiyan, MS, Professor, Master’s supervisor, Department of Anatomy, School of Basic Medical Sciences, Inner Mongolia Medical University, Hohhot 010110, Inner Mongolia Autonomous Region, China -
About author:高升,男,1975年生,内蒙古自治区呼和浩特市人,汉族,硕士,主要从事医学影像的研究。 并列第一作者:辛世民,男,1994年生,黑龙江省鸡西市人,汉族,主要从事肌骨康复的研究。 -
Supported by:Inner Mongolia Autonomous Region Higher Education Innovation Team Development Plan, No. NMGIRT2419 (to WHY); 2022 Inner Mongolia Autonomous Region Health Science and Technology Plan, No. 202201188 (to WHY)
CLC Number:
Cite this article
Gao Sheng, Xin Shimin, Liu Xingquan, Kang Liqing, Ren Baolin, Wang Haiyan. Biomechanical finite element analysis of lumbar degeneration based on radiological imaging[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(15): 3810-3819.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

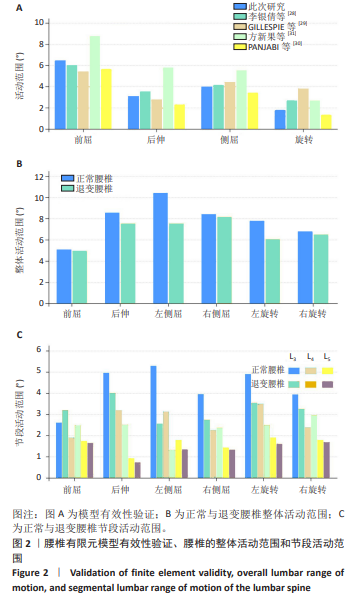
2.1 整体活动范围与节段活动范围 在10 Nm纯力矩下,屈伸、轴向旋转和横向弯曲的活动范围与已发表的结果进行了验证(图2A)。与国内外参考文献保持高度一致,达到模型的有效性[27-30]。 整体活动范围:前屈时,正常腰椎的活动度为5.10°,退变腰椎为4.97°,前屈活动度在退变过程中下降。后伸时,正常腰椎为8.59°,退变腰椎为7.56°,显示出后伸能力下降。左侧屈和右侧屈时,正常腰椎的左侧屈和右侧屈分别为10.44°和8.43°,而退变腰椎的分别为7.56°和8.19°,表明退变腰椎的侧屈活动度下降,尤其是左侧屈。左旋转和右旋转时,正常腰椎为7.80°和6.80°,退变腰椎分别为6.09°和6.52°,显示出旋转活动度的整体下降(图2B)。综合来看,腰椎退变导致其整体活动度模式发生改变,不同方向活动度均出现不同程度的下降,这反映了腰椎退变对其运动功能的影响。 节段活动范围:在前屈时,退变L3节段(3.20°)较正常L3节段(2.62°)有略微增加;但在后伸和侧屈时,退变L3节段的活动度大幅下降,尤其是左侧屈(从5.29°降至2.57°),这是因为退变导致 L3 节段的椎间盘高度降低、小关节骨质增生,使得后伸和侧屈时关节活动受限。L4节段的活动度在退变后普遍下降,尤其是左侧屈(从3.14°降至1.33°),L4在退变过程中的活动度受限最为明显。L4作为承受较大负荷的椎体,其退变导致运动范围大幅减小,进一步限制脊柱功能。L4 作为承受较大负荷的椎体,退变时椎间盘的退变、椎体终板的损伤等会导致椎体间稳定性下降,周围肌肉和韧带为了维持脊柱的稳定会限制其活动,从而导致运动范围大幅减小,进一步限制脊柱功能。L5节段在退变过程中前屈、后伸变化不大,但在侧屈和旋转的活动度方面有所下降,尤其是右旋转(从1.80°降至1.69°)。L5的功能变化相对较小,可能是因为其活动度本身较小,退变对其影响不如L4和L3显著(图2C)。L5的功能变化相对较小,可能是因为其活动度本身较小,周围有较强的肌肉和韧带附着提供一定的稳定性,所以退变对其影响不如L4和L3显著。"

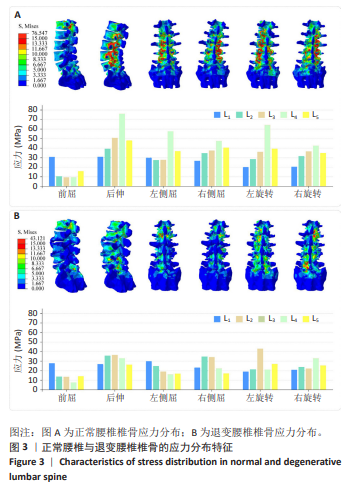
2.2 椎骨应力分布 在正常腰椎中,L1-5在前屈、后伸、侧屈和旋转方向的应力值呈现一定的规律性变化。例如,L4在后伸方向应力达到最大值76.02 MPa,而L1的前屈应力值最高为30.81 MPa;与其他节段相比,L3的应力在旋转运动时(36.03 MPa和36.60 MPa)相对较高,该节段在旋转活动中更易受到应力集中。L4的应力值在后伸和侧屈时明显高于其他节段,尤其是在后伸时达到76.02 MPa,提示L4节段在正常生理活动中承受较大的力学负荷,可能成为应力集中的高风险区域。应力云图显示,应力主要集中在小关节与峡部位置;前屈时,椎骨应力相对小且主要集中在L1位置,其余工况下,应力集中主要集中在L3-5节段(图3A)。 在退变腰椎中,应力值总体下降,总体而言,退变腰椎的应力值呈现普遍下降趋势,尤其是在L4和L5节段。L4在左侧屈时应力从正常的57.60 MPa降至16.07 MPa,L5的右旋转应力从34.83 MPa降至25.42 MPa。L3节段在退变状态下应力集中,L3左旋转应力为43.12 MPa,显著高于正常状态的36.03 MPa,表明退变腰椎中L3节段在旋转运动中的力学负担加重。此外,退变腰椎的应力分布模式发生了明显改变:在侧屈载荷下,应力集中区域向头侧迁移;而在旋转载荷下,应力集中区域则向尾侧迁移至L4和L5节段(图3B)。这些变化提示腰椎退变可能导致力学负荷的重新分布,进而影响脊柱的整体生物力学行为。"

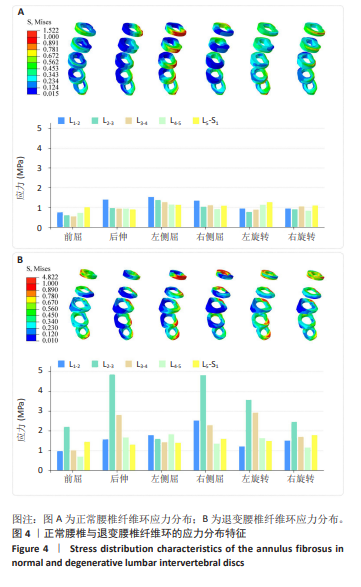
2.3 纤维环应力分布 在正常腰椎模型中,纤维环的应力分布呈现与运动模式密切相关的节段特异性(图4A)。前屈载荷下,纤维环应力从L1-2节段的0.74 MPa呈梯度上升趋势至L5-S1节段的1.00 MPa,表明L5-S1节段在此工况下承受最大的拉伸应力。后伸载荷中,应力分布呈现反向特征,L1-2节段应力峰值达1.39 MPa,显著高于L5-S1节段的0.89 MPa。侧屈与旋转载荷下,各节段应力分布相对均匀,但L5-S1节段在旋转运动中的应力增幅显著。L5-S1节段在侧屈与旋转运动中亦表现出区域性高应力分布,提示该节段在复合载荷下可能成为退变的初始位点。 腰椎退变模型的纤维环应力分布模式发生显著重构(图4B),尤其是邻近节段(L2-3与L3-4),L2-3节段异常负荷:该节段在后伸与右侧屈载荷下分别达到4.85 MPa与4.82 MPa的应力峰值,显著高于其他节段。L3-4节段在左旋载荷下的应力值升至2.92 MPa,而L4-5节段在左侧屈时应力达1.82 MPa,提示退变导致力学负荷向头尾端节段转移。与正常模型相比,退变腰椎的应力集中区域呈现动态迁移特征——侧屈时向头侧偏移至L2-3,旋转时则向尾侧扩展至L4-5。特别值得注意的是,L2-3节段在后伸载荷下不仅出现全域性应力集中(4.85 MPa),其应力分布梯度亦显著陡峭化,表明该节段可能成为退变进程中的力学薄弱点,邻近节段受到较大影响。此外,L3-4节段在左旋载荷下的高应力区与椎间盘造影证实的退变区域高度吻合。"

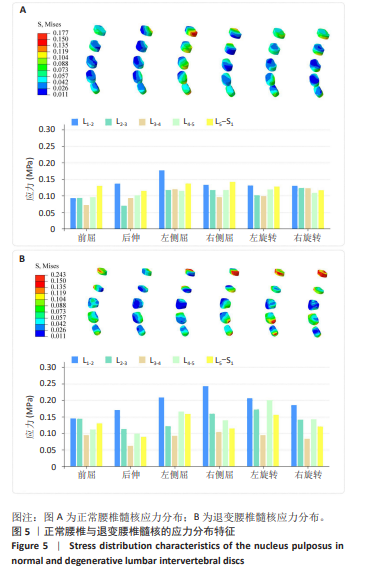
2.4 髓核应力分布 在正常腰椎中,各节段髓核应力在不同运动方向下的变化较为稳定。L1-2节段的应力在各运动方向下均较为稳定,前屈时应力为0.09 MPa,后伸时为0.14 MPa,而左右旋转应力均为0.13 MPa。L5-S1节段则表现出稍高的应力值,尤其在前屈和后伸时,分别为0.13 MPa和0.12 MPa。各节段的应力分布较为均匀,前屈和后伸的应力普遍较低,侧屈和旋转的应力适中。应力云图也显示了稳定的变化(图5A)。这表明在正常腰椎中,髓核承受的压力较为分散且均匀。 在腰椎退变状态下,髓核应力显著增加。L1-2节段的应力显著增加,前屈时应力达到0.15 MPa,后伸时为0.17 MPa,左侧屈应力为0.21 MPa,右侧屈则升至0.24 MPa,左右旋转时的应力分别为0.21 MPa和0.19 MPa。相比正常状态,退变髓核在侧屈和旋转运动中的应力大幅增加,这是由于椎间盘退变导致的髓核和纤维环之间的力学失衡,髓核的负载分布不再均匀,局部应力显著增加。L2-3节段前屈应力为0.14 MPa,后伸时的应力大幅上升至0.11 MPa,左侧屈和右侧屈时的应力分别为0.12 MPa和0.16 MPa,尤其是在左旋转时应力升至0.17 MPa,远高于正常状态下的应力水平。这种变化反映出退变腰椎的各节段在运动过程中会出现力学失衡,特别是在旋转和侧屈等运动中,椎间盘的负担加剧,从而导致髓核应力升高。L4-5作为负荷较大的节段,在退变状态下表现出应力集中现象,前屈时应力为0.11 MPa,后伸为0.10 MPa;侧屈运动中的应力显著增加,左侧屈时应力达到0.17 MPa,右侧屈应力为0.14 MPa;在旋转运动中,左旋转时应力升至 0.20 MPa,右旋转时为0.14 MPa。这表明退变腰椎在运动负载下的应力集中的问题更加突出,尤其是在L4-5和L5-S1节段,进一步加剧了这些区域的生物力学负担。L5-S1节段作为腰椎底部的承压区域,在退变状态下的应力变化较为显著,前屈应力为0.13 MPa, 后伸应力降低至0.09 MPa;但在侧屈和旋转运动中应力增加,左侧屈应力为0.16 MPa,右侧屈应力为0.11 MPa;此外,左右旋转时应力值分别为0.16 MPa和0.12 MPa。在右侧屈、左右旋转时,L4-5、L5-S1节段髓核后角出现明显的应力集中点,且与正常腰椎相比,应力范围扩大(图5B)。这些变化显示L5-S1节段的髓核在退变状态下承受了更多的负荷,这可能与腰椎底部作为承压区域的特殊位置有关。尤其在退变过程中,髓核的应力过于集中,可能会导致进一步的损伤和病变。"

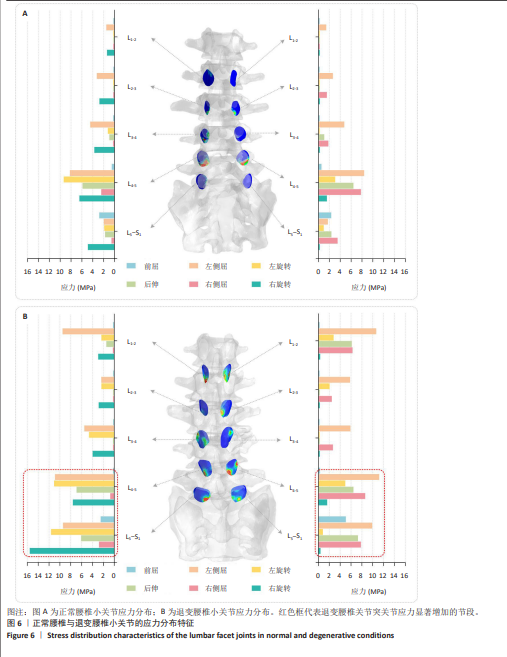
2.5 小关节应力分布 在前屈时,正常腰椎的小关节应力相对较低,L1-2至L4-5节段的应力分布均匀,最大应力出现在L5-S1节段(左侧2.81 MPa,右侧2.34 MPa),这表明正常腰椎显示出较为稳定的应力传递路径。相比之下,退变腰椎在前屈时应力显著增加,尤其在L5-S1节段(左侧2.49 MPa,右侧5.04 MPa),应力集中更为明显;在后伸时,正常腰椎小关节的应力值大幅增加,尤其是L4-5节段(左侧8.20 MPa,右侧8.39 MPa),小关节承受的负荷较大。退变腰椎小关节应力分布异常显著,L1-2节段应力值大幅提升(左侧9.50 MPa,右侧10.63 MPa),后伸时易产生应力集中明显。在侧屈运动中,正常腰椎的小关节应力相对对称,L4-5节段的应力较高(左侧9.34 MPa,右侧6.42 MPa),显示出较好的力学分布;而退变腰椎在左右侧屈时应力不对称,尤其是在L5-S1节段,右侧屈时应力值达到最大(左侧11.62 MPa,右侧7.28 MPa)。在旋转运动中,正常腰椎的小关节应力较为平均,L4-5节段左右旋转时应力集中(左旋转7.80 MPa,右旋转6.45 MPa);相比之下,退变腰椎在旋转运动时应力显著增大,尤其是在L5-S1节段(右旋转时应力高达15.53 MPa),旋转运动对退变节段的应力负荷较大(图6)。这一现象提示随着退变的进展,脊柱的力学负荷从椎间盘转移到小关节,进一步加剧了小关节负担和可能的损伤。"
| [1] PYE SR, REID DM, LUNT M, et al. Lumbar disc degeneration: association between osteophytes, end-plate sclerosis and disc space narrowing. Ann Rheum Dis. 2007;66(3):330-333. [2] JUNGHANNS H, GEORG S. The human spine in health and disease. New York: Grune & Stratton, 1971:xi, 504-xi, 504. [3] PRANEATPOLGRANG S, DAS S, NAVIC P, et al. Age-related changes in the vertebral osteophytes: a review. Int Med J. 2020;27(2):181-184. [4] CHANAPA P, YOSHIYUKI T, MAHAKKANUKRAUH P. Distribution and length of osteophytes in the lumbar vertebrae and risk of rupture of abdominal aortic aneurysms: a study of dry bones from Chiang Mai, Thailand. Anat Cell Biol. 2014;47(3):157-161. [5] KASAI Y, KAWAKITA E, SAKAKIBARA T, et al. Direction of the formation of anterior lumbar vertebral osteophytes. BMC Musculoskelet Disord. 2009;10(4):1-6 [6] KETTLER A, ROHLMANN F, RING C, et al. Do early stages of lumbar intervertebral disc degeneration really cause instability? Evaluation of an in vitro database. Eur Spine J. 2011;20(4):578-584. [7] FUJIWARA A, LIM TH, HOWARD S, et al. The Effect of Disc Degeneration and Facet Joint Osteoarthritis on the Segmental Flexibility of the Lumbar Spine. Spine. 2000;25(23):3036-3044. [8] FUJIWARA A, TAMAI K, HOWARD S, et al. The Relationship Between Disc Degeneration, Facet Joint Osteoarthritis, and Stability of the Degenerative Lumbar Spine. J Spinal Disord Tech. 2000;13(5):444-450. [9] HICKS GE, MORONE N, WEINER DK. Degenerative Lumbar Disc and Facet Disease in Older Adults. Spine. 2009;34(12): 1301-1306. [10] JOHANSSON MS, JENSEN STOCHKENDAHL M, HARTVIGSEN J, et al. Incidence and prognosis of mid-back pain in the general population: A systematic review. Eur J Pain. 201;21(1):20-28. [11] HOMMINGA J, LEHR AM, MEIJER GJ, et al. Posteriorly directed shear loads and disc degeneration affect the torsional stiffness of spinal motion segments: a biomechanical modeling study. Spine (Phila Pa 1976). 2013;38(21):E1313-1319. [12] ZHANG XY, HAN Y. Comparison of the biomechanical effects of lumbar disc degeneration on normal patients and osteoporotic patients: A finite element analysis. Med Eng Phys. 2023;112:103952. [13] PARK JS, GOH TS, LEE JS, et al. Analyzing isolated degeneration of lumbar facet joints: implications for degenerative instability and lumbar biomechanics using finite element analysis. Front Bioeng Biotechnol. 2024;12:1294658. [14] WANG H, LI N, HUANG H, et al. Biomechanical effect of intervertebral disc degeneration on the lower lumbar spine, Comput Methods Biomech Biomed Engin. 2023;26(14):1669-1677. [15] ROHLMANN A, ZANDER T, SCHMIDT H, et al. Analysis of the influence of disc degeneration on the mechanical behaviour of a lumbar motion segment using the finite element method. J Biomech. 2006;39(13): 2484-2490. [16] LITTLE JP, ADAM CJ, EVANS JH, et al. Nonlinear finite element analysis of anular lesions in the L4/5 intervertebral disc. J Biomech. 2007; 40(12):2744-2751. [17] KEAVENY TM, BUCKLEY JM. Biomechanics of Vertebral Bone. Spine Technol Handbook. 2006:63-98. [18] GALBUSERA F, SCHMIDT H, NEIDLINGER-WILKE C, et al. The mechanical response of the lumbar spine to different combinations of disc degenerative changes investigated using randomized poroelastic finite element models. Eur Spine J. 2011;20(4):563-571. [19] DU CF, CAI XY, GUI W, et al. Does oblique lumbar interbody fusion promote adjacent degeneration in degenerative disc disease: A finite element analysis, Comput Biol Med. 2021;128:104122. [20] SONG C, CHANG H, ZHANG D, et al. Biomechanical Evaluation of Oblique Lumbar Interbody Fusion with Various Fixation Options: A Finite Element Analysis. Orthop Surg. 2021;13(2):517-529. [21] CAI XY, SUN MS, HUANG YP, et al. Biomechanical effect of L4–L5 intervertebral disc degeneration on the lower lumbar spine: a finite element study. Orthop Surg. 2020;12(3):917-930. [22] MENGONI M. Biomechanical modelling of the facet joints: a review of methods and validation processes in finite element analysis. Biomech Model Mechanobiol. 2021;20(2):389-401. [23] RENNER SM, NATARAJAN RN, PATWARDHAN AG, et al. Novel model to analyze the effect of a large compressive follower pre-load on range of motions in a lumbar spine. J Biomech. 2007;40(6):1326-1332. [24] ZHU R, NIU WX, WANG ZP, et al. The Effect of Muscle Direction on the Predictions of Finite Element Model of Human Lumbar Spine. Biomed Res Int. 2018;2018:4517471. [25] BELAID D, VENDEUVRE T, BOUCHOUCHA A, et al. Utility of cement injection to stabilize split-depression tibial plateau fracture by minimally invasive methods: A finite element analysis. Clin Biomech (Bristol, Avon). 2018;56:27-35. [26] DEHOUST J, MÜNCH M, SEIDE K, et al. Biomechanical aspects of the posteromedial split in bicondylar tibial plateau fractures-a finite-element investigation. Eur J Trauma Emerg Surg. 2020;46(6): 1257-1266. [27] 李银倩,吕杰,丁立军,等.韧带损伤影响腰椎稳定性的生物力学特征[J].中国组织工程研究,2024,28(21):3286-3292. [28] GILLESPIE KA, DICKEY JP. Biomechanical role of lumbar spine ligaments in flexion and extension: determination using a parallel linkage robot and a porcine model. Spine (Phila Pa 1976). 2004;29(11):1208-1216. [29] PANJABI MM, GOEL VK, TAKATA K. Physiologic strains in the lumbar spinal ligaments. An in vitro biomechanical study 1981 Volvo Award in Biomechanics. Spine (Phila Pa 1976). 1982;7(3):192-203. [30] 方新果, 赵改平, 王晨曦, 等. 基于CT图像腰椎L4L5节段有限元模型建立与分析[J]. 中国生物医学工程学报,2014,33(4):487-492. [31] PARK WM, KIM K, KIM YH. Effects of degenerated intervertebral discs on intersegmental rotations, intradiscal pressures, and facet joint forces of the whole lumbar spine. Comput Biol Med. 2013;43(9):1234-1240. [32] RUBERTÉ LM, NATARAJAN RN, ANDERSSON GB. Influence of single-level lumbar degenerative disc disease on the behavior of the adjacent segments--a finite element model study. J Biomech. 2009; 42(3):341-348. [33] 赵亮,闫广华,瞿东滨,等.腰椎间盘退变对软骨终板生物力学特性影响的有限元分析[J]. 中国临床解剖学杂志,2015,33(4): 455-460. [34] QIN DP, ZHANG XG, SON M, et al. Effect of different attributes of the mimic human lumbar spine biomechanics material structure change by finite element analysis. SN Appl Sci. 2021;3(12):880. [35] WANG K, JIANG C, WANG L, et al. The biomechanical influence of anterior vertebral body osteophytes on the lumbar spine: A finite element study. Spine J. 2018;18(12):2288-2296. [36] SCHMIDT H, KETTLER A, ROHLMANN A, et al. The risk of disc prolapses with complex loading in different degrees of disc degeneration - a finite element analysis. Clin Biomech (Bristol, Avon). 2007;22(9):988-998. [37] MIMURA M, PANJABI MM, OXLAND TR, et al. Disc degeneration affects the multidirectional flexibility of the lumbar spine. Spine (Phila Pa 1976). 1994;19(12):1371-1380. [38] FELSON DT, NEOGI T. Osteoarthritis: is it a disease of cartilage or of bone? Arthritis Rheum. 2004;50(2):341-344. [39] IBARZ E, MAS Y, MATEO J, et al. Instability of the lumbar spine due to disc degeneration. A finite element simulation. Adv Biosci Biotechnol. 2013;4(4):548-556. [40] 刘珍珍,陈建宇,钟镜联,等. 腰椎间盘退变MRI:与Modic改变相关的影像学分析[J]. 中国组织工程研究,2012,16(52):9737-9743. [41] 文王强,徐浩翔,张泽佩,等. 腰椎小关节退变的相关因素及生物力学特点[J]. 中国组织工程研究,2020,24(24):3883-3889. [42] WANG YXJ, DENG M, HE LC, et al. Osteoporotic vertebral endplate and cortex fractures: A pictorial review. J Orthop Translat. 2018;15: 35-49. [43] WILKE HJ, ROHLMANN F, NEIDLINGER-WILKE C, et al. Validity and interobserver agreement of a new radiographic grading system for intervertebral disc degeneration: Part I. Lumbar spine. Eur Spine J. 2006;15(6):720-730. [44] ADAMS MA, ROUGHLEY PJ. What is intervertebral disc degeneration, and what causes it? Spine (Phila Pa 1976). 2006;31(18):2151-2161. [45] LUOMA K, RIIHIMÄKI H, LUUKKONEN R, et al. Low back pain in relation to lumbar disc degeneration. Spine (Phila Pa 1976). 2000;25(4): 487-492. |
| [1] | Liu Wenlong, Dong Lei, Xiao Zhengzheng, Nie Yu. Finite element analysis of tibial prosthesis loosening after fixed-bearing unicompartmental knee arthroplasty for osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2191-2198. |
| [2] | Zheng Wangyang, Fei Ji, Yang Di, Zhao Lang, Wang Lingli, Liu Peng, Li Haiyang. Finite element analysis of the force changes of the supraspinatus tendon and glenohumeral joint during the abduction and flexion of the humerus [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2199-2207. |
| [3] | Cai Qirui, Dai Xiaowei, Zheng Xiaobin, Jian Sili, Lu Shaoping, Liu Texi, Liu Guoke, Lin Yuanfang. Mechanical effects of Long’s traction orthopedic method on cervical functional units: quantitative analysis of biomechanical model of head and neck [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2208-2216. |
| [4] | Rao Jingcheng, Li Yuwan, Zheng Hongbing, Xu Zhi, Zhu Aixiang, Shi Ce, Wang Bing, Yang Chun, Kong Xiangru, Zhu Dawei. Biomechanical differences between the new proximal femoral stable intramedullary nail and traditional intramedullary nail#br# [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2217-2225. |
| [5] | Chen Long, Wang Xiaozhen, Xi Jintao, Lu Qilin. Biomechanical performance of short-segment screw fixation combined with expandable polyetheretherketone vertebral body replacement in osteoporotic vertebrae [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2226-2235. |
| [6] | Li Zhifei, Han Bin, Liu Qiuli, Zhang Zhanming, Wei Haokai, Zuo Kuangshi, Zhang Yisheng. Cervical motion characteristics in patients with cervical spondylotic radiculopathy based on motion capture technology [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2286-2293. |
| [7] | Wang Nan, Chen Shuang, Xi Zhipeng, Qian Yuzhang, Zhang Xiaoyu, Gu Jun, Kang Ran, Xie Lin. MRI evaluation of nerve root subsidence sign affecting efficacy of percutaneous endoscopic decompression in lumbar spinal stenosis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2262-2268. |
| [8] | Zhang Zizheng, Luo Wang, Liu Changlu. Application value of finite element analysis on unicompartmental knee arthroplasty for medial knee compartmental osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2313-2322. |
| [9] | Chen Huiting, Zeng Weiquan, Zhou Jianhong, Wang Jie, Zhuang Congying, Chen Peiyou, Liang Zeqian, Deng Weiming. Tail anchoring technique of vertebroplasty in treatment of osteoporotic vertebral compression fractures with intravertebral cleft: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2145-2152. |
| [10] | Cheng Qisheng, Julaiti·Maitirouzi, Xiao Yang, Zhang Chenwei, Paerhati·Rexiti. Finite element analysis of novel variable-diameter screws in modified cortical bone trajectory of lumbar vertebrae [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2162-2171. |
| [11] | Liu Jiafu, Ren Ruxia, Liao Zhouwei, Zhou Xiali, Wu Yihong, Zhang Shaoqun. Three-dimensional finite element analysis of cervical spine biomechanical characteristics in a rat model of cervical vertigo [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2182-2190. |
| [12] | Zhu Xiaolong, Zhang Wei, Yang Yang. Visualization analysis of research hotspots and cutting-edge information in the field of intervertebral disc regeneration and repair [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2391-2402. |
| [13] | Wen Fayan, Li Yan, Qiang Tianming, Yang Chen, Shen Linming, Li Yadong, Liu Yongming. Unilateral biportal endoscopic technology for treatment of lumbar degenerative diseases: global research status and changing trends [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2380-2390. |
| [14] | Xinjiang Branch of China Trauma Rescue & Treatment Association. Expert consensus on diagnosis and treatment of brucellar osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2403-2412. |
| [15] | Pan Zhiyi, Huang Jiawen, Xue Wenjun, Xu Jianda. Advantages of MXene-based flexible electronic sensors and their application in monitoring diabetic foot wounds [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2023-2032. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||