Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (12): 3014-3028.doi: 10.12307/2026.712
Previous Articles Next Articles
Effect and mechanism of dichloromethane extract of fresh Sambucus adnata Wall. in rat osteoarthritis models
Lu Yuchun1, Zhu Zimo1, 2, Li Chaomeng1, Liu Ju1, Jiang Zixian1, Li Xiufang1, Wang Tao3, Wang Wenjing1
- 1School of Traditional Chinese Medicine, Yunnan University of Chinese Medicine, Kunming 650500, Yunnan Province, China; 2Yunnan Key Laboratory of Dai and Yi Medicines, Yunnan University of Chinese Medicine, Kunming 650500, Yunnan Province, China; 3Department of Orthopedics, Kunming Municipal Hospital of Traditional Chinese Medicine, Kunming 650051, Yunnan Province, China
-
Received:2025-04-03Accepted:2025-08-31Online:2026-04-28Published:2025-09-29 -
Contact:Wang Wenjing, PhD, Professor, Doctoral supervisor, School of Traditional Chinese Medicine, Yunnan University of Chinese Medicine, Kunming 650500, Yunnan Province, China Co-corresponding author: Wang Tao, MS, Associate chief physician, Department of Orthopedics, Kunming Municipal Hospital of Traditional Chinese Medicine, Kunming 650051, Yunnan Province, China -
About author:Lu Yuchun, MS candidate, School of Traditional Chinese Medicine, Yunnan University of Chinese Medicine, Kunming 650500, Yunnan Province, China Zhu Zimo, PhD candidate, School of Traditional Chinese Medicine, Yunnan University of Chinese Medicine, Kunming 650500, Yunnan Province, China; Yunnan Key Laboratory of Dai and Yi Medicines, Yunnan University of Chinese Medicine, Kunming 650500, Yunnan Province, China Lu Yuchun and Zhu Zimo contributed to this work. -
Supported by:the National Natural Science Foundation of China (Regional Program), No. 82160744 (to WWJ); Song Shaojiang Expert Workstation in Yunnan Province, No. 202305AF150030 (to WWJ); A Preclinical Study of Sambucus adnata Wall. in the Treatment of Osteoarthritis, No. 30272110298 (to WWJ); 12th Five-year Key Construction Discipline of State Administration of Traditional Chinese Medicine - "Dai Pharmacy," No. 024SS24011 (to ZZM)
CLC Number:
Cite this article
Lu Yuchun, Zhu Zimo, Li Chaomeng, Liu Ju, Jiang Zixian, Li Xiufang, Wang Tao, Wang Wenjing. Effect and mechanism of dichloromethane extract of fresh Sambucus adnata Wall. in rat osteoarthritis models[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(12): 3014-3028.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
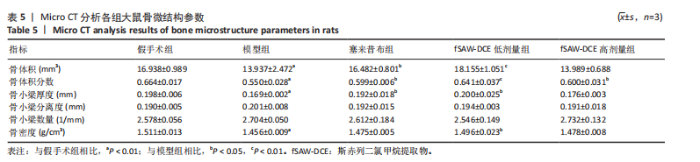
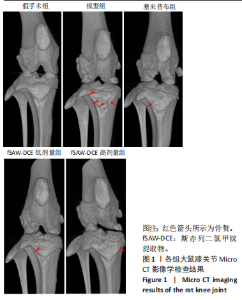
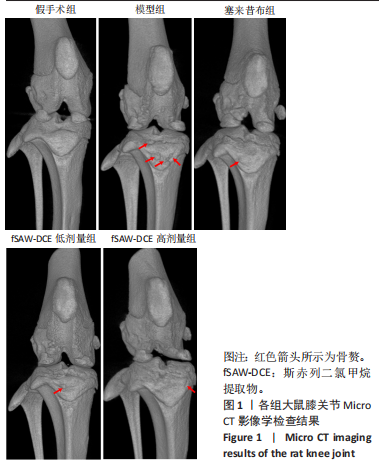
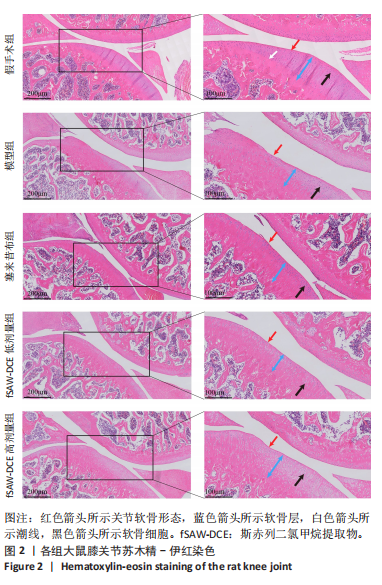
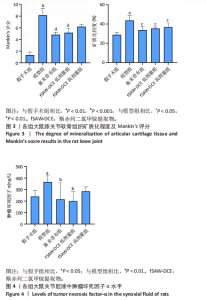
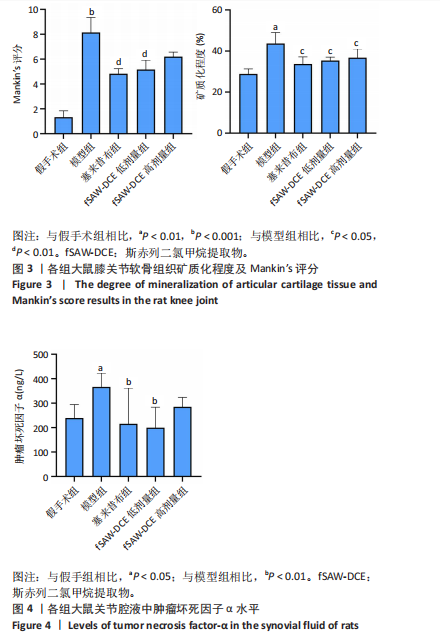
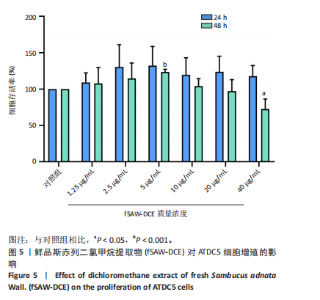
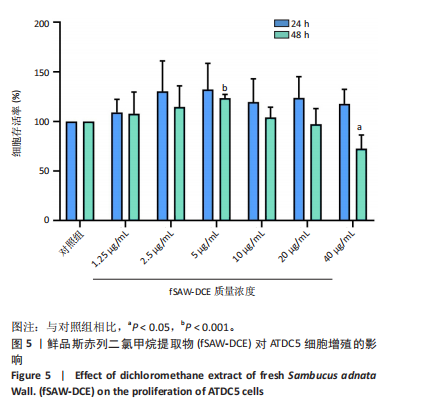
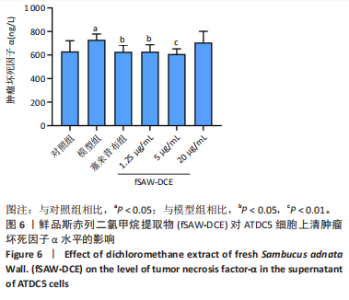
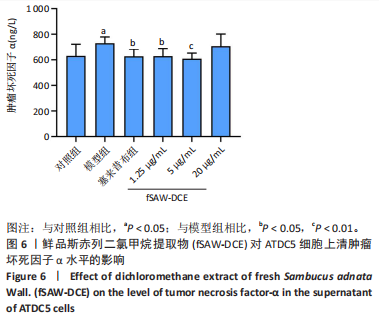
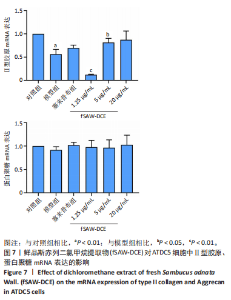
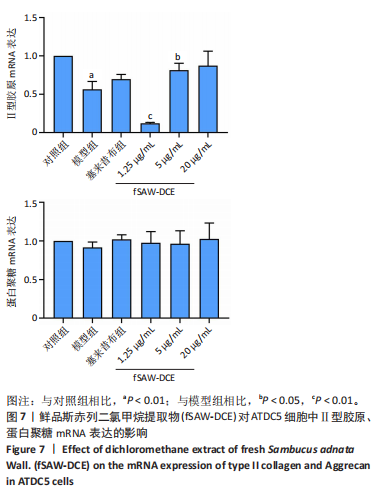
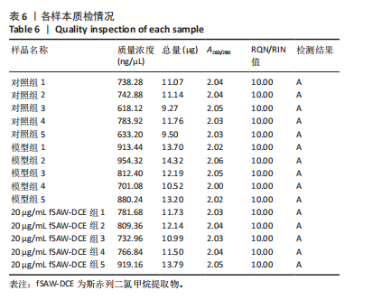
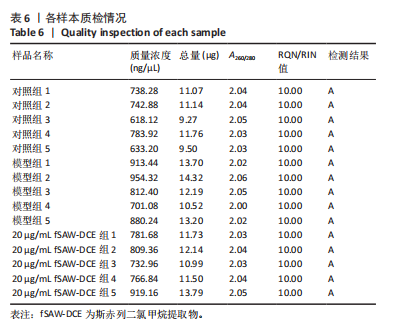
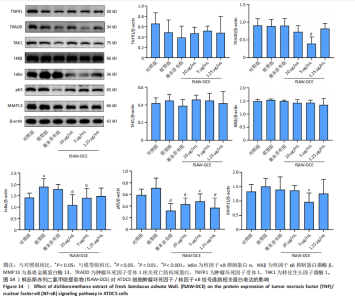
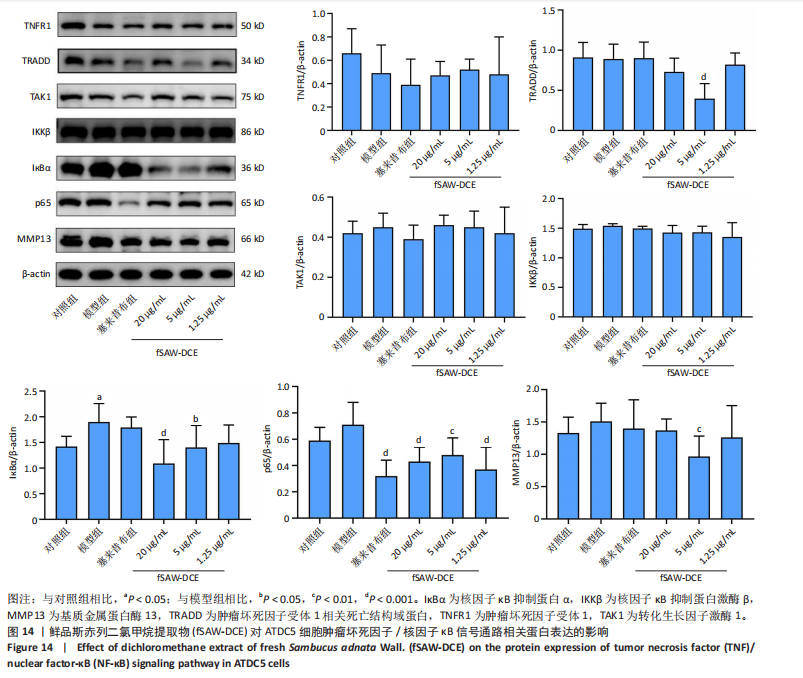
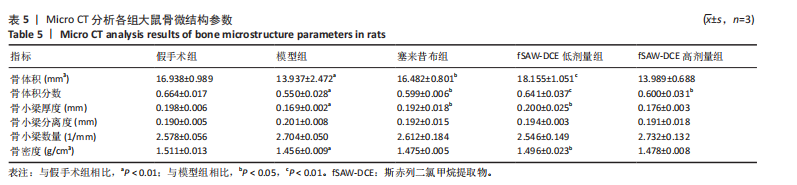
2.1 实验动物数量分析 参与实验SD大鼠40只,均进入结果分析。 2.2 Micro CT影像学检查结果 CT结果显示假手术组大鼠关节面光滑,无明显损伤,无骨赘生成;与假手术组相比,模型组大鼠关节表面粗糙,有明显骨赘生成,关节间隙变窄;与模型组相比,经塞来昔布及低、高剂量fSAW-DCE干预后关节面较光滑,骨赘生成减少,关节损伤减轻,关节间隙变宽,见图1。 与假手术组相比,模型组大鼠骨体积、骨体积分数、骨小梁厚度、骨密度显著降低(P < 0.01);与模型组相比,塞来昔布组骨体积、骨体积分数、骨小梁厚度显著升高(P < 0.05),fSAW-DCE低剂量组骨体积、骨体积分数、骨小梁厚度、骨密度显著升高 (P < 0.05,P < 0.01),fSAW-DCE高剂量组骨体积分数显著升高(P < 0.05),见表5。 2.3 fSAW-DCE对骨关节炎大鼠关节软骨病理形态的影响 苏木精-伊红染色结果显示,假手术组大鼠膝关节软骨染色均匀,软骨表面光滑平整无明显损伤,软骨组织完整,软骨细胞排列整齐,潮线完整,未见异常改变;模型组大鼠软骨厚度明显变薄,软骨破坏明显,中间区域着色较浅,潮线结构消失,软骨细胞排列散乱并伴有簇集的现象,软骨层厚度变薄,软骨细胞数量明显减少;塞来昔布组软骨形态有明显改善,软骨结构完整,软骨细胞数量与排列有明显改善,软骨层厚度增加;fSAW-DCE低、高剂量组软骨表面较为光滑,软骨形态与结构完整性有所改善,软骨层厚度有所增加,软骨细胞数量与排列较好,见图2。 2.4 fSAW-DCE对骨关节炎大鼠关节软骨矿质化程度及Mankin’s评分的影响 与假手术组相比,模型组大鼠关节软骨矿质化程度严重(P < 0.001),Mankin’s评分明显升高(P < 0.01);与模型组相比,塞来昔布组及fSAW-DCE低剂量组关节软骨矿质化程度及Mankin’s 评分明显降低(P < 0.05,P < 0.01), fSAW-DCE高剂量组关节软骨矿质化程度明显降低(P < 0.05),Mankin’s评分有降低趋势,但结果无统计学差异,见图3。 2.5 fSAW-DCE对骨关节炎大鼠关节腔液中肿瘤坏死因子α水平的影响 与假手术组相比,模型组大鼠关节腔液中肿瘤坏死因子α水平显著升高(P < 0.05);与模型组相比,塞来昔布组及fSAW-DCE低剂量组关节腔液中肿瘤坏死因子α水平明显降低(P < 0.01),fSAW-DCE高剂量组关节腔液中肿瘤坏死因子α水平呈降低趋势,但结果无统计学差异,见图4。 2.6 fSAW-DCE对ATDC5细胞增殖的影响 与对照组相比,1.25-40 μg/mL fSAW-DCE干预24 h后细胞存活率增加,但差异无显著性意义;1.25-5 μg/mL fSAW-DCE干预48 h后细胞存活率呈上升趋势,10-40 μg/mL fSAW-DCE干预48 h后细胞存活率呈下降趋势,其中5 μg/mL fSAW-DCE干预48 h后可明显增加细胞的存活率、40 μg/mL fSAW-DCE干预48 h后可明显降低细胞的存活率(P < 0.001,P < 0.05),见图5。 2.7 fSAW-DCE对ATDC5细胞上清中肿瘤坏死因子α水平的影响 与对照组相比,模型组上清中肿瘤坏死因子α水平明显升高(P < 0.05);与模型组相比,塞来昔布组及1.25,5 μg/mL fSAW-DCE组细胞上清中肿瘤坏死因子α水平明显降低(P < 0.05,P < 0.01),20 μg/mL fSAW-DCE组细胞上清中肿瘤坏死因子α水平呈降低趋势,但差异无显著性意义,见图6。"

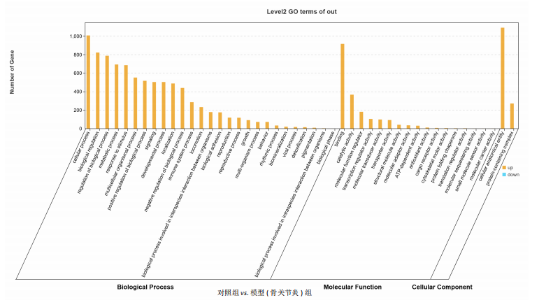
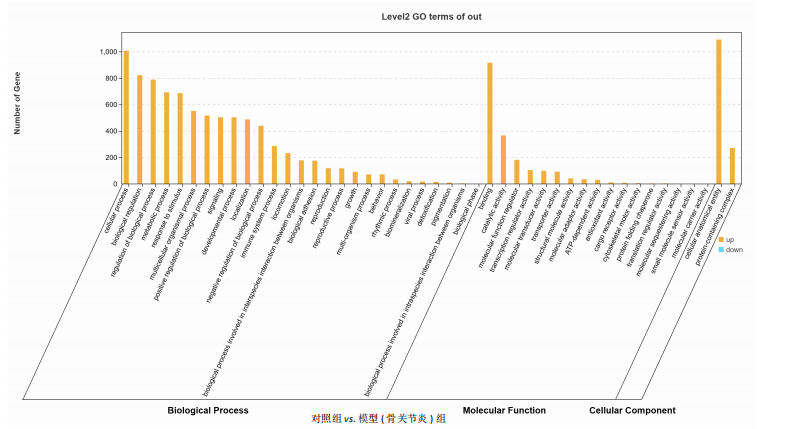
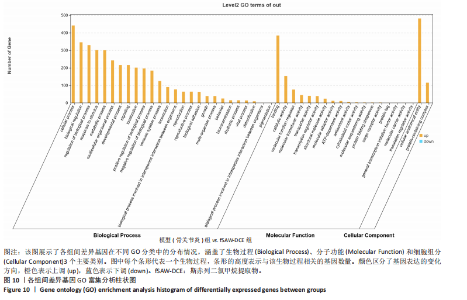
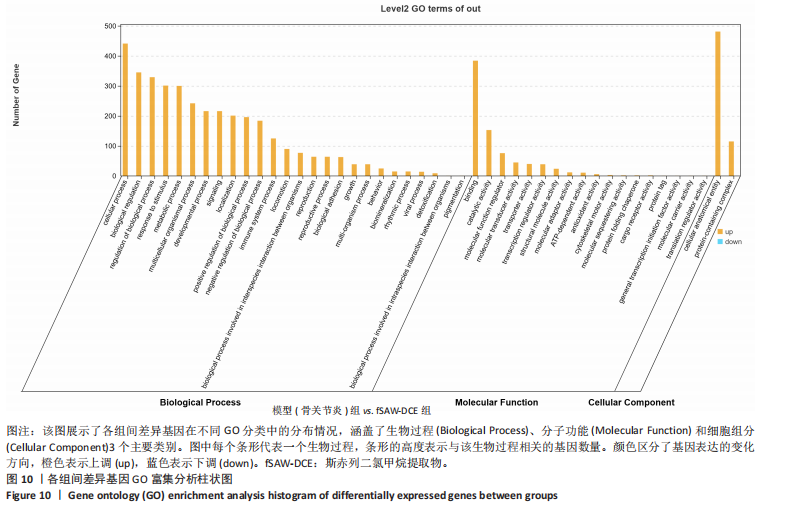
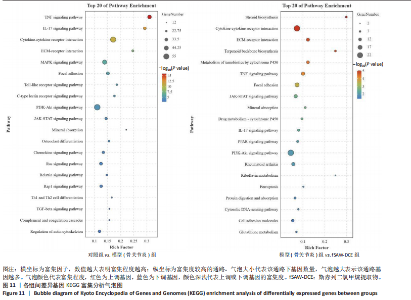
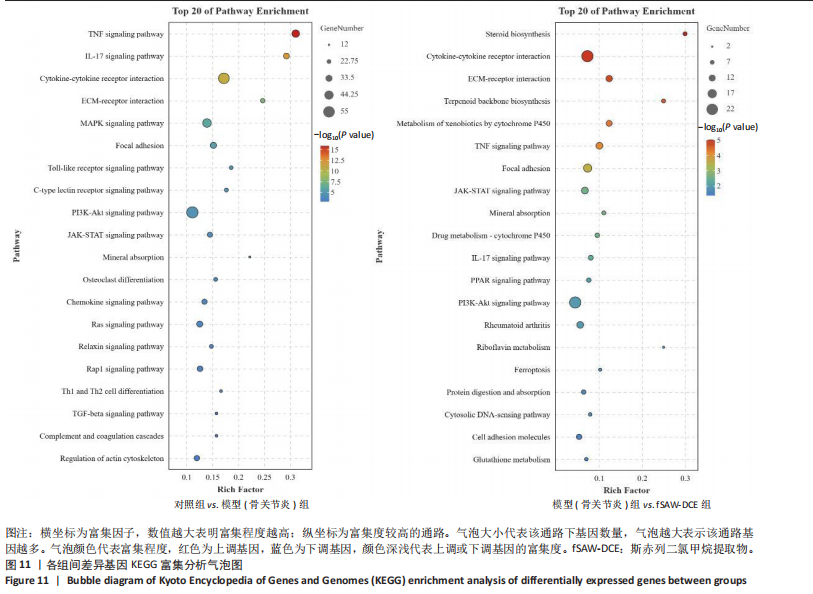
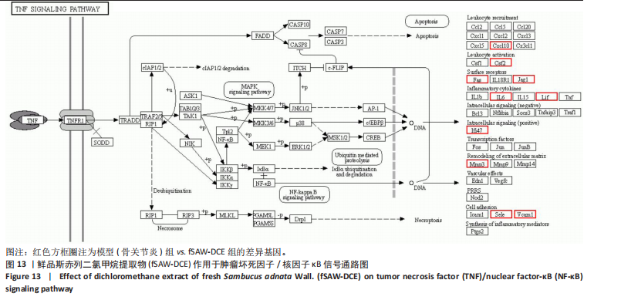
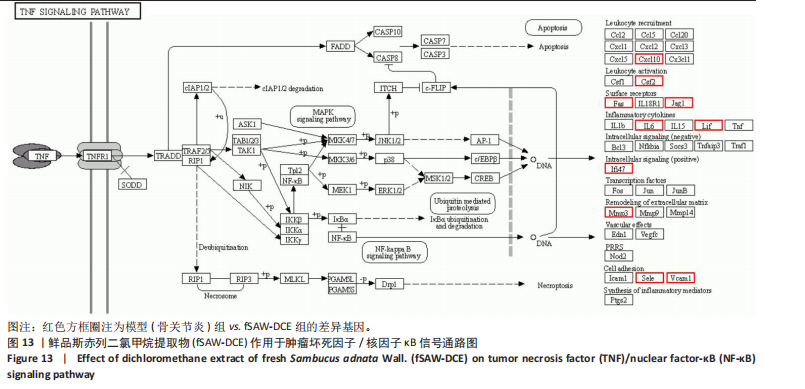
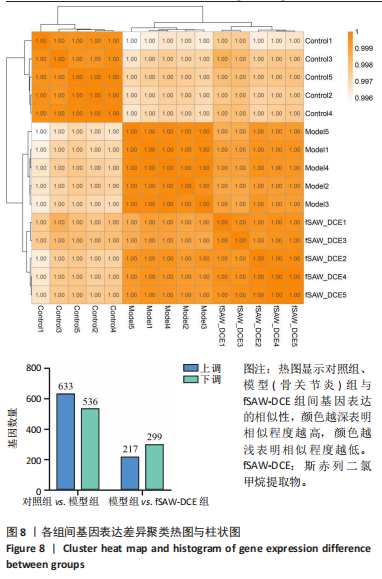
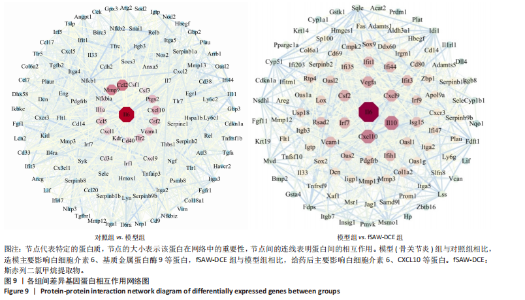
2.9.2 基因表达差异分析 样本间相关性热图显示各组间分类界限明显,各组内样本基因表达相似性较高。差异基因数目柱状图显示,与对照组相比,模型组共有1 169个差异基因,其中633个基因上调,536个基因下调;与模型组相比,20 μg/mL fSAW-DCE 组共有516个差异基因,其中217个基因上调,299个基因下调,见图8。 2.9.3 蛋白相互作用网络 将差异基因导入STRING网站进行蛋白间相互作用分析,物种选择小鼠,下载其tsv文件,并导入Cytoscape 3.10.1进行可视化,以degree值为指标将差异基因进行大小排序,以筛选核心靶点。蛋白相互作用网络图结果显示,与对照组相比,造模后主要影响了白细胞介素6、C-C趋化因子配体2、基质金属蛋白酶9等基因;与模型组相比,给予fSAW-DCE后主要影响白细胞介素6、C-X-C趋化因子配体10、C-X-C趋化因子配体9等基因,见图9。 2.9.4 GO和KEGG富集分析 将差异基因及其FC值导入Omicshare云平台进行动态GO和KEGG富集分析,物种选择小鼠。富集结果按照P值从小到大进行排列,选取排名前20的结果进行展示,P < 0.05视为结果有显著性意义。KEGG富集结果删除与关节炎不相关的人类疾病后,选取排名前20的结果进行"
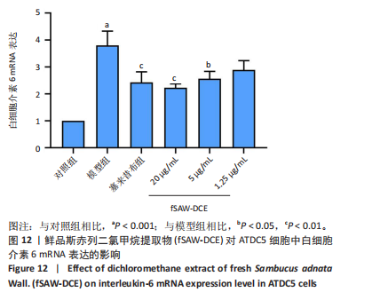
展示。GO和KEGG富集结果显示,与对照组相比,模型组富集到的基因主要涉及生物调节、多细胞生物过程及免疫系统过程等生物过程;调节催化活性、抗氧化活性及小分子传感器活性等分子功能;调节细胞解剖实体及含蛋白质的复合物等细胞组成;影响肿瘤坏死因子、白细胞介素17、细胞外基质受体相互作用等信号通路发挥作用。与模型组相比,给予fSAW-DCE后富集到的基因主要涉及生物调节、多细胞生物过程及免疫系统过程等生物过程;调节催化活性、ATP依赖活性及抗氧化活性等分子功能;调节细胞解剖实体及含蛋白质的复合物等细胞组成;通过影响细胞外基质受体相互作用、肿瘤坏死因子、Janus激酶-信号转导和转录活化因子等信号通路发挥作用,见图10,11。 2.10 转录组学结果验证 2.10.1 核心基因检测结果 根据蛋白相互作用网络分析结果,选择白细胞介素6进行验证。RT-qPCR结果显示,与对照组相比,模型组软骨细胞中白细胞介素6 mRNA表达水平明显升高(P < 0.001);与模型组相比,经塞来昔布及5,20 μg/mL fSAW-DCE干预后白细胞介素6 mRNA表达水平明显降低(P < 0.01,P < 0.05),1.25 μg/mL fSAW-DCE干预后白细胞介素6 mRNA表达水平有降低的趋势,见图12。"

| [1] TANG S, ZHANG C, OO WM, et al. Osteoarthritis. Nat Rev Dis Primers. 2025;11(1):10. [2] CAO F, XU Z, LI XX, et al. Trends and cross-country inequalities in the global burden of osteoarthritis, 1990-2019: A population-based study. Ageing Res Rev. 2024;99:102382. [3] HUNTER DJ, BIERMA-ZEINSTRA S. Osteoarthritis. Lancet. 2019; 393(10182):1745-1759. [4] LIU Y, ZHANG Z, LI T, et al. Senescence in osteoarthritis: from mechanism to potential treatment. Arthritis Res Ther. 2022;24(1):174. [5] MAKARCZYK MJ. Cell Therapy Approaches for Articular Cartilage Regeneration. Organogenesis. 2023;19(1):2278235. [6] ALCAIDE-RUGGIERO L, MOLINA-HERNÁNDEZ V, GRANADOS MM, et al. Main and Minor Types of Collagens in the Articular Cartilage: The Role of Collagens in Repair Tissue Evaluation in Chondral Defects. Int J Mol Sci. 2021;22(24):13329. [7] WEBER AE, BOLIA IK, TRASOLINI NA. Biological strategies for osteoarthritis: from early diagnosis to treatment. Int Orthop. 2021; 45(2):335-344. [8] JANG S, LEE K, JU JH. Recent Updates of Diagnosis, Pathophysiology, and Treatment on Osteoarthritis of the Knee. Int J Mol Sci. 2021; 22(5):2619. [9] VINCENTI MP, BRINCKERHOFF CE. Transcriptional regulation of collagenase (MMP-1, MMP-13) genes in arthritis: integration of complex signaling pathways for the recruitment of gene-specific transcription factors. Arthritis Res. 2002;4(3):157-164. [10] 杨本雷.中国彝族药学[M].昆明:云南民族出版社,2004. [11] 王泽玲,韩立峰,郝佳,等.接骨木属植物化学成分及药理活性研究进展[J].中成药,2023,45(6):1936-1943. [12] 江自鲜,陆玉春,李朝梦,等.斯赤列提取物抑制骨关节炎模型大鼠的异常血管新生[J].中国组织工程研究,2024,28(34):5458-5466. [13] YANG D, XU K, XU X, et al. Revisiting prostaglandin E2: A promising therapeutic target for osteoarthritis. Clin Immunol. 2024;260:109904. [14] 郑俭彬,陆玉春,江自鲜,等.彝药斯赤列甲醇提取物对骨关节炎模型大鼠的治疗作用及靶点预测[J].中国组织工程研究,2024, 28(23):3627-3635. [15] MACRI EM, SELLES RW, STEFANIK JJ, et al. OARSI year in review 2023: Rehabilitation and outcomes. Osteoarthritis Cartilage. 2023; 31(12):1534-1547. [16] BANNURU RR, OSANI MC, VAYSBROT EE, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27(11):1578-1589. [17] MINTARJO JA, POERWANTO E, TEDYANTO EH. Current Non-surgical Management of Knee Osteoarthritis. Cureus. 2023;15(6):e40966. [18] 吴正波.斯赤列石油醚和乙酸乙酯萃取部位化学成分研究[D].昆明:云南中医药大学, 2023. [19] 李巧月,王葳,仇贤庆,等.彝药斯赤列地上部分挥发油研究[J].中南药学,2019,17(10):1655-1658. [20] 刘冬丽,王葳,陈飞龙,等.血满草化学成分及生物活性的研究进展[J].华西药学杂志,2018,33(6):542-545. [21] GHEISARI A, RISTANIEMI A, HAGHIGHATNEJAD M, et al. Alterations in mechanical properties of rabbit collateral ligaments eight weeks after anterior cruciate ligament transection. J Biomech. 2024;176:112350. [22] 罗平.前交叉韧带与膝骨关节炎的结构改变及膝关节置换术的相关性研究[D].广州:南方医科大学,2024. [23] RODRIGUEZ-MERCHAN EC, ENCINAS-ULLAN CA. Knee Osteoarthritis Following Anterior Cruciate Ligament Reconstruction: Frequency, Contributory Elements, and Recent Interventions to Modify the Route of Degeneration. Arch Bone Jt Surg. 2022;10(11):951-958. [24] KIM YB, FITZSIMMONS JS, BELLATO E, et al. Anterolateral rotatory instability of the elbow: a possible etiology of primary osteoarthritis. Clin Shoulder Elb. 2024;27(4):419-427. [25] LOU Y, SONG F, KANG Y, et al. Periodic Mechanical Stress Inhibits the Development of Osteoarthritis via Regulating ATF3-Akt Axis. J Inflamm Res. 2023;16:5613-5628. [26] ELKHENANY HA, LINARDI RL, ORTVED KF. Differential modulation of inflammatory cytokines by recombinant IL-10 in IL-1β and TNF-α ̶ stimulated equine chondrocytes and synoviocytes: impact of washing and timing on cytokine responses. BMC Vet Res. 2024;20(1):546. [27] PARK YM, SHIN DY, LEE HY, et al. Pinus densiflora Root Extract Attenuates Osteoarthritis Progression by Inhibiting Inflammation and Cartilage Degradation in Interleukin-1β and Monosodium Iodoacetate-Induced Osteoarthritis Models. Nutrients. 2024;16(22):3882. [28] SCHREINER AJ, STOKER AM, BOZYNSKI CC, et al. Clinical Application of the Basic Science of Articular Cartilage Pathology and Treatment. J Knee Surg. 2020;33(11):1056-1068. [29] BAKER BM, SHAH RP, HUANG AH, et al. Dynamic tensile loading improves the functional properties of mesenchymal stem cell-laden nanofiber-based fibrocartilage. Tissue Eng Part A. 2011;17(9-10):1445-1455. [30] 伍伟挺,黎润光,曹生鲁,等.过度周期性机械应力刺激可引起软骨细胞炎症反应及凋亡[J].中国组织工程研究,2021,25(29):4608-4613. [31] TAHERI S, WINKLER T, SCHENK LS, et al. Developmental Transformation and Reduction of Connective Cavities within the Subchondral Bone. Int J Mol Sci. 2019;20(3):770. [32] CHEN L, ZHANG Z, LIU X. Role and Mechanism of Mechanical Load in the Homeostasis of the Subchondral Bone in Knee Osteoarthritis: A Comprehensive Review. J Inflamm Res. 2024;17:9359-9378. [33] LUO Y, ZHANG Y, HUANG Y. Icariin Reduces Cartilage Degeneration in a Mouse Model of Osteoarthritis and is Associated with the Changes in Expression of Indian Hedgehog and Parathyroid Hormone-Related Protein. Med Sci Monit. 2018;24:6695-6706. [34] PREEDY MK, WHITE MRH, TERGAONKAR V. Cellular heterogeneity in TNF/TNFR1 signalling: live cell imaging of cell fate decisions in single cells. Cell Death Dis. 2024;15(3):202. [35] DOSTERT C, GRUSDAT M, LETELLIER E, et al. The TNF Family of Ligands and Receptors: Communication Modules in the Immune System and Beyond. Physiol Rev. 2019;99(1):115-160. [36] XU D, ZHAO H, JIN M, et al. Modulating TRADD to restore cellular homeostasis and inhibit apoptosis. Nature. 2020;587(7832):133-138. [37] SUN K, GUO Z, ZHANG J, et al. Inhibition of TRADD ameliorates chondrocyte necroptosis and osteoarthritis by blocking RIPK1-TAK1 pathway and restoring autophagy. Cell Death Discov. 2023;9(1):109. [38] YU H, LI M, WEN X, et al. Elevation of α-1,3 fucosylation promotes the binding ability of TNFR1 to TNF-α and contributes to osteoarthritic cartilage destruction and apoptosis. Arthritis Res Ther. 2022;24(1):93. [39] DING SL, PANG ZY, CHEN XM, et al. Urolithin a attenuates IL-1β-induced inflammatory responses and cartilage degradation via inhibiting the MAPK/NF-κB signaling pathways in rat articular chondrocytes. J Inflamm (Lond). 2020;17:13. [40] ZHU L, LAMA S, TU L, et al. TAK1 signaling is a potential therapeutic target for pathological angiogenesis. Angiogenesis. 2021;24(3):453-470. [41] LI LJ, ZHANG SJ, LIU P, et al. Corilagin Interferes With Toll-Like Receptor 3-Mediated Immune Response in Herpes Simplex Encephalitis. Front Mol Neurosci. 2019;12:83. [42] ANSARI MY, AHMAD N, HAQQI TM. Oxidative stress and inflammation in osteoarthritis pathogenesis: Role of polyphenols. Biomed Pharmacother. 2020;129:110452. [43] KUPPA SS, KIM HK, KANG JY, et al. Role of Mesenchymal Stem Cells and Their Paracrine Mediators in Macrophage Polarization: An Approach to Reduce Inflammation in Osteoarthritis. Int J Mol Sci. 2022;23(21):13016. [44] GILBERT SJ, BONNET CS, BLAIN EJ. Mechanical Cues: Bidirectional Reciprocity in the Extracellular Matrix Drives Mechano-Signalling in Articular Cartilage. Int J Mol Sci. 2021;22(24):13595. [45] VINCENT TL, MCCLURG O, TROEBERG L. The Extracellular Matrix of Articular Cartilage Controls the Bioavailability of Pericellular Matrix-Bound Growth Factors to Drive Tissue Homeostasis and Repair. Int J Mol Sci. 2022;23(11):6003. [46] HOWES JM, BIHAN D, SLATTER DA, et al. The recognition of collagen and triple-helical toolkit peptides by MMP-13: sequence specificity for binding and cleavage. J Biol Chem. 2014;289(35):24091-24101. [47] LI T, PENG J, LI Q, et al. The Mechanism and Role of ADAMTS Protein Family in Osteoarthritis. Biomolecules. 2022;12(7):959. |
| [1] | Ye Wei, Jiang Dongfu, Zhuang Jielin, Lai Huaxin. Effect of warm acupuncture combined with platelet-rich plasma injection on gait parameters and joint function recovery of knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(12): 2975-2985. |
| [2] | Shalayiding · Aierxiding, Gao Jian, Alimujiang · Abudourousuli, Kutiluke · Shoukeer, Aikebaierjiang · Aisaiti, Gulimire · Yilihamu, Jiang Kan, Aikeremujiang · Muheremu. Mechanisms by which macrophage polarization regulates bone destruction in rheumatoid arthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(10): 2484-2490. |
| [3] | Zhang Qian, Huang Dongfeng. Weighted gene co-expression network analysis combined with machine learning to screen and validate biomarkers for osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1096-1105. |
| [4] | Chen Yixian, Chen Chen, Lu Liheng, Tang Jinpeng, Yu Xiaowei. Triptolide in the treatment of osteoarthritis: network pharmacology analysis and animal model validation [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 805-815. |
| [5] | Pang Jiahui, Wang Bo, Hu Yingxuan, Hu Ziwei, Wu Wen. Association between dietary preferences and the risk of osteoarthritis in Europeans: analysis of human genome-wide association study data [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6333-6342. |
| [6] | Sun Hailiang, Pang Jian, Shi Wanzhong, Shi Ying. Protective effect of Huaizhen Yanggan Capsule on knee osteoarthritis induced by sodium iodoacetate in model mice [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(26): 5579-5587. |
| [7] | Wang Zhe, Qi Yansong, Xu Yongsheng. Diagnosis and treatment of osteoarthritis with exosomes derived from different stem cells and carrying non-coding RNA [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(19): 4122-4131. |
| [8] | Wu Fuzhang, Zhang Pengli, Zhang Zhenhua, He Yongbing, Sun Heyan. Acellular cartilage extracellular matrix homogenate combined with oxymatrine on treatment of osteoarthritis in rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(13): 2675-2682. |
| [9] | Tian Sheng, Wang Xi, Wang Yongcheng, Liu Yaning, Yang Hongquan. Mechanism underlying microRNA-214 regulation of cartilage and subchondral bone metabolism in osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(12): 2466-2474. |
| [10] | Shen Xuyu, Luo Chengnuo, Zhang Xiaoyun, Jiang Zhouying, Chai Yuan . Role and mechanism of alkaloid components of traditional Chinese medicine against knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(11): 2368-2376. |
| [11] | Tian Yanhu, Huang Xinan, Guo Tongtong, Rusitanmu·Ahetanmu, Luo Jiangmiao, Xiao Yao, Wang Chao, Wang Weishan . Machine learning identification of LRRC15 and MICB as immunodiagnostic markers for rheumatoid arthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(11): 2411-2420. |
| [12] | Ma Haoyu, Qiao Hongchao, Hao Qianqian, Shi Dongbo. Causal effects of different exercise intensities on the risk of osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1305-1311. |
| [13] | Liu Mengfei, Chen Gang, Shi Yihan, Zeng Lin, Jiang Kan, Yilihamujiang•Wusiman. Finite element analysis of optimization of femoral prosthesis implantation position in unicompartmental knee arthroplasty in osteoporotic patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 464-470. |
| [14] | Lou Xinqi, Zhong Hao, Wang Xiyu, Feng Haoyu, Li Pengcui, Wei Xiaochun, Wang Yanqin, Wu Xiaogang, Chen Weiyi, Xue Yanru. Possible mechanisms of multi-pathway biological effects of laser therapy for knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(34): 5521-5527. |
| [15] | Li Zhengyuan, Hao Lin, Chen Shenghong, Peng Kai, Wang Jun, Yin Zongsheng. Topical application of vancomycin in prevention of early incision infection in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(33): 5346-5350. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||