Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (29): 6317-6325.doi: 10.12307/2025.793
Previous Articles Next Articles
Systematic review of machine learning models for predicting functional recovery and prognosis in stroke
Wang Jiaru1, Zhang Ying2, Yang Yong1, Qi Wen2, Xiao Huaye2, Ma Qiuping1, Yang Lianzhao1, Luo Ziwei1, He Yaqing2, Zhang Jiangyin1, #br# Wei Jiawen1, Meng Yuan1, Tan Silian3#br#
- 1Guangxi University of Chinese Medicine, Nanning 530200, Guangxi Zhuang Autonomous Region, China; 2Faculty of Chinese Medicine Science, Guangxi University of Chinese Medicine, Nanning 530222, Guangxi Zhuang Autonomous Region, China; 3Guangxi Zhuang Autonomous Region Maternal and Child Health Hospital, Nanning 530021, Guangxi Zhuang Autonomous Region, China
-
Received:2024-08-10Accepted:2024-11-05Online:2025-10-18Published:2025-03-08 -
Contact:Yang Yong, PhD, Professor, Master’s supervisor, Guangxi University of Chinese Medicine, Nanning 530200, Guangxi Zhuang Autonomous Region, China -
About author:Wang Jiaru, Master candidate, Guangxi University of Chinese Medicine, Nanning 530200, Guangxi Zhuang Autonomous Region, China Zhang Ying, MS, Associate professor, Senior experimentalist, Faculty of Chinese Medicine Science, Guangxi University of Chinese Medicine, Nanning 530222, Guangxi Zhuang Autonomous Region, China Wang Jiaru and Zhang Ying contributed equally to this article. -
Supported by:2022 Scientific Research Basic Ability Improvement Project of Guangxi University Young and Middle-aged Teachers (Natural Science), No. 2022KY1670 (to ZY); 2022 School-Level Scientific Research Project of Faculty of Chinese Medicine Science of Guangxi University of Chinese Medicine, No. 2022MS012 (to ZY); 2024 College Student Innovation Training Program Project of Faculty of Chinese Medicine Science of Guangxi University of Chinese Medicine, No. 202413643028 (National Level) (to HYQ) 2022 School-Level Scientific Research Project of Guangxi University of Chinese Medicine, No. 2022MS020 (to YY); High-level Talent Innovation Cultivation Team of Guangxi University of Chinese Medicine, No. 2022A010 (to MQP); 2020 Guangxi Philosophy and Social Sciences Planning Research Project, No. 20FGL024 (to YLZ); Guangxi Natural Science Foundation Project, No. 2013GXNSFDA278001 (to YLZ)
CLC Number:
Cite this article
Wang Jiaru, Zhang Ying, Yang Yong, Qi Wen, Xiao Huaye, Ma Qiuping, Yang Lianzhao, Luo Ziwei, He Yaqing, Zhang Jiangyin, Wei Jiawen, Meng Yuan, Tan Silian. Systematic review of machine learning models for predicting functional recovery and prognosis in stroke[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6317-6325.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
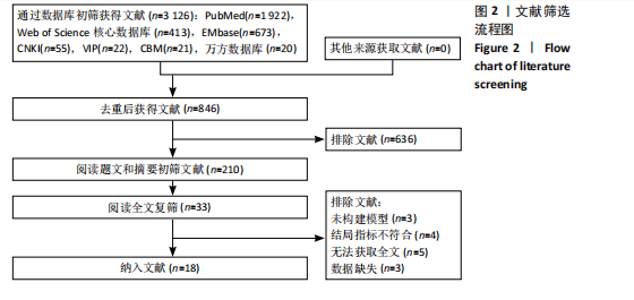
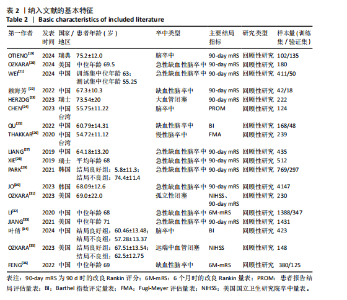
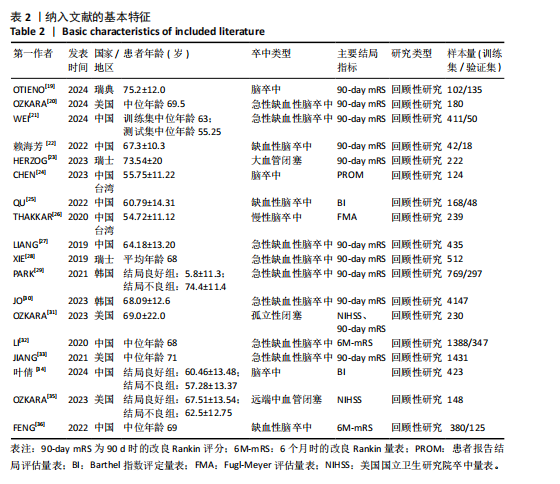
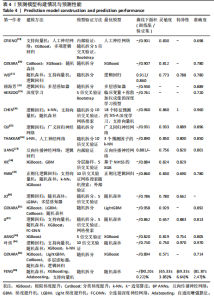
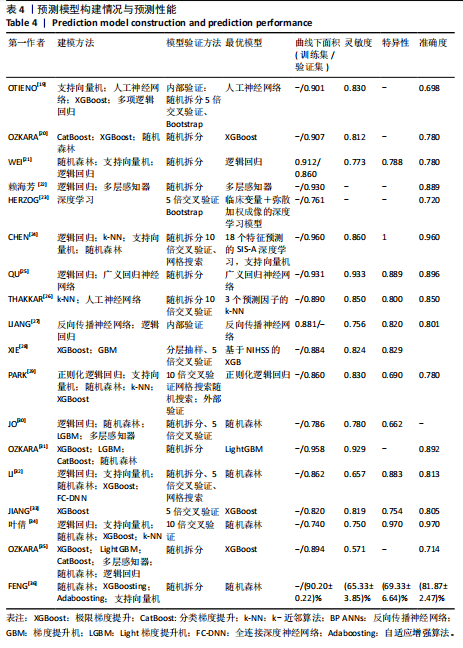
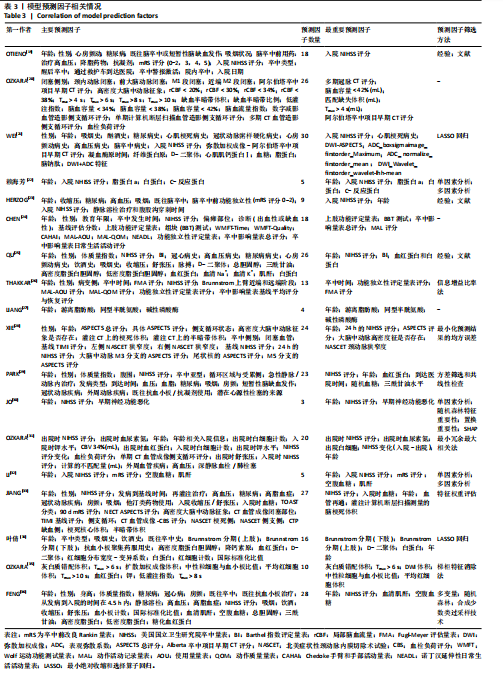
2.1 文献检索结果 检索数据库共得到3 126篇论文,没有通过其他来源检索的文献。使用 EndNote X9去除重复文献,经过逐层筛选后最终共有18篇研究结果被纳入分析[19-36]。文献筛选流程图见图2。 2.2 纳入文献的一般特征 此次研究共纳入了18项研究,均为回顾性研究,研究时间跨度为2019-2024年,总共涉及114 263例脑卒中患者,用于模型开发和验证。其中3项样本量最大的研究依赖于共享的数字数据库和数据收集的基础设施[19,30,32];患者平均年龄为65.89岁;大多数研究集中在缺血性脑卒中[20-23,25,27-33,35-36],仅一项为慢性脑卒中[26],其他未对卒中类型进行分类;11项研究使用90 d时的改良Rankin评分作为主要结局指标作为结局指标[19-23,27-31,33]。纳入文献的基本特征见表2。 2.3 预测模型构建情况与预测性能 纳入的18项研究共运用13种机器学习方法构建了150个预测模型,其中应用次数最多的3种方法为逻辑回归、随机森林、极限梯度提升(extreme gradient boosting,XGBoost)。模型验证方面,仅有1项研究实施了外部验证[29]。缺失数据方面,8项研究报告了缺失数据的处理方法[19-20,23,25,30-31,33-35]。 所有研究均列出最优的预测模型,均报告了AUC值,范围为0.74-0.96,CHEN等[24]的研究中支持向量机的AUC最高为0.96。灵敏度(Sensitivity)范围为0.65-0.933;特异性(Specificity)范围为0.66-1.00;准确度(Accuracy)报告值为0.698-0.97,反映了不同模型在不同数据集上的表现差异。纳入特征的数量和类型因研究而异,既包括临床变量(如年龄、性别、既往病史、"
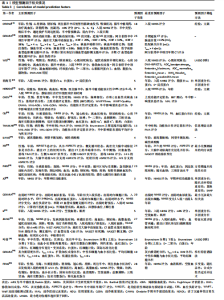
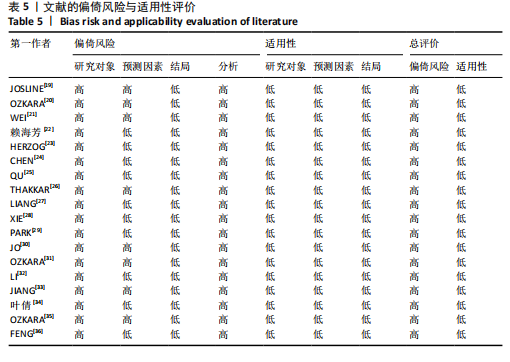
NIHSS评分等),也包括影像学数据(如弥散加权成像、Tmax、脑血容量等)重要特征的选择依赖于具体研究和模型,通常包括年龄、美国国立卫生研究院卒中量表(National Institute of Health stroke scale,NIHSS)评分、影像学指标[如Alberta卒中项目早期CT评分(Alberta Stroke Program Early CT Score,ASPECTS)、脑血容量等]。8项研究采用了临床数据与影像学数据结合来构建模型[21,23,28,30-31,33-35],9项研究仅运用临床数据构建模型[19,22,24-27,32,36],1项研究仅用影像学数据构建模型[20]。纳入的预测因子最多有30个最少为3个。18项研究均给出了研究结果中最重要的特征,其中被提及最多的是NIHSS评分和年龄。模型预测因子相关情况见表3。预测模型构建情况与预测性能见表4。 2.4 偏倚风险评价和适用性评价 根据预测模型偏倚风险评价工具评价标准对纳入研究进行偏倚风险和适用性评价,具体结果见表5。纳入的18项研究均呈现高偏倚风险。在研究对象领域,18项研究均被评为高偏倚风险,导致偏倚风险高的主要原因是研究设计采用了回顾性研究。预测因子领域,"
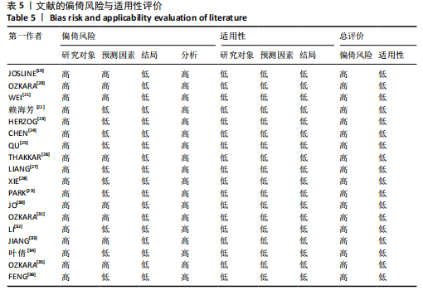
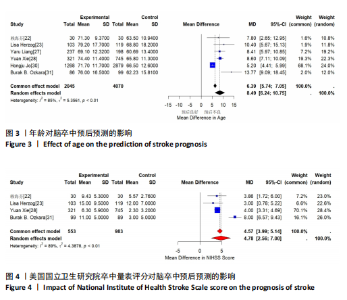
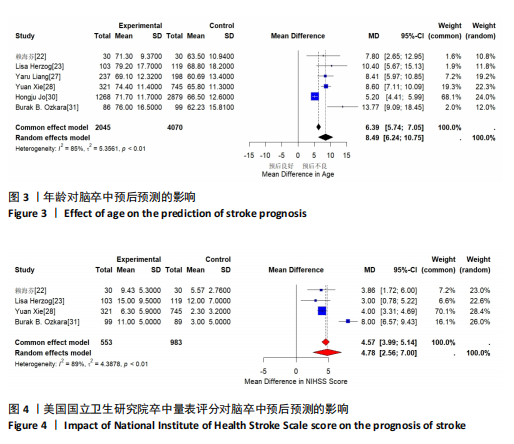
8项研究使用了多中心的数据被评为高偏倚风险[19-21,26,30- 31,33,35],各中心预测因子的评估方式可能不同,其数据采集方式可能存在差异,从而产生偏倚。在结果领域,PARK等[29]的研究中将mRS值0-1设为阳性指标存在一定争议结果领域偏倚风险高,其余研究均清晰报告了结局指标的定义、测量方法,偏倚风险低。分析领域均评价为高风险。建模时每个变量所对应的事件发生数应≥20,验模的样本量应≥100例,8项研究的建模样本量不足[20,22-26,31,35],6项研究的验模样本量< 100例[20,22-25,35]。3项研究未报告模型中预测因素的筛选方法[20,24,27],4项研究仅通过经验和文献来筛选特征[19,23,25-26],10项研究未报告数据是否缺失或缺失数据处理方法不当。在适用性中,所有研究的适用性均较低。 2.5 Meta 分析结果 此次研究18项研究均列出最重要预测因子,其中NIHSS评分、年龄是被提到最多的重要预测因子。 2.5.1 年龄对脑卒中预后预测影响 年龄是脑卒中后功能恢复和预后的重要独立预测因子,通常年龄越大,功能恢复的难度越大,预后越差。老年患者的神经可塑性较差,恢复速度和程度较年轻患者慢。在不同年龄段的患者中,模型的预测能力可能会有所不同。例如,年轻患者的预后往往较好,因此模型在这类患者中的预测准确性较高。而对于老年患者,由于其健康状况的复杂性和多样性,模型的预测可能更加困难。多数研究纳入的患者年龄为≥18岁,并没有详细地划分年龄进行针对性预测。老年患者在卒中后恢复中的功能需求和目标可能与年轻患者不同,这也需要在模型设计中考虑。 利用6项将年龄作为最重要影响因素的研究数据分析了年龄对脑卒中预后预测的预测价值,各研究之间存在异质性(I2=85%,τ2=5.356 1,P < 0.01),采用随机效应模型分析,结果表明年龄是脑卒中预后的重要影响因素。年龄对预后影响的均差(MD)= 8.49,95%CI为(6.24,10.75)。因此,从总体上看,年龄越大的患者更有可能预后不良,但具体影响的大小可能因个体特征和其他因素而异。见图3。 2.5.2 NIHSS评分对脑卒中预后预测的影响 NIHSS评分是临床上广泛使用的量表,用于评估脑卒中的严重程度。NIHSS评分高表示卒中程度严重和预后不良,因此其在预测功能恢复和预后中起关键作用。NIHSS评分也存在一定的局限性:一方面,NIHSS评分对某些特定卒中症状,如语言障碍和视觉缺陷,可能存在偏差;另一方面,NIHSS评分在急性期可能不足以全面反映长期预后。部分轻度卒中的患者虽然NIHSS评分低,但仍可能出现显著的功能障碍,这在预测中可能导致误差需要研究人员进行全面考虑。 利用4项将NIHSS评分作为最重要影响因素的研究数据分析了NIHSS评分对脑卒中预后预测价值,各研究之间存在异质性(I2=89%,τ2=4.387 8,P < 0.01),采用随机效应模型分析,结果表明NIHSS是一个显著的预后指标,MD=4.78,95%CI为(2.56,7.00)。因此,从总体上看,NIHSS评分对于脑卒中预后的影响显著。见图4。"
| [1] KATAN M, LUFT A. Global Burden of Stroke. Semin Neurol. 2018;38(2):208-211. [2] GBD 2019 STROKE COLLABORATORS. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20(10):795-820. [3] WINTERS C, KWAKKEL G, VAN WEGEN E, et al. Moving stroke rehabilitation forward: The need to change research. Neuro Rehabilitation. 2018;43(1):19-30. [4] YUFE R. Stroke prognostication using age and NIH Stroke Scale: SPAN-100. Neurology. 2013,81(6):603. [5] CHEN LL, YAN SM, WANG WT, et al. Cohort study of THRIVE predicting adverse outcomes in acute ischemic stroke of the anterior circulation and posterior circulation after 3 months and 1 year of follow-up. J Clin Neurosci. 2022;96:33-37. [6] COLAlILLO JM, SMITH J. Artificial intelligence in medicine: The rise of machine learning. Emerg Med Australas. 2024;36(4):628-631. [7] OBERMEYER Z, EMANUEL EJ. Predicting the Future - Big Data, Machine Learning, and Clinical Medicine. N Engl J Med. 2016; 375(13):1216-1219. [8] BONKHOFF AK, GREFKES C. Precision medicine in stroke: towards personalized outcome predictions using artificial intelligence. Brain. 2022;145(2):457-475. [9] WANG W, RUDD AG, WAN Y, et al. Risk prediction of 30-day mortality after stroke using machine learning: a nationwide registry-based cohort study. BMC Neurol. 2022;22(1):195. [10] WANG W, OTIENO J A, ERIKSSON M, et al. Developing and externally validating a machine learning risk prediction model for 30-day mortality after stroke using national stroke registers in the UK and Sweden. BMJ Open. 2023;13(11):e69811. [11] WENG SF, REPS J, KAI J, et al. Can machine-learning improve cardiovascular risk prediction using routine clinical data? PLoS One. 2017;12(4):e174944. [12] ORFANOUDAKI A, CHESLEY E, CADISCH C, et al. Machine learning provides evidence that stroke risk is not linear: The non-linear Framingham stroke risk score. PLoS One. 2020;15(5):e232414. [13] KATARIA S, RAVINDRAN V. Electronic health records: a critical appraisal of strengths and limitations. J R Coll Physicians Edinb. 2020;50(3):262-268. [14] REDDY S. Explainability and artificial intelligence in medicine. Lancet Digit Health. 2022;4(4):e214-e215. [15] KUNDU S. AI in medicine must be explainable. Nat Med. 2021;27(8):1328. [16] MORLEY J, MACHADO C, BURR C, et al. The ethics of AI in health care: A mapping review. Soc Sci Med. 2020;260:113172. [17] MOONS KG, DE Groot JA, BOUWMEESTER W, et al. Critical appraisal and data extraction for systematic reviews of prediction modelling studies: the CHARMS checklist. PLoS Med. 2014;11(10):e1001744. [18] WOLFF RF, MOONS K, RILEY RD, et al. PROBAST: A Tool to Assess the Risk of Bias and Applicability of Prediction Model Studies. Ann Intern Med. 2019;170(1):51-58. [19] OTIENO JA, HÄGGSTRÖM J, DAREHED D, et al. Developing machine learning models to predict multi-class functional outcomes and death three months after stroke in Sweden. PLoS One. 2024;19(5):e303287. [20] OZKARA BB, KARABACAK M, HOSEINYAZDI M, et al. Utilizing imaging parameters for functional outcome prediction in acute ischemic stroke: A machine learning study. J Neuroimaging. 2024;34(3):356-365. [21] WEI L, PAN X, DENG W, et al. Predicting long-term outcomes for acute ischemic stroke using multi-model MRI radiomics and clinical variables. Front Med (Lausanne). 2024;11:1328073. [22] 赖海芳, 顾琳, 纵亚, 等. 采用多层感知器神经网络构建亚急性期缺血性脑卒中患者短期预后的预测模型[J]. 中国康复理论与实践,2022,28(3):335-339. [23] HERZOG L, KOOK L, HAMANN J, et al. Deep Learning Versus Neurologists: Functional Outcome Prediction in LVO Stroke Patients Undergoing Mechanical Thrombectomy. Stroke. 2023;54(7):1761-1769. [24] CHEN YW, LIN KC, Li YC, et al. Predicting patient-reported outcome of activities of daily living in stroke rehabilitation: a machine learning study. J Neuroeng Rehabil. 2023;20(1):25. [25] QU S, ZHOU M, JIAO S, et al. Optimizing acute stroke outcome prediction models: Comparison of generalized regression neural networks and logistic regressions. PLoS One. 2022;17(5):e267747. [26] THAKKAR HK, LIAO WW, WU CY, et al. Predicting clinically significant motor function improvement after contemporary task-oriented interventions using machine learning approaches. J Neuroeng Rehabil. 2020;17(1):131. [27] LIANG Y, LI Q, CHEN P, et al. Comparative Study of Back Propagation Artificial Neural Networks and Logistic Regression Model in Predicting Poor Prognosis after Acute Ischemic Stroke. Open Med (Wars). 2019; 14:324-330. [28] XIE Y, JIANG B, GONG E, et al. JOURNAL CLUB: Use of Gradient Boosting Machine Learning to Predict Patient Outcome in Acute Ischemic Stroke on the Basis of Imaging, Demographic, and Clinical Information. AJR Am J Roentgenol. 2019; 212(1):44-51. [29] PARK D, JEONG E, KIM H, et al. Machine Learning-Based Three-Month Outcome Prediction in Acute Ischemic Stroke: A Single Cerebrovascular-Specialty Hospital Study in South Korea. Diagnostics (Basel). 2021;11(10):1909. [30] JO H, KIM C, GWON D, et al. Combining clinical and imaging data for predicting functional outcomes after acute ischemic stroke: an automated machine learning approach. Sci Rep. 2023;13(1):16926. [31] OZKARA BB, KARABACAK M, HAMAM O, et al. Prediction of Functional Outcome in Stroke Patients with Proximal Middle Cerebral Artery Occlusions Using Machine Learning Models. J Clin Med. 2023;12(3):839. [32] LI X, PAN X, JIANG C, et al. Predicting 6-Month Unfavorable Outcome of Acute Ischemic Stroke Using Machine Learning. Front Neurol. 2020;11:539509. [33] JIANG B, ZHU G, XIE Y, et al. Prediction of Clinical Outcome in Patients with Large-Vessel Acute Ischemic Stroke: Performance of Machine Learning versus SPAN-100. AJNR Am J Neuroradiol. 2021;42(2):240-246. [34] 叶倩, 杨云, 徐文韬, 等. 基于可解释机器学习构建脑卒中患者日常生活自理能力风险预测模型[J]. 南京医科大学学报(自然科学版),2024,44(5):672-680. [35] OZKARA BB, KARABACAK M, KOTHA A, et al. Development of machine learning models for predicting outcome in patients with distal medium vessel occlusions: a retrospective study. Quant Imaging Med Surg. 2023;13(9):5815-5830. [36] FENG X, HUA Y, ZOU J, et al. Intelligible Models for HealthCare: Predicting the Probability of 6-Month Unfavorable Outcome in Patients with Ischemic Stroke. Neuroinformatics. 2022;20(3):575-585. [37] ROY-O’REILLY M, MCCULLOUGH LD. Age and Sex Are Critical Factors in Ischemic Stroke Pathology. Endocrinology. 2018; 159(8):3120-3131. [38] GALLIZIOLI M, ARBAIZAR-ROVIROSA M, BREA D, et al. Differences in the post-stroke innate immune response between young and old. Semin Immunopathol. 2023;45(3):367-376. [39] KWAH LK, DIONG J. National Institutes of Health Stroke Scale (NIHSS). J Physiother. 2014;60(1):61. [40] COMER AR, TEMPLETON E, GLIDDEN M, et al. National Institutes of Health Stroke Scale (NIHSS) scoring inconsistencies between neurologists and emergency room nurses. Front Neurol. 2022;13:1093392. [41] NAM D, CHAPIRO J, PARADIS V, et al. Artificial intelligence in liver diseases: Improving diagnostics, prognostics and response prediction. JHEP Rep. 2022;4(4):100443. [42] SAMAD MD, ABRAR S, DIAWARA N. Missing Value Estimation using Clustering and Deep Learning within Multiple Imputation Framework. Knowl Based Syst. 2022;249:108968. |
| [1] | Wang Mi, Ma Shujie, Liu Yang, Qi Rui. Identification and validation of characterized gene NFE2L2 for ferroptosis in ischemic stroke [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1466-1474. |
| [2] | Gao Yang, Qin Hewei, Liu Dandan. ACSL4 mediates ferroptosis and its potential role in atherosclerotic cardiovascular disease [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1239-1247. |
| [3] | Liu Zan, An Ran, Li Baocheng. Effect of pravastatin on functional recovery from sciatic nerve crush injury in rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 942-950. |
| [4] | Wang Xuesong, Wang Yue, Xu Yan, Zeng Wenhui, Lu Wenming, Tang Xingkun, Chen Wenjie, Ye Junsong. Brain-computer interface combined with different therapies for limb dysfunction in stroke patients: effectiveness and mechanism analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6538-6546. |
| [5] | Wang He, Yu Shaohong, . Meta-analysis of transcranial direct current stimulation in improving lower limb motor dysfunction in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6556-6565. |
| [6] | Ping Xingfeng, Huang Zongxuan, Li Kai, Xie Guangmin, Lyu Junying. Regularity of prescriptions for ischemic stroke based on latent structure combined with association rules [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6277-6284. |
| [7] | Yu Bingbing, Wang Tingting, Fang Junlin, Guo Yun, Huang Yingru. Acupuncture for treatment of postmenopausal osteoporosis: meta-analysis, systematic evaluation and trial sequential analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6305-6316. |
| [8] | Wang Zhifeng, Yang Jiao, Xi Yujiang, Xu Shuangfeng, Shi Ting, Lan Junfeng, Hao Zhihui, He Pengfen, Yang Aiming, Pan Pan, Wang Jian. Biomarkers affecting the progression of mild to moderate cognitive impairment after stroke: #br# a non-targeted metabolomics analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5116-5126. |
| [9] | Cao Haijie, Song Huijie, Sun Yalu, Zhang Guangyou, Li Xiang. A wearable exoskeleton with posture feedback improves abnormal gait in patients with stroke [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5127-5133. |
| [10] | Deng Yiran, Wang Xianliang, Li Dandan. Meta-analysis of exercise intervention on cardiopulmonary function in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5203-5211. |
| [11] | Hu Tong, Li Xuan, Yuan Jing, Wang Wei. Different electromagnetic stimulation programs improve post-stroke dysphagia: a network Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5224-5236. |
| [12] | Lin Huijie, Huang Yun, Huang Zhihua, Jiang Lixia. Hot topics on exosomes as drug delivery system in central nervous system diseases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(23): 5013-5021. |
| [13] | Zhang Qiming, Liao Di, Zhong Zhiliang, Lin Lihua, Zheng Xiang, Li Qiong, Shan Sharui. Effect of deep muscle stimulation combined with electromyographic biofeedback on the spasms of the triceps surae and gait changes after stroke [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(2): 385-392. |
| [14] | Wang Ruikun, Gao Weijuan, Zhang Haoran, Liu Yijie, Bu Jiaxin, Yuan Mei, Qin Yuxin, Zhang Yi. Effects of Buyang Huanwu Tang and its main components on pyroptosis in brain tissue of rats with middle cerebral artery occlusion and reperfusion [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(18): 3819-3825. |
| [15] | Wang Ke, Wang Lei, Li Wenshan, Gong Weijun . Application prospect of brain-computer interface technology in the rehabilitation of lower limb function in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(14): 3027-3033. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||