Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (27): 5802-5809.doi: 10.12307/2025.836
Previous Articles Next Articles
Computer simulation analysis of medial tibial stress during running
Sun Yuan1, Yang Chen2, 3, Ma Yunchao1
- 1College of PE and Sports, Beijing Normal University, Beijing 100875, China; 2College of Sports and Health, Shandong Sport University, Jinan 250100, Shandong Province, China; 3College of Physical Education and Sports Science, Qufu Normal University, Qufu 273100, Shandong Province, China
-
Received:2024-07-12Accepted:2024-08-24Online:2025-09-28Published:2025-03-05 -
Contact:Ma Yunchao, MD, Associate professor, College of PE and Sports, Beijing Normal University, Beijing 100875, China -
About author:Sun Yuan, Master candidate, College of PE and Sports, Beijing Normal University, Beijing 100875, China -
Supported by:Ministry of Education Humanities and Social Sciences Research Youth Project, No. 19YJC890030 (to MYC); Beijing Social Science Fund, No. 22YTB009 (to MYC)
CLC Number:
Cite this article
Sun Yuan, Yang Chen, Ma Yunchao. Computer simulation analysis of medial tibial stress during running[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5802-5809.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

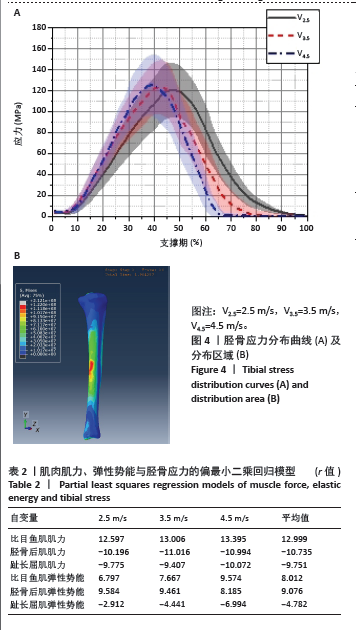
2.4 胫骨应力分布区域及水平 由图4可以发现,胫骨应力集中区域在胫骨远端内侧缘,与文献中报道的患者经常感觉到疼痛的区域接近[19-20]。缓冲期(0-50%),胫骨平均应力水平存在任务间的统计学差异(P=0.044,F=3.834,ηp2=0.040),事后比较结果表明,与V2.5相比,V3.5时的胫骨平均应力水平显著增大(P=0.048,F=3.576,Cohen’s d=0.419)。推进期未发现统计学差异(P=0.055,F=1.926,ηp2=0.027)。 2.5 肌力、弹性势能与胫骨应力的回归模型 3块肌肉的肌力、弹性势能水平均值与胫骨应力的偏最小二乘回归结果见表2。结果显示,3种速度下,均是比目鱼肌的肌力与胫骨应力之间的相关性最高,且都为正相关;其次,胫骨后肌肌力与胫骨应力的相关性排名第二,为负相关;最后是趾长屈肌肌力,为负相关。弹性势能方面,胫骨后肌与应力的相关性最大,为正相关;其次是比目鱼肌,为正相关;最后是趾长屈肌,为负相关。 "
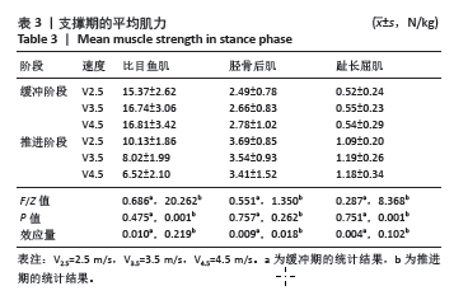
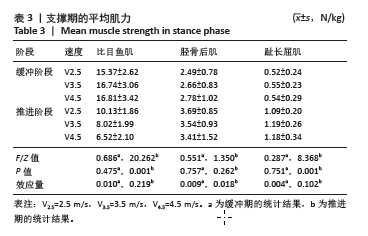
2.6 支撑期内肌肉的肌力变化 缓冲期(1%-50%),比目鱼肌(P=0.475,F=0.686,ηp2=0.010)、胫骨后肌(P=0.757,F=0.551,ηp2=0.009)、趾长屈肌(P=0.751,F=0.287,ηp2=0.004)不存在任务间的统计学差异。推进期(51%-100%),比目鱼肌(P=0.001,F=20.262,ηp2=0.219)、趾长屈肌(P=0.001,F=8.368,ηp2=0.102)的肌力存在任务间的统计学差异,事后检验结果表明,与V2.5相比,V3.5时的比目鱼肌(P < 0.001,Cohen’s d=0.828)肌力显著增大;与V2.5相比,V4.5时的比目鱼肌力显著减少(P < 0.001,Cohen’s d=1.124),趾长屈肌的肌力显著增大(P=0.033,Cohen’s d=0.504)。胫骨后肌的肌力不存在任务间的统计学差异(P=0.262,F=1.350,ηp2=0.018)。见表3。"
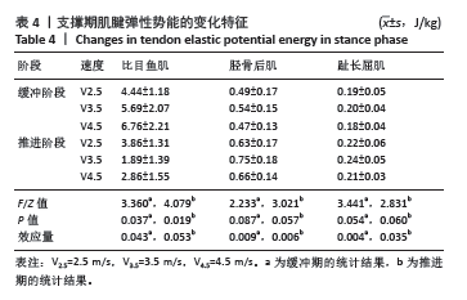
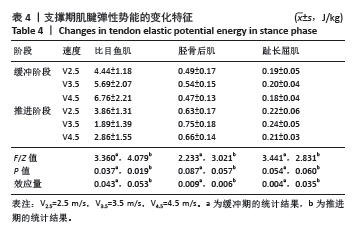
2.7 支撑期内肌肉-肌腱单位中储存的弹性势能变化 缓冲期(1%-50%),比目鱼肌(P=0.037,F=3.360,ηp2=0.043)的弹性势能存在任务间的统计学著差异,事后检验结果显示,与V2.5相比,V4.5时的比目鱼肌(P=0.048,Cohen’s d=0.491)的弹性势能显著增大。胫骨后肌、趾长屈肌的数据不符合正态分布,使用Kruskal-Wallis检验,结果显示,胫骨后肌(P=0.087,χ2=2.233)与趾长屈肌(P=0.054,χ2=3.441)的弹性势能不存在任务间的显著差异。推进期(50%-100%),比目鱼肌(P=0.019,F=4.079,ηp2=0.053)的弹性势能存在任务间的统计学差异,事后检验结果显示,与V2.5相比,V4.5时比目鱼肌(P=0.048,Cohen’s d=0.528)的弹性势能显著减少。胫骨后肌、趾长屈肌的数据不符合正态分布,对它们使用了Kruskal-Wallis检验,结果显示,胫骨后肌(P=0.057,χ2=3.021)、趾长屈肌的弹性势能(P=0.060,χ2=2.831)不存在任务间的统计学差异。见表4。 2.8 不良事件 此次试验实施过程中无不良事件发生。"
| [1] BLIEKENDAAL S, MOEN M, FOKKER Y, et al. Incidence and risk factors of medial tibial stress syndrome: a prospective study in Physical Education Teacher Education students. BMJ Open Sport Exerc Med. 2018;4(1):e000421. [2] REINKING MF, AUSTIN TM, RICHTER RR, et al. Medial tibial stress syndrome in active individuals: a systematic review and meta-analysis of risk factors. Sports Health. 2017;9(3):252-261. [3] MATTOCK JPM, STEELE JR, MICKLE KJ. Are Leg Muscle, Tendon and Functional Characteristics Associated with Medial Tibial Stress Syndrome? A Systematic Review. Sports Med Open. 2021;7(1):71. [4] BECKER J, JAMES S, WAYNER R, et al. Biomechanical Factors Associated With Achilles Tendinopathy and Medial Tibial Stress Syndrome in Runners. Am J Sports Med. 2017;45(11):2614-2621. [5] NADERI A, MOEN MH, DEGENS H. Is high soleus muscle activity during the stance phase of the running cycle a potential risk factor for the development of medial tibial stress syndrome? A prospective study. J Sports Sci. 2020;38(20):2350-2358. [6] BOUCHÉ RT, JOHNSON CH. Medial tibial stress syndrome (tibial fasciitis): a proposed pathomechanical model involving fascial traction. J Am Podiatr Med Assoc. 2007;97(1):31-36. [7] FRANKLYN M, OAKES B, FIELD B, et al. Section Modulus is the Optimum Geometric Predictor for Stress Fractures and Medial Tibial Stress Syndrome in both Male and Female Athletes. Am J Sports Med. 2008; 36(6):1179-1189. [8] XU C, SILDER A, ZHANG J, et al. An Integrated Musculoskeletal-Finite-Element Model to Evaluate Effects of Load Carriage on the Tibia During Walking. J Biomech Eng. 2016;138(10). doi: 10.1115/1.4034216. [9] XIONG B, YANG P, LIN T, et al. Changes in hip joint contact stress during a gait cycle based on the individualized modeling method of “gait-musculoskeletal system-finite element”. J Orthop Surg Res. 2022;17(1): 267. [10] BEGUE J, PEYROT N, DALLEAU G, et al. Age-related changes in the control of whole-body angular momentum during stepping. Exp Gerontol. 2019;127:110714. [11] HERMENS HJ, FRERIKS B, DISSELHORST-KLUG C, et al. Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol. 2000;10(5):361-374. [12] HUENAERTS C, DEWIT T, SOENTJENS D, et al. Differences in surface electrode placement and its effect on duration of EMG activity. Gait Posture. 2022;97:S7-S8. [13] HOUGLUM P. Therapeutic Exercise for Musculoskeletal Injuries. Human Kinetics Publishers, 2016. [14] CARBONE V, FLUIT R, PELLIKAAN P, et al. TLEM 2.0 – A comprehensive musculoskeletal geometry dataset for subject-specific modeling of lower extremity. J Biomech. 2015;48(5):734-741. [15] YE B, LIU G, HE Z, et al. Biomechanical mechanisms of anterior cruciate ligament injury in the jerk dip phase of clean and jerk: A case study of an injury event captured on-site. Heliyon. 2024;10(11):e31390. [16] ÜN K, ÇALIK A. Relevance of inhomogeneous–anisotropic models of human cortical bone: a tibia study using the finite element method. Biotechnol Biotechnol Equip. 2016;30(3):538-547. [17] O’ROURKE D, BUCCI F, BURTON WS, et al. Determining the relationship between tibiofemoral geometry and passive motion with partial least squares regression. J Orthop Res. 2023;41(8):1709-1716. [18] CICCHETTI D. Guidelines, Criteria, and Rules of Thumb for Evaluating Normed and Standardized Assessment Instrument in Psychology. Psychol Assess. 1994;6:284-290. [19] BROWN AA. Medial Tibial Stress Syndrome: Muscles Located at the Site of Pain. Scientifica (Cairo). 2016;2016:7097489. [20] LOVALEKAR M, HAURET K, ROY T, et al. Musculoskeletal injuries in military personnel—Descriptive epidemiology, risk factor identification, and prevention. J Sci Med Sport. 2021;24(10):963-969. [21] GOLDMANN JP, BRÜGGEMANN GP. The potential of human toe flexor muscles to produce force. J Anat. 2012;221(2):187-194. [22] HONEINE JL, SCHIEPPATI M, GAGEY O, et al. The functional role of the triceps surae muscle during human locomotion. PLoS One. 2013;8(1): e52943. [23] LAI A, SCHACHE AG, LIN YC, et al. Tendon elastic strain energy in the human ankle plantar-flexors and its role with increased running speed. Exp Biol. 2014;217(17): 3159-3168. [24] NEPTUNE RR, SASAKI K. Ankle plantar flexor force production is an important determinant of the preferred walk-to-run transition speed. J Exp Biol. 2005;208(Pt 5):799-808. [25] BOHM S, MERSMANN F, SCHROLL A, et al. Speed-specific optimal contractile conditions of the human soleus muscle from slow to maximum running speed. J Exp Biol. 2023;226(22):jeb246437. [26] DERRICK TR, HAMILL J, CALDWELL GE. Energy absorption of impacts during running at various stride lengths. Med Sci Sports Exerc. 1998; 30(1):128-135. [27] BLAZEVICH AJ, FLETCHER JR. More than energy cost: multiple benefits of the long Achilles tendon in human walking and running. Biol Rev. 2023;98(6):2210-2225. [28] EDAMA M, ONISHI H, KUBO M, et al. Gender differences of muscle and crural fascia origins in relation to the occurrence of medial tibial stress syndrome. Scand J Med Sci Sports. 2017;27(2):203-208. [29] BECK BR, OSTERNIG LR. Medial tibial stress syndrome. The location of muscles in the leg in relation to symptoms. J Bone Joint Surg Am. 1994;76(7):1057-1061. [30] ZHANG H, PENG W, QIN C, et al. Lower Leg Muscle Stiffness on Two-Dimensional Shear Wave Elastography in Subjects With Medial Tibial Stress Syndrome. J Ultrasound Med. 2022;41(7):1633-1642. [31] SAEKI J, NAKAMURA M, NAKAO S, et al. Muscle stiffness of posterior lower leg in runners with a history of medial tibial stress syndrome. Scand J Med Sci Sports. 2018;28(1):246-251. [32] KOVÁCS B, KÓBOR I, GYIMES Z, et al. Lower leg muscle-tendon unit characteristics are related to marathon running performance. Sci Rep. 2020;10(1):17870. [33] YE D, LI L, ZHANG S, et al. Acute effect of foot strike patterns on in vivo tibiotalar and subtalar joint kinematics during barefoot running. J Sport Health Sci. 2024;13(1):108-117. [34] LI J, SONG Y, XUAN R, et al. Effect of long-distance running on inter-segment foot kinematics and ground reaction forces: A preliminary study. Front Bioeng Biotechnol. 2022;10:833774. [35] NOH B, MASUNARI A, AKIYAMA K, et al. Structural deformation of longitudinal arches during running in soccer players with medial tibial stress syndrome. Eur J Sport Sci. 2015;15(2):173-181. [36] MORGAN KD, DONNELLY CJ, REINBOLT JA. Elevated gastrocnemius forces compensate for decreased hamstrings forces during the weight-acceptance phase of single-leg jump landing: implications for anterior cruciate ligament injury risk. J Biomech. 2014;47(13):3295-3302. [37] ZHANG H, PENG W, QIN C, et al. Lower leg muscle stiffness on two‐dimensional shear wave elastography in subjects with medial tibial stress syndrome. J Ultrasound Med. 2022;41(7):1633-1642. [38] SAKAMOTO K, SASAKI M, TSUJIOKA C, et al. An elastic foot orthosis for limiting the increase of shear modulus of lower leg muscles after a running task: A randomized crossover trial. Int J Environ Res Public Health. 2022;19(22):15212. [39] OHYA S, NAKAMURA M, AOKI T, et al. The effect of a running task on muscle shear elastic modulus of posterior lower leg. J Foot Ankle Res. 2017;10:56. [40] POHL MB, RABBITO M, FERBER R. The role of tibialis posterior fatigue on foot kinematics during walking. J Foot Ankle Res. 2010;3:6. [41] REEVES J, JONES R, LIU A, et al. The immediate effects of foot orthosis geometry on lower limb muscle activity and foot biomechanics. J Biomech. 2021;128:110716. |
| [1] | Liu Wenlong, Dong Lei, Xiao Zhengzheng, Nie Yu. Finite element analysis of tibial prosthesis loosening after fixed-bearing unicompartmental knee arthroplasty for osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2191-2198. |
| [2] | Zheng Wangyang, Fei Ji, Yang Di, Zhao Lang, Wang Lingli, Liu Peng, Li Haiyang. Finite element analysis of the force changes of the supraspinatus tendon and glenohumeral joint during the abduction and flexion of the humerus [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2199-2207. |
| [3] | Cai Qirui, Dai Xiaowei, Zheng Xiaobin, Jian Sili, Lu Shaoping, Liu Texi, Liu Guoke, Lin Yuanfang. Mechanical effects of Long’s traction orthopedic method on cervical functional units: quantitative analysis of biomechanical model of head and neck [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2208-2216. |
| [4] | Rao Jingcheng, Li Yuwan, Zheng Hongbing, Xu Zhi, Zhu Aixiang, Shi Ce, Wang Bing, Yang Chun, Kong Xiangru, Zhu Dawei. Biomechanical differences between the new proximal femoral stable intramedullary nail and traditional intramedullary nail#br# [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2217-2225. |
| [5] | Chen Long, Wang Xiaozhen, Xi Jintao, Lu Qilin. Biomechanical performance of short-segment screw fixation combined with expandable polyetheretherketone vertebral body replacement in osteoporotic vertebrae [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2226-2235. |
| [6] | Chen Huiting, Zeng Weiquan, Zhou Jianhong, Wang Jie, Zhuang Congying, Chen Peiyou, Liang Zeqian, Deng Weiming. Tail anchoring technique of vertebroplasty in treatment of osteoporotic vertebral compression fractures with intravertebral cleft: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2145-2152. |
| [7] | Cheng Qisheng, Julaiti·Maitirouzi, Xiao Yang, Zhang Chenwei, Paerhati·Rexiti. Finite element analysis of novel variable-diameter screws in modified cortical bone trajectory of lumbar vertebrae [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2162-2171. |
| [8] | Liu Jiafu, Ren Ruxia, Liao Zhouwei, Zhou Xiali, Wu Yihong, Zhang Shaoqun. Three-dimensional finite element analysis of cervical spine biomechanical characteristics in a rat model of cervical vertigo [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2182-2190. |
| [9] | Zheng Xuying, Hu Hongcheng, Xu Libing, Han Jianmin, Di Ping. Stress magnitude and distribution in two-piece cement-retained zirconia implants under different loading conditions and with varying internal connection shapes [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1979-1987. |
| [10] | Zhong Caihong, Xiao Xiaoge, Li Ming, Lin Jianhong, Hong Jing. Biomechanical mechanism of sports-related patellar tendinitis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1417-1423. |
| [11] | Xu Hao, Ding Lu, Li Xiao. Mechanical effect of mechanical wear of abutment screws on the Morse taper connection implant system: a three-dimensional finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1375-1383. |
| [12] | Shang Depeng, Wei Haiyu, Yang Fan. Finite element analysis for three different types of internal screw fixation in treatment of severe lumbar 1 vertebral body fractures [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 537-545. |
| [13] | Yu Xinlin, Chen Huiyu, Wang Yingying, Guo Weizhong, Feng Bin Lin Chengshou, Lin Wang. Finite element analysis of internal fixation with new retrograde intramedullary nail on lateral femur condyle for distal type A2 femur fractures [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 546-552. |
| [14] | Zhao Jingang, Liu Liping, Chen Jianwei, . Finite element analysis comparing lumbar fusion and artificial intervertebral disc replacement [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 553-560. |
| [15] | Wang Meng, Lu Tan, Li Minjie, Liu Zhicheng, Guo Xiaoyong. Finite element analysis of stress distribution of anchors at different implantation depths under different bone density conditions in rotator cuff tears [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 561-569. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||