Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (15): 3271-3279.doi: 10.12307/2025.175
Previous Articles Next Articles
Classification and advantages and disadvantages of orthopedic robots in clinical applications
Sun Chengjie, Zhang Deqiang
- First Affiliated Hospital of Dalian Medical University, Dalian 116000, Liaoning Province, China
-
Received:2024-02-27Accepted:2024-04-30Online:2025-05-28Published:2024-11-06 -
Contact:Zhang Deqiang, MD, Professor, First Affiliated Hospital of Dalian Medical University, Dalian 116000, Liaoning Province, China -
About author:Sun Chengjie, First Affiliated Hospital of Dalian Medical University, Dalian 116000, Liaoning Province, China
CLC Number:
Cite this article
Sun Chengjie, Zhang Deqiang. Classification and advantages and disadvantages of orthopedic robots in clinical applications[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(15): 3271-3279.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
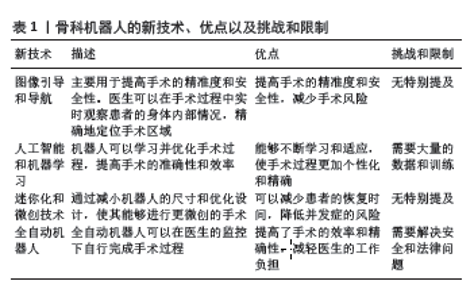
2.1 手术机器人与骨科机器人 通常来讲,手术机器人主要由控制平台、成像系统以及手术机械臂构成[3],其中控制平台中的机器人操作系统是手术机器人的核心。以外科手术中常见的达芬奇机器人为例,其操作系统通过用示指和拇指的指套远距离操纵器来创造熟悉的抓取运动,同时对外科医生的手部运动进行缩放、过滤,并将其转化为达芬奇器械的精确微动[15-16]。 成像系统作为手术机器人获取手术视野的工具是外科机器人手术中不可缺少的一部分。在大部分外科手术中,使用的成像系统是光学变焦成像系统,可以在不移动物体和图像平面的情况下放大手术视野[17]。 手术机械手臂是术中操作的执行者,手术过程中机械臂执行操作的灵活性和稳定性是决定手术成功的关键因素。在手术操作中对机械臂末端反馈灵敏度的要求极高,这需要联合术者的视野、机械臂操作中的力学反馈以及机械臂的稳定性[3]。通过对手术器械的缩小与手术视野的放大,进一步减小术中对患者造成的创伤。 与常见的外科手术机器人注重对软组织进行操作相比,骨科机器人的发展方向有显著的不同,主要体现在以下几个方面:首先,骨科手术,如关节置换和脊柱手术,需要根据每个患者的具体情况进行个性化设计和规划。因此,骨科机器人的发展趋势是向更高程度的个性化手术方向发展,这就要求骨科机器人能够处理大量的个人化数据,包括影像数据和生物力学数据,以实现精准的手术规划和执行。其次,由于骨科手术的复杂性和精细性,骨科机器人需要具备更高的精准度。例如,在脊柱手术中,骨科机器人需要在非常狭小和复杂的空间内进行精准的操作。因此,提高机器人的操作精准度和稳定性成为骨科机器人的重要发展方向。再者,骨科手术通常涉及到各种复杂的骨科疾病和手术方式,这就要求骨科机器人具有更强的适应性。利用人工智能和机器学习技术,使骨科机器人能够学习和适应不同的手术情况和患者情况,是骨科机器人的重要发展方向。最后,骨科机器人的发展方向还包括开发更先进的骨科特定导航系统,这种导航系统可以帮助医生在手术中实时定位,从而提高手术的精准度和安全性[18-21]。见表1。"
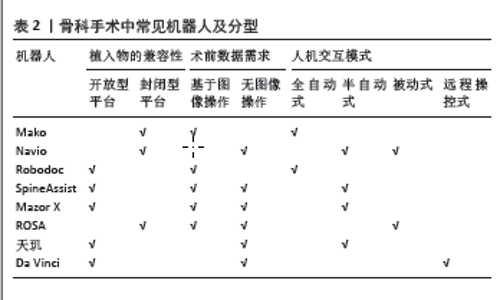
2.2 骨科机器人的分类 依据人机交互模式的不同将机器人分为全自动机器人(通过提前设计的程序来自主执行预先计划的机器人)、半自动机器人(具有约束运动系统的机器人;约束可以由特定的硬件产生,也可以是经过编程的软件)、被动式机器人(无动力和手动驱动的机器人)及远程操控机器人(由机器人持有的工具,由人类远程控制)[1-2,22-24]。 另一个角度而言,基于对植入物的兼容性以及术前影像学资料的需求将机器人系统分为封闭式平台/开放式平台,基于图像操作/无图像操作[24]。对不同厂家的植入物是否兼容是最先需要考虑的问题,封闭式平台意味着机器人仅能使用指定的植入物进行操作而无法使用非指定的植入物。 所有机器人的操作都是基于对患者解剖结构来设计,然而获取这些数据的方式可以是术前检查和或术中测量。应用图像操作系统的机器人需要对患者进行影像学检查获取所需的资料,通过将已获取的影像学数据输入到工作站设计术前计划,其主要缺点是增加了手术成本以及CT成像过程有关的并发症。无图像则是指患者的相关数据以及手术计划是由术中医生测量和设计,虽然减少了手术成本和避免了CT成像过程的辐射暴露,但是也可能导致手术操作准确性的下降。然而对于骨科患者而言,术前行相关的影像学检查是极其必要的,医生需要通过观看患者影像学资料来判断患者病情的严重程度并设计患者的手术计划。机器人具体分型见表2。"
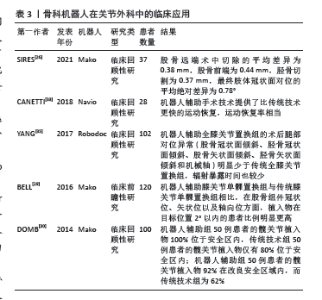
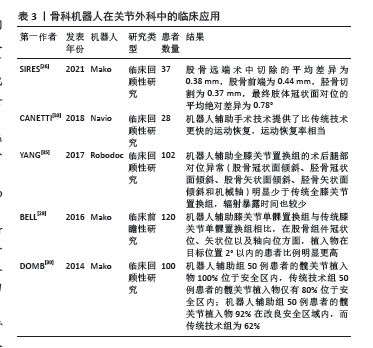
2.3 骨科机器人在骨科的临床应用 2.3.1 骨科机器人在关节外科的临床应用 在关节外科相关手术中常需要机器人辅助的手术包括膝关节置换以及全髋关节置换。这些手术往往需要术前测量患者置换关节的数据,设计患者关节的三维立体结构,比对人工关节能否准确地替换,确保人工关节长久的寿命;同时术中需要精准的操作,避免置换关节过程中出现周围组织的损伤。关节外科手术与其他骨科手术不同的是,手术中需要选择合适的人工假体。由于人工假体的特殊性,仅关节外科机器人存在上文提及的封闭型平台的骨科机器人。目前临床上常见的辅助关节置换的机器人包括Mako、Navio以及Robodoc。 Mako (Stryker Mako Surgical Corporation, Fort Lauder dale, FL)机器人最初由MAKO外科公司开发,于2008年获得美国食品和药物管理局批准[25]。Mako机器人通过术前获取患者数据,提前设计需要被切除的患者骨骼组织的参数以及三维立体空间模型来确定植入物的大小和方位,解决术中可能出现的关节线错位、植入物尺寸、放置不协调和间隙不平衡等问题,从而减少手术并发症并提高植入物的长期存活率[26-28]。SIRES等[26]发现应用Mako机器人可以提高切割骨骼的准确性。BELL等[29]对120例患者进行前瞻性随机分组研究,结果表明在机器人的协助下,切割股骨与胫骨的误差有统计学意义上的降低。DOMB等[30]对100例接受全髋关节置换的患者进行回顾性对比研究,结果发现使用机器人可以获得远超于传统技术的准确率;其中机器人辅助组50例患者的髋关节植入物100%位于安全区内,而传统技术组50例患者的髋关节植入物仅有80%位于安全区内(P=0.001);机器人辅助组50例患者的髋关节植入物92%在改良安全区域内,而传统技术组为62%(P=0.001)。 Navio(Blue Belt Technologies,Plymouth,MN)有一个可伸缩的钻头,通过红外摄像机来构建导航系统,它可以与目前有不同的假体系统一起使用,予以医生更多的选择[31-32]。CANETTI等[33]对28例接受膝关节单髁置换术的患者进行回顾性分析,分析发现机器人辅助手术组患者较传统技术组患者有着更快的运动恢复效果,但运动恢复率相当。 Robodoc (Curexo Technology Corporation,Fremont,CA)是第一个用于关节置换手术的机器人手臂和软件系 统[25]。通过患者术前电子计算机断层扫描的图像设计出术前计划,并在术中将导航针置于患者手术处,进行CT扫描将数据导入到名为ORTHODOC的计算机工作站,自动构建患者三维立体关节挑选合适大小的假体,保证手术的成功[34-36]。YANG等[35]对102例进行全膝关节置换的患者进行回顾性分析,发现虽然两组的临床结果和长期生存率相似;但在放射学结果方面,机器人辅助全膝关节置换组的术后腿部对位异常明显少于传统全膝关节置换组,证明使用Robodoc机器人可以更好地维持患者的生理解剖结构,减轻了患者术后的痛苦,缩短康复所需 时间。 骨科机器人在关节外科中临床应用的汇总表见表3。 "
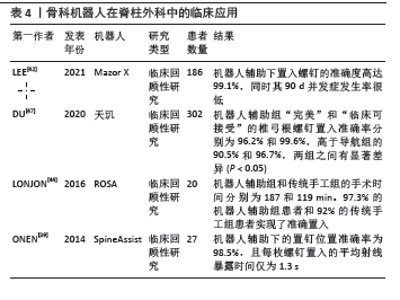
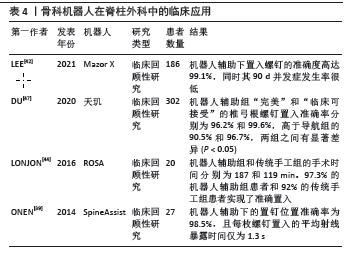
2.3.2 骨科机器人在脊柱外科的临床应用 椎弓根螺钉置入术是脊柱外科中常见的术式,可应用于脊柱骨折、肿瘤、感染、畸形和退行性疾病的治疗,提高脊柱重建后的稳定性。椎弓根螺钉置入术最初是开放式的手术,随着微创技术的出现,微创手术迅速取代了传统开放式的术式。然而应用微创技术进行椎弓根螺钉置入对术者的操作要求更高,存在较高的技术门槛。由于手术量大且手术操作要求高,临床医生有着身体上的劳累和精神上的高度紧张,可能会导致手术风险的增加。然而机器人辅助技术的出现减轻了术者的压力,术者可在术前将患者的影像学资料输入到机器人的系统中,从而设计出患者的术前计划并在术中通过机器人导航系统判断螺钉的位置,依靠机械臂进行螺钉置入来提高操作的准确性和手术的安全。目前脊柱外科手术中常用的机器人包括SpineAssist机器人、Mazor X机器人、天玑机器人、ROSA机器人等。 SpineAssist (Mazor Robotics; Caesareas, Israel) 是并联式半自动机器人,拥有6台电机和6个自由度,在术前需要用一个Hover-T框架固定在骨性标志上,从而维持术中相对位置固定[23,37-38]。ONEN等[39]对27例患者进行回顾性分析,通过置入共计136枚螺钉并对比手术前后影像发现机器人辅助下的置钉位置准确率较传统手工置入明显提高,为98.5%;且每枚螺钉置入的平均射线暴露时间缩短近一半,仅为1.3 s。 Mazor X (Mazor Robotics; Caesareas, Israel) 使用一个带有空间跟踪功能的综合三维摄像机和一个设计为串行而非平行的机器人手臂组成[40-42]。使用该机器人时,是由医生进行椎弓根钻孔操作,通过辅助导航系统来实现术前或术中的手术计划。LEE等[42]通过对186例患者的手术前后影像图像比较,发现Mazor X置入螺钉的准确度高达99.1%,同时其90 d并发症发生率很低(3.8%)。 ROSA (Zimmer Biomet; Warsaw, IN, USA) 是一个自由站立的机器人手术助手,它由一个可在地板上移动的底座和一个坚硬的机器人手臂构成,通过在患者术侧放置经皮参考针,依靠光学追踪设备实现实时跟踪,保证置入螺钉的准确性[40,43-45]。LONJON等[44]通过对20例患者进行回顾性分析,将患者平均分为机器人辅助组和传统手工组,累计置入共90枚椎弓根螺钉。通过数据分析证实了通过使用ROSA机器人可以获得更高的准确率(P < 0.05)。 天玑机器人由一个可移动的6度自由度操纵器系统、一个光学跟踪系统和一个操作平台和导航系统组成[46-49]。DU等[47]通过搜集302例患者的术前术中影像资料进行回顾性分析,将患者分为机器人辅助组与O型臂导航系统辅助组,结果表明机器人组椎弓根螺钉置入准确率为97.9%,导航组为93.6%,两组之间有明显差异(P < 0.05),说明使用天玑机器人可获得更高的准确率。 骨科机器人在脊柱外科中临床应用的汇总表见表4。 "
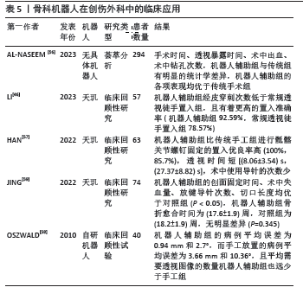
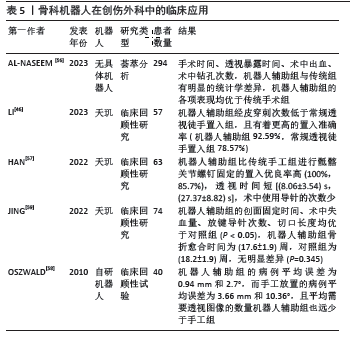
2.3.3 骨科机器人在创伤外科的临床应用 传统的创伤外科手术中往往采取的是完全暴露骨折的部位,导致患者术中出血量、术后感染的可能性增加[50-51]。随着科学技术的发展,人们越发提倡骨科微创技术,相比传统手术具有更高的安全性。然而微创技术也有着明显的缺点:频繁使用C型臂透视对人体的辐射伤害和手术时间的延长等[51-52]。 不稳定骨盆骨折复位固定是创伤手术中难度较高、风险较大的手术之一,致残率高达60%,死亡率超过13%[53]。早期治疗骨盆骨折需要开放性手术治疗,伴随着微创技术的出现,医生们更倾向于对患者损伤程度更小的闭合复位技术[54]。然而临床上采取的C型臂透视二维成像无法完全展示骨折碎片的空间位置,只能采取多方位透视来确定具体位置,导致患者与医生遭受频繁的射线透 视[52,55]。与创伤骨科相关的机器人辅助手术主要是治疗骨盆骨折以及股骨骨折。目前可查阅到用于治疗骨盆骨折的机器人是国产的天玑机器人。相关荟萃分析文献报告了手术时间、透视暴露时间、术中出血、术中钻孔次数,机器人辅助组与传统组有明显的统计学差异,机器人辅助组的各项表现均优于传统手术组[56]。HAN等[57]对63例患者进行回顾性分析,发现机器人辅助比传统手工进行骶髂关节螺钉固定的置入优良率高,透视时间短,术中使用导针的次数少。LI等[46]回顾性分析了57例不稳定性骨盆后环损伤患者的临床资料,发现机器人辅助组经皮穿刺次数低于常规透视徒手组,且有着更高的置入准确率。 自髓内钉面世以来,迅速被应用于股骨干骨折和胫腓骨骨折,然而其使用需要徒手放置远端交锁螺栓,临床操作中往往会出现放置远端交锁螺栓错位等情况,导致患者手术时间、透视暴露时间延长。OSZWALD等[58]对机器人辅助与手工放置远端交锁螺栓进行分析,发现使用机器人辅助的病例平均误差为0.94 mm和2.7°,而手工放置的病例平均误差为3.66 mm和10.36°,且需要透视图像的数量机器人辅助组也远少于手工组。JING等[59]对74例患者进行回顾性分析发现,机器人辅助组有创固定时间、术中出血量、主导针置入次数以及切口长度均优于传统徒手操作组。 骨科机器人在创伤外科中临床应用的汇总表见表5。"
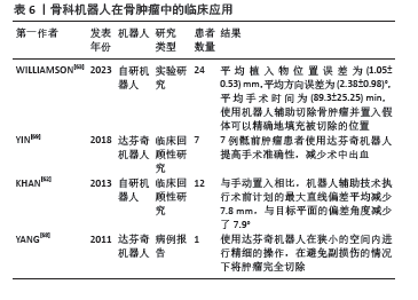
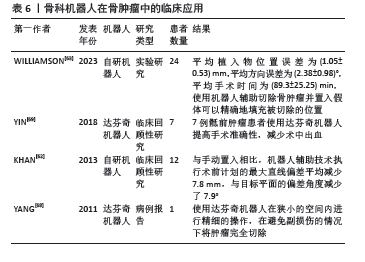
2.3.4 骨科机器人在骨肿瘤的临床应用 骨肿瘤作为一种罕见的疾病,可发生于全年龄段的人身上[60]。骨科医生采取的治疗方式主要是通过患者的影像数据,确定肿瘤的位置以及大小,设计术前计划将肿瘤以及周围部分正常组织完全切割干净[60-63]。然而在传统的骨肿瘤手术中,外科医生采取徒手使用手术器械进行切割时,可能会漏切部分肿瘤组织,或不必要地切除大面积的正常组织。前者的操作失误极有可能导致患者术后骨肿复发瘤,后者则会影响患者术后的恢复[62,64-65]。伴随着手术机器人的迅速发展,机器人辅助技术开始应用于骨肿瘤的手术中。将术前计划导入到机器人辅助系统中有助于外科医生在手术时准确地切割肿瘤组织。虽然机器人可以准确无误地执行术前切割计划,但它在切割的过程中可能会损伤到可变形的软组织结构,如血管和神经。所以目前应用于骨肿瘤手术中的机器人主要为半自动机器人。KHAN等[62]通过设计一种触觉系统的机器人辅助骨肿瘤手术,对12个骨骼标本进行切割,结果表明触觉机器人辅助技术提高了平面切割的准确性。 目前临床上主要应用达芬奇机器人来进行骨肿瘤的切除,达芬奇拥有许多优点,包括较小的切口、减少组织创伤和出血、保护正常的神经血管肌肉组织、减轻患者的术后疼痛[66]。同样重要的是,达芬奇的双目内窥镜提供了三维立体的视觉效果,同时可将视野放大10-20倍,对术者而言意义重大[67]。通过操作达芬奇机器人继续手术也可以解决术者肌肉不自主颤动的问题,避免了手术副损伤。YANG等[68]报告了1例腰椎旁肿瘤切除手术,使用达芬奇机器人在狭小的空间内进行精细的操作,在避免副损伤的情况下将肿瘤完全切除,证明了腹膜后间隙机器人切除术的优越性。YIN等[69]对7例接受达芬奇机器人辅助手术的患者进行回顾性分析,结果表明达芬奇机器人可提供“完美”的手术视野,提高手术准确性,减少术中出血,对患者的损伤更小,有助于患者术后恢复。 同时部分骨肿瘤切除手术中往往需要在切除的位置上置入假体。依据术前计划的切割部分的大小形状,设计合适的假体,术中使用机器人辅助切割骨肿瘤并置入假体可以精确地填充被切除的位置[63]。 骨科机器人在骨肿瘤中临床应用的汇总表见表6。"
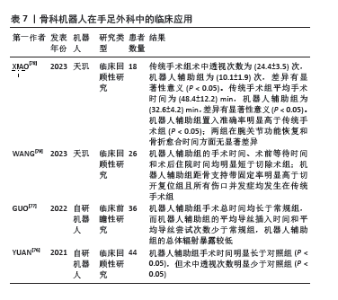
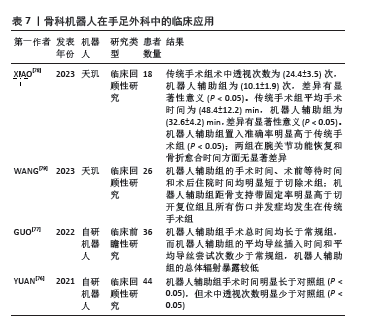
2.3.5 骨科机器人在手足显微外科的临床应用 相比较其他骨科专业,手足显微外科在机器人辅助手术方面的研究较少,相对落后[70]。机器人辅助下行踝关节置换术目前处于研究阶段,大多为尸体测试,距离临床上应用还有一段距离[71-75]。目前机器人辅助技术大多应用在经皮空心螺钉固定手术中[76-79]。WANG等[79]对26例闭合性跟骨骨折患者(28处骨折)进行回顾性分析,发现使用机器人辅助手术的患者手术时间以及住院时间均明显缩短,并且术后4例并发症均出现在传统手工组。XIAO等[78]通过搜集18例舟骨骨折患者的资料进行回顾性分析,发现传统手术组术中透视次数、手术时间远超过机器人辅助组;同时应用机器人辅助还可以获得更高的准确度。 骨科机器人在手足外科中临床应用的汇总表见表7。"
| [1] DAVIES B. A review of robotics in surgery. Proc Inst Mech Eng H. 2000; 214(1):129-140. [2] PARSLEY BS. Robotics in orthopedics: a brave new world. J Arthroplasty. 2018;33(8):2355-2357. [3] ZHANG W, LI H, CUI L, et al. Research Progress and Development Trend of Surgical Robot and Surgical Instrument Arm. Int J Med Robot. 2021;17(5):e2309. [4] RODRÍGUEZ-SANJUÁN JC, GÓMEZ-RUIZ M, TRUGEDA-CARRERA S, et al. Laparoscopic and robot-assisted laparoscopic digestive surgery: present and future directions. World J Gastroenterol. 2016; 22(6):1975-2004. [5] UHRICH M, UNDERWOOD RA, STANDEVEN JW, et al. Assessment of fatigue, monitor placement, and surgical experience during simulated laparoscopic surgery. Surg Endosc. 2002;16:635-639. [6] JUNG M, MOREL P, BUEHLER L, et al. Robotic general surgery: current practice, evidence, and perspective. Langenbecks Arch Surg. 2015;400:283-292. [7] VAN DER HULST R, SAWOR J, BOUVY N. Microvascular anastomosis: is there a role for robotic surgery. J Plast Reconstr Aesthet Surg. 2007; 60(1):101-102. [8] AITZETMÜLLER MM, KLIETZ ML, DERMIETZEL A, et al. Robotic-assisted microsurgery and its future in plastic surgery. J Clin Med. 2022;11(12): 3378. [9] LI HM, ZHANG RJ, SHEN CL. Accuracy of pedicle screw placement and clinical outcomes of robot-assisted technique versus conventional freehand technique in spine surgery from nine randomized controlled trials: a meta-analysis. Spine. 2020;45(2):E111-E119. [10] LIN L, SUN M, XU C, et al. Assessment of robot-assisted mandibular contouring surgery in comparison with traditional surgery: a prospective, single-center, randomized controlled trial. Aesthet Surg J. 2022;42(6):567-579. [11] SHENG S, ZHAO T, WANG X. Comparison of robot-assisted surgery, laparoscopic-assisted surgery, and open surgery for the treatment of colorectal cancer: a network meta-analysis. Medicine. 2018;97(34):e11817. [12] DU Y, LONG Q, GUAN B, et al. Robot-assisted radical prostatectomy is more beneficial for prostate cancer patients: a system review and meta-analysis. Med Sci Monit. 2018;24:272-287. [13] VERONESI G, NOVELLIS P, VOULAZ E, et al. Robot-assisted surgery for lung cancer: State of the art and perspectives. Lung Cancer. 2016; 101:28-34. [14] XIE W, CAO D, YANG J, et al. Robot-assisted surgery versus conventional laparoscopic surgery for endometrial cancer: a systematic review and meta-analysis. J Cancer Res Clin Oncol. 2016;142:2173-2183. [15] JACOFSKY DJ, ALLEN M. Robotics in arthroplasty: a comprehensive review. J Arthroplasty. 2016;31(10):2353-2363. [16] SIMOROV A, OTTE RS, KOPIETZ CM, et al. Review of surgical robotics user interface: what is the best way to control robotic surgery. Surg Endosc. 2012;26:2117-2125. [17] CHENG Y, CAO J, TANG X, et al. Optical zoom imaging systems using adaptive liquid lenses. Bioinspir Biomim. 2021;16(4):041002. [18] EWURUM CH, GUO Y, PAGNHA S, et al. Surgical navigation in orthopedics: workflow and system review. Adv Exp Med Biol. 2018; 1093:47-63. [19] QURESHI S, LU Y, MCANANY S, et al. Three-dimensional intraoperative imaging modalities in Orthop Surg: a narrative review. J Am Acad Orthop Surg. 2014;22(12):800-809. [20] BAUMANN F, BECKER C, FREIGANG V, et al. Imaging, post-processing and navigation: Surgical applications in pelvic fracture treatment. Injury. 2022;53:S16-S22. [21] JOHNSON N. Imaging, navigation, and robotics in spine surgery. Spine. 2016;41:S32. [22] TROCCAZ J, DAGNINO G, YANG GZ. Frontiers of medical robotics: from concept to systems to clinical translation. Annu Rev Biomed Eng. 2019;21:193-218. [23] BERTELSEN A, MELO J, SÁNCHEZ E, et al. A review of surgical robots for spinal interventions. Int J Med Robot. 2013;9(4):407-422. [24] INNOCENTI B, BORI E. Robotics in Orthop Surg: why, what and how. Arch Orthop Trauma Surg. 2021;141:2035-2042. [25] BAUTISTA M, MANRIQUE J, HOZACK WJ. Robotics in total knee arthroplasty. J Knee Surg. 2019;32(7):600-606. [26] SIRES JD, CRAIK JD, WILSON CJ. Accuracy of bone resection in MAKO total knee robotic-assisted surgery. J Knee Surg. 2021;34(7):745-748. [27] BATAILLER C, FERNANDEZ A, SWAN J, et al. MAKO CT-based robotic arm-assisted system is a reliable procedure for total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2021;29(11):3585-3598. [28] ROCHE M. The MAKO robotic-arm knee arthroplasty system. Arch Orthop Trauma Surg. 2021;141:2043-2047. [29] BELL SW, ANTHONY I, JONES B, et al. Improved accuracy of component positioning with robotic-assisted unicompartmental knee arthroplasty: data from a prospective, randomized controlled study. J Bone Joint Surg Am. 2016;98(8):627-635. [30] DOMB BG, EL BITAR YF, SADIK AY, et al. Comparison of robotic-assisted and conventional acetabular cup placement in THA: a matched-pair controlled study. Clin Orthop Relat Res. 2014;472(1):329-336. [31] IÑIGUEZ M, NEGRÍN R, DUBOY J, et al. Robot-assisted unicompartmental knee arthroplasty: increasing surgical accuracy? A cadaveric study. J Knee Surg. 2021;34(6):628-634. [32] BATTENBERG AK, NETRAVALI NA, LONNER JH. A novel handheld robotic-assisted system for unicompartmental knee arthroplasty: surgical technique and early survivorship. J Rob Surg. 2020;14(1): 55-60. [33] CANETTI R, BATAILLER C, BANKHEAD C, et al. Faster return to sport after robotic-assisted lateral unicompartmental knee arthroplasty: a comparative study. Arch Orthop Trauma Surg. 2018;138:1765-1771. [34] BULLOCK EK, BROWN MJ, CLARK G, et al. Robotics in total hip arthroplasty: current concepts. J Clin Med. 2022;11(22):6674. [35] YANG HY, SEON JK, SHIN YJ, et al. Robotic total knee arthroplasty with a cruciate-retaining implant: a 10-year follow-up study. Clin Orthop Surg. 2017;9(2):169. [36] LIOW MHL, CHIN PL, TAY KJD, et al.Early experiences with robot-assisted total knee arthroplasty using the DigiMatch™ ROBODOC® surgical system. Singapore Med J. 2014;55(10):529-534. [37] DEVITO DP, KAPLAN L, DIETL R, et al. Clinical acceptance and accuracy assessment of spinal implants guided with SpineAssist surgical robot: retrospective study. Spine. 2010;35(24):2109-2115. [38] MOLLIQAJ G, SCHATLO B, ALAID A, et al. Accuracy of robot-guided versus freehand fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery. Neurosurg Focus. 2017;42(5):E14. [39] ONEN MR, SIMSEK M, NADERI S. Robotic spine surgery: a preliminary report. Turk Neurosurg. 2014;24(4):512-518. [40] JIANG B, AZAD TD, COTTRILL E, et al. New spinal robotic technologies. Front Med. 2019;13:723-729. [41] KHAN A, SOLIMAN MA, LEE NJ, et al. CT-to-fluoroscopy registration versus scan-and-plan registration for robot-assisted insertion of lumbar pedicle screws. Neurosurg Focus. 2022;52(1):E8. [42] LEE NJ, ZUCKERMAN SL, BUCHANAN IA, et al. Is there a difference between navigated and non-navigated robot cohorts in robot-assisted spine surgery? A multicenter, propensity-matched analysis of 2,800 screws and 372 patients. Spine J. 2021;21(9):1504-1512. [43] LEFRANC M, PELTIER J. Evaluation of the ROSA™ Spine robot for minimally invasive surgical procedures. Expert Rev Med Devices. 2016;13(10):899-906. [44] LONJON N, CHAN-SENG E, COSTALAT V, et al. Robot-assisted spine surgery: feasibility study through a prospective case-matched analysis. Eur Spine J. 2016;25:947-955. [45] AHERN DP, GIBBONS D, SCHROEDER GD, et al. Image-guidance, robotics, and the future of spine surgery. Clin Spine Surg. 2020;33(5): 179-184. [46] LI N, ZHU Z, XIAO C, et al. The efficacy of “TiRobot” orthopaedic robot-assisted VS conventional fluoroscopic percutaneous screw fixation of the sacroiliac joint. Int Orthop. 2023;47(2):351-358. [47] DU J, GAO L, HUANG D, et al. Radiological and clinical differences between Tinavi orthopedic robot and O-arm navigation system in thoracolumbar screw implantation for reconstruction of spinal stability. Med Sci Monit. 2020;26:e924770. [48] WANG JQ, WANG Y, FENG Y, et al. Percutaneous sacroiliac screw placement: a prospective randomized comparison of robot-assisted navigation procedures with a conventional technique. Chin Med J. 2017;130(21):2527-2534. [49] ZHANG RJ, ZHOU LP, ZHANG L, et al. Safety and risk factors of TINAVI robot-assisted percutaneous pedicle screw placement in spinal surgery. J Orthop Surg Res. 2022;17(1):379. [50] KOLODZIEJ P, LEE FS, PATEL A, et al. Biomechanical evaluation of the schuhli nut. Clin Orthop Relat Res. 1998;347:79-85. [51] BAI L, YANG J, CHEN X, et al. Medical robotics in bone fracture reduction surgery: a review. Sensors. 2019;19(16):3593. [52] GOSLING T, WESTPHAL R, HUFNER T, et al. Robot-assisted fracture reduction: A preliminary study in the femur shaft. Med Biol Eng Comput. 2005;43:115-120. [53] ZHAO C, WANG Y, WU X, et al. Design and evaluation of an intelligent reduction robot system for the minimally invasive reduction in pelvic fractures. J Orthop Surg Res. 2022;17(1):205. [54] LODDE MF, KATTHAGEN JC, RIESENBECK O, et al. Trends in the surgical treatment of fractures of the pelvic ring: A nationwide analysis of operations and procedures code (OPS) data between 2005 and 2017. Unfallchirurg. 2021;124:373-381. [55] MATHEW G, HANSON BP. Global burden of trauma: Need for effective fracture therapies. Indian J Orthop. 2009;43(2):111. [56] AL-NASEEM A, SALLAM A, GONNAH A, et al. Robot-assisted versus conventional percutaneous sacroiliac screw fixation for posterior pelvic ring injuries: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2023;33(1):9-20. [57] HAN W, ZHANG T, SU YG, et al. Percutaneous Robot-Assisted versus freehand S2 iliosacral screw fixation in unstable posterior pelvic ring fracture. Orthop Surg. 2022;14(2):221-228. [58] OSZWALD M, WESTPHAL R, KLEPZIG D, et al. Hands-on robotic distal interlocking in intramedullary nail fixation of femoral shaft fractures. Technol Health Care. 2010;18(4-5):325-334. [59] JING Y, ZHANG S, HAN Z, et al. Short-term effectiveness of orthopedic robot-assisted femoral neck system fixation for fresh femoral neck fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2022;36(8): 946-950. [60] HILL D, WILLIAMSON T, LAI CY, et al. Automated elaborate resection planning for bone tumor surgery. Int J Comput Assist Radiol Surg. 2023;18(3):553-564. [61] SAYARI AJ, PARDO C, BASQUES BA, et al. Review of robotic-assisted surgery: what the future looks like through a spine oncology lens. Ann Transl Med. 2019;7(10):224. [62] KHAN F, PEARLE A, LIGHTCAP C, et al. Haptic robot-assisted surgery improves accuracy of wide resection of bone tumors: a pilot study. Clin Orthop Relat Res. 2013;471(3):851-859. [63] WILLIAMSON T, RYAN S, BUEHNER U, et al. Robot-assisted implantation of additively manufactured patient-specific orthopaedic implants: evaluation in a sheep model. Int J Comput Assist Radiol Surg. 2023; 18(10):1783-1793. [64] BACCI G, FERRARI S, MERCURI M, et al. Predictive factors for local recurrence in osteosarcoma 540 patients with extremity tumors followed for minimum 2.5 years after neoadjuvant chemotherapy. Acta Orthop Scand. 1998;69(3):230-236. [65] BACCI G, FORNI C, LONGHI A, et al. Local recurrence and local control of non-metastatic osteosarcoma of the extremities: a 27-year experience in a single institution. J Surg Oncol. 2007;96(2):118-123. [66] TRYBULA SJ, OYON DE, WOLINSKY JP. Robotic tissue manipulation and resection in spine surgery. Neurosurg Clin N Am. 2020;31(1):121-129. [67] MOSKOWITZ RM, YOUNG JL, BOX GN, et al. Retroperitoneal transdiaphragmatic robotic-assisted laparoscopic resection of a left thoracolumbar neurofibroma. JSLS. 2009;13(1):64-68. [68] YANG MS, KIM KN, PENNANT W, et al. Robot-assisted resection of paraspinal Schwannoma. J Korean Med Sci. 2011;26(1):150-153. [69] YIN J, WU H, TU J, et al. Robot-assisted sacral tumor resection: a preliminary study. BMC Musculoskelet Disord. 2018;19:186. [70] STAUFFER TP, KIM BI, GRANT C, et al. Robotic technology in foot and ankle surgery: a comprehensive review. Sensors. 2023;23(2):686. [71] HENRY JK, STURNICK D, ROSENBAUM A, et al. Cadaveric gait simulation of the effect of subtalar arthrodesis on total ankle replacement kinematics. Foot Ankle Int. 2022;43(8):1110-1117. [72] DAOU HE, CALDER JD, STEPHEN JM. Development and validation of a robotic system for ankle joint testing. Med Eng Phys. 2018;62:53-57. [73] SAKAKIBARA Y, TERAMOTO A, TAKAGI T, et al. Effects of the Ankle Flexion Angle during Anterior Talofibular Ligament Reconstruction on Ankle Kinematics, Laxity, and in situ forces of the reconstructed graft. Foot Ankle Int. 2022;43(5):725-732. [74] ZHU G, WANG Z, YUAN C, et al. In vitro study of foot bone kinematics via a custom-made cadaveric gait simulator. J Orthop Surg Res. 2020; 15:1-7. [75] GEBREMESKEL M, SHAFIQ B, UNERI A, et al. Quantification of manipulation forces needed for robot-assisted reduction of the ankle syndesmosis: an initial cadaveric study. Int J Comput Assist Radiol Surg. 2022;17(12):2263-2267. [76] YUAN X, ZHANG B, HU J, et al. A comparative study on internal fixation of calcaneal fractures assisted by robot and traditional open reduction internal fixation. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2021;35(6):729-733. [77] GUO Y, MA W, ZLOTOLOW D, et al. A comparison between robotic-assisted scaphoid screw fixation and a freehand technique for acute scaphoid fracture: a randomized, controlled trial. J Hand Surg Am. 2022;47(12):1172-1179. [78] XIAO C, WEI D, ZHU Z, et al. Robot-assisted vs traditional percutaneous freehand for the scaphoid fracture treatment: a retrospective study. Int Orthop. 2023;47(3):839-845. [79] WANG J, HAN W, SU Y, et al. Comparison of Robot-Assisted Percutaneous Cannulated Screws Versus Open Reduction and Internal Fixation in Calcaneal Fractures. Orthop Surg. 2023;15(3):724-730. [80] GHAEDNIA H, FOURMAN MS, LANS A, et al. Augmented and virtual reality in spine surgery, current applications and future potentials. Spine J. 2021;21(10):1617-1625. [81] SPIRIG JEM, RONER S, LIEBMANN F, et al. Augmented reality-navigated pedicle screw placement: a cadaveric pilot study. Eur Spine J. 2021;30: 3731-3737. [82] 曹旭含,白子兴,孙承颐,等.机器人在骨科手术中应用的可靠性与提升空间[J]. 中国组织工程研究,2020,24(9):1416-1421. |
| [1] | Wei Zhiheng, Guan Tianmin, Liu Qing, Gong Jue, Xiang Xianxiang. Application of 3D printing accurate osteotomy guide combined with the revision of anterior cruciate ligament with abnormally increased posterior slope of tibial plateau [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7130-7136. |
| [2] | Wang Lingcheng, Chen Xi, Yang Shuoyao, Huang Zhoulu, Yang Shunjie, You Mingke, Zhou Kai, , Chen Gang, , Li Jian. Effect of periacetabular osteotomy on pelvic sagittal tilt in developmental dysplasia of hip [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4452-4457. |
| [3] | Niu Yanyan, Zhang Qi, Fan Mingxing. Research and development trends and hot spots of spinal surgical robots for treatment of spinal diseases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4612-4620. |
| [4] | Gao Yang, Gao Yuan, Ma Bingjiang, Yue Hui, Shi Yongxin. Applications and prospects of tissue clearing technology in field of orthopedics [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(15): 3227-3234. |
| [5] | Yuan Jing, Sun Xiaohu, Chen Hui, Qiao Yongjie, Wang Lixin. Digital measurement and analysis of the distal femur in adults with secondary knee valgus deformity [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 881-885. |
| [6] | Ma Chao, Wang Fei, Liu Xiaomin, Wang Ziyun, Xu Kui, Yang Wendong, Feng Wei. Quantification of the objective index of lumbar disc herniation with body surface topography map: three-dimensional angulation of the elastically fixed turning point of the lower back curve [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 924-928. |
| [7] | Xin Daqi, Wang Guoqiang, Han Di, Xing Wenhua, Fu Yu, Zhu Yong, Zhou Yang, Bai Xianming, He Chenyang, Zhao Yan. Finite element simulation surgical modeling of Lenke 3 adult idiopathic scoliosis: modeling evaluation twice in 5 years [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(36): 5755-5763. |
| [8] | Xiong Hengheng, Nie Weizhi. Accurate simulation of stress state in bone joint and related soft tissue injury by three-dimensional finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(36): 5875-5880. |
| [9] | Bi Jingwei, Ren Jiabin, Liu Xin, Sun Ning, Li Rui, Li Yuefei, Sun Zhaozhong. 3D-CT-guided unilateral biportal endoscopic localization of L5 and S1 nerve roots and intervertebral space [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(33): 5283-5289. |
| [10] | Shi Xiaoxiu, Mao Shilong, Liu Yang, Ma Xingshuang, Luo Yanfeng. Comparison of tantalum and titanium (alloy) as orthopedic materials: physical and chemical indexes, antibacterial and osteogenic ability [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 593-599. |
| [11] | Pan Xuan, Zhao Meng, Zhang Xiumei, Zhao Jie, Zhai Yunkai. Research and application of biological three-dimensional printing technology in the field of precision medicine: analysis of Chinese and English literature [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3382-3389. |
| [12] | Jing Jinpeng, Zhang Yue, Liu Xiaomin, Liu Yi. Buyang Huanwu Decoction in prevention of deep venous thrombosis after orthopedic surgery: meta-analysis and trial sequential analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(20): 3267-3274. |
| [13] | Zhong Yuanming, Fu Xiaopeng, Xu Wei, Zhao Qingrui, Huang Yong, Ye Weiquan. Nicardipine controlled hypotension applied to perioperative blood loss in orthopedics: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2930-2937. |
| [14] | Liu Zhengpeng, Wang Yahui, Ming Ying, Sun He. Computer design combined with three-dimensional printing template for spinal orthopedics can improve surgical accuracy and correction effect [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1826-1830. |
| [15] | Zhou Chen, Xing Wenhua. Application advantages of three-dimensional printing technology and finite element analysis in scoliosis correction [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1898-1903. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||