[1] YANG SY, BONIELLO AJ, POORMAN CE, et al. A review of the diagnosis and treatment of atlantoaxial dislocations. Global Spine J. 2014;4(3):197-210.
[2] RUF M, PITZEN T, MEYER C, et al. Atlantoaxial Rotatory Dislocation: Delayed Diagnose Will Result in More Invasive Treatment Options. J Neurol Surg A Cent Eur Neurosurg. 2021;82(1):1-8.
[3] SINGLA R, MANJUNATH N, SHARMA R, et al. Neglected Traumatic Atlantoaxial Rotatory Dislocation in Adult: A Case Report. Int J Spine Surg. 2020;14(1):46-52.
[4] FIORE AJ, HAID RW, RODTS GE, et al. Atlantal lateral mass screws for posterior spinal reconstruction: technical note and case series. Neurosurg Focus. 2002; 12(1):E5.
[5] 吴学元,郝崔培,凌鸣,等.颈后路内固定植骨融合术治疗寰枢椎脱位的疗效分析[J].实用骨科杂志,2022,28(9):821-826.
[6] 谭明生.寰枢椎脱位的中西医治疗[J].中国矫形外科杂志,2022,30(21):1921-1924.
[7] HIRABAYASHI K, MIYAKAWA J, SATOMI K, et al. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Phila Pa 1976). 1981;6(4):354-364.
[8] VERNON H, MIOR S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14(7):409-415.
[9] OLINGER C, BRANSFORD R. Upper Cervical Trauma. Orthop Clin North Am. 2021; 52(4):451-479.
[10] 申庆丰,李凌博,马诗博,等.寰枢椎脱位融合方式的研究进展[J].骨科临床与研究杂志,2022,7(5):315-318.
[11] SUN Y, TAN MS. Research progress of causes and strategies in revision surgery for atlantoaxial dislocation. Zhongguo Gu Shang. 2022;35(5):495-499.
[12] GOEL A, LAHERI V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien). 1994;129(1-2):47-53.
[13] GOEL A. Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine. 2004;1(3):281-286.
[14] ARYAN HE, NEWMAN CB, NOTTMEIER EW, et al. Stabilization of the atlantoaxial complex via C-1 lateral mass and C-2 pedicle screw fixation in a multicenter clinical experience in 102 patients: modification of the Harms and Goel techniques. J Neurosurg Spine. 2008;8(3):222-229.
[15] CHEN Q, BRAHIMAJ BC, KHANNA R, et al. Posterior atlantoaxial fusion: a comprehensive review of surgical techniques and relevant vascular anomalies. J Spine Surg. 2020;6(1):164-180.
[16] SUN Y, TAN MS. Research progress of causes and strategies in revision surgery for atlantoaxial dislocation. Zhongguo Gu Shang. 2022;35(5):495-499.
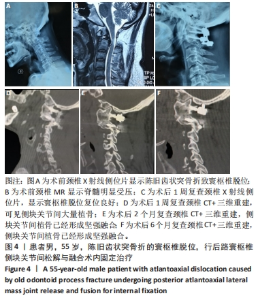
[17] LIU Z, JIAN Q, DUAN W, et al. Atlantoaxial Dislocation with Bony Fusion of C1/2 Facet Joints Treated with Posterior Joint Release, Distraction and Reduction. Spine Surg Relat Res. 2021;6(2):175-180.
[18] GHOSTINE SS, KALOOSTIAN PE, ORDOOKHANIAN C, et al. Improving C1-C2 Complex Fusion Rates: An Alternate Approach. Cureus. 2017;9(11):e1887.
[19] GOREK J, ACAROGLU E, BERVEN S, et al. Constructs incorporating intralaminar C2 screws provide rigid stability for atlantoaxial fixation. Spine (Phila Pa 1976). 2005;30(13):1513-1518.
[20] 孙岩,谭明生.寰枢椎脱位翻修手术原因及策略研究进展[J].中国骨伤, 2022,35(5):495-499.
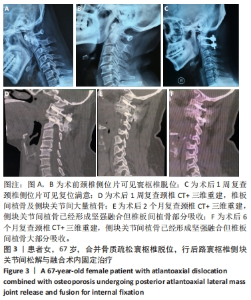
[21] SHEN Q, XIA Y, XU T. Clinical Outcomes of Atlantoaxial Dislocation Combined with Osteoporosis Using Posterior Atlantoaxial Rod, Screw Fixation, and Posterior Interfacet Fusion: A Retrospective Study of 21 Cases. Med Sci Monit. 2020;26:e925187.
[22] SHLOBIN NA, DAHDALEH NS. Cervical spine manifestations of rheumatoid arthritis: a review. Neurosurg Rev. 2021;44(4):1957-1965.
[23] BEN TEKAYA A, REZGUI S, TBINI H, et al. Risk factors for atlantoaxial dislocation in rheumatoid arthritis: A comparative study. Musculoskeletal Care. 2023;21(2): 592-599.
[24] GUAN J, CHEN Z, WU H, et al. Effectiveness of posterior reduction and fixation in atlantoaxial dislocation: a retrospective cohort study of 135 patients with a treatment algorithm proposal. Eur Spine J. 2019;28(5):1053-1063.
[25] 徐韬,甫拉提·买买提,买尔旦·买买提,等.前后联合入路与单纯后路手术治疗难复性寰枢椎脱位型颅底凹陷症的疗效比较[J].中华骨科杂志,2020, 40(18):1255-1265.
[26] YIN YH, QIAO GY, YU XG, et al. Posterior realignment of irreducible atlantoaxial dislocation with C1-C2 screw and rod system: a technique of direct reduction and fixation. Spine J. 2013;13(12):1864-1871.
[27] YAMAZAKI M, OKAWA A, FURUYA T, et al. Anomalous vertebral arteries in the extra- and intraosseous regions of the craniovertebral junction visualized by 3-dimensional computed tomographic angiography: analysis of 100 consecutive surgical cases and review of the literature. Spine (Phila Pa 1976). 2012;37(22):E1389-1397.
[28] MAGKLARA EP, PANTELIA ET, SOLIA E, et al. Vertebral artery variations revised: origin, course, branches and embryonic development. Folia Morphol (Warsz). 2021;80(1):1-12.
[29] LIN X, ZHU HJ, XU Y, et al. Prevalence of Vertebral artery anomaly in upper cervical and its surgical implications: a systematic review. Eur Spine J. 2021;30(12):3607-3613.
[30] HORSFALL HL, GHAROONI AA, AL-MOUSA A, et al. Traumatic atlantoaxial rotatory subluxation in adults - A case report and literature review. Surg Neurol Int. 2020; 11:376.
|