Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (6): 927-933.doi: 10.12307/2023.777
Previous Articles Next Articles
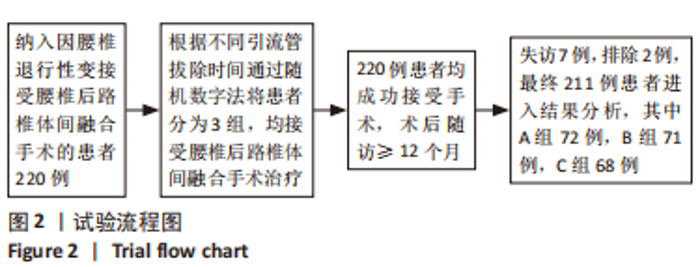
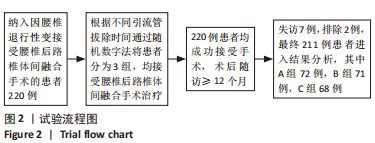
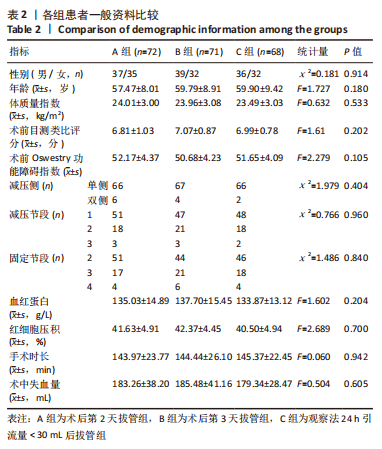
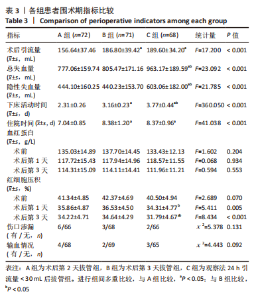
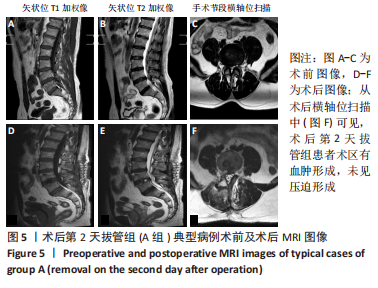
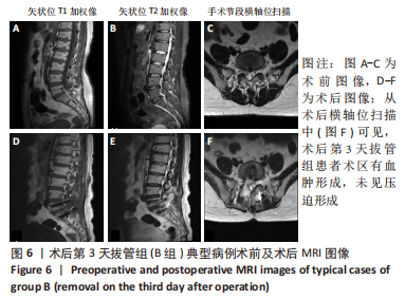
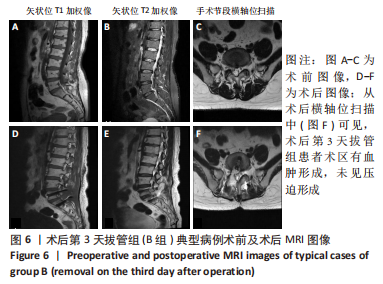
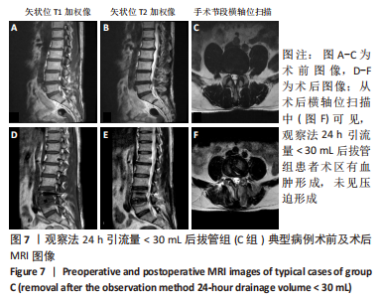
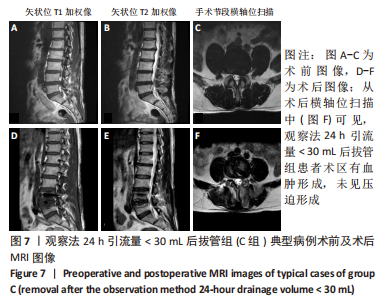
Relationship between drainage time and early efficacy after short-segment lumbar fusion
Chen Zan, Lei Fei, Ye Fei, Zhou Qingzhong, Yuan Hao, Zheng Lipeng, Zha Xian, Feng Daxiong
- Department of Orthopedics, Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China
-
Received:2022-11-15Accepted:2023-01-10Online:2024-02-28Published:2023-07-12 -
Contact:Feng Daxiong, MD, Chief physician, Department of Orthopedics, Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China -
About author:Chen Zan, Master candidate, Department of Orthopedics, Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China
CLC Number:
Cite this article
Chen Zan, Lei Fei, Ye Fei, Zhou Qingzhong, Yuan Hao, Zheng Lipeng, Zha Xian, Feng Daxiong. Relationship between drainage time and early efficacy after short-segment lumbar fusion[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 927-933.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
| [1] BUSER Z, ORTEGA B, D’ORO A, et al. Spine Degenerative Conditions and Their Treatments: National Trends in the United States of America. Global Spine J. 2018;8(1):57-67. [2] FUJITA N, SAKURAI A, MIYAMOTO A, et al. Lumbar spinal canal stenosis leads to locomotive syndrome in elderly patients. J Orthop Sci. 2019;24(1):19-23. [3] PHILLIPS F M, CUNNINGHAM B. Managing chronic pain of spinal origin after lumbar surgery: the role of decompressive surgery. Spine (Phila Pa 1976). 2002; 27(22):2547-2553; discussion 2554. [4] AONO H, OHWADA T, HOSONO N, et al. Incidence of postoperative symptomatic epidural hematoma in spinal decompression surgery. J Neurosurg Spine. 2011; 15(2):202-205. [5] WAUGH TR, STINCHFIELD FE. Suction drainage of orthopaedic wounds. J Bone Joint Surg Am. 1961;43-a:939-946. [6] GROSS JB. Estimating allowable blood loss: corrected for dilution. Anesthesiology. 1983;58(3):277-280. [7] NADLER SB, HIDALGO JH, BLOCH T. Prediction of blood volume in normal human adults. Surgery. 1962;51(2):224-232. [8] SEHAT KR, EVANS RL, NEWMAN JH. Hidden blood loss following hip and knee arthroplasty. Correct management of blood loss should take hidden loss into account. J Bone Joint Surg Br. 2004;86(4):561-565. [9] DIAB M, SMUCNY M, DORMANS JP, et al. Use and outcomes of wound drain in spinal fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2012; 37(11):966-973. [10] VON ECKARDSTEIN KL, DOHMES JE, ROHDE V. Use of closed suction devices and other drains in spinal surgery: results of an online, Germany-wide questionnaire. Eur Spine J. 2016;25(3):708-715. [11] HO C, SUCATO DJ, RICHARDS BS. Risk factors for the development of delayed infections following posterior spinal fusion and instrumentation in adolescent idiopathic scoliosis patients. Spine (Phila Pa 1976). 2007;32(20):2272-2277. [12] OLSEN MA, NEPPLE JJ, RIEW KD, et al. Risk factors for surgical site infection following orthopaedic spinal operations. J Bone Joint Surg Am. 2008;90(1):62-69. [13] LEI Y, HUANG Q, HUANG Z, et al. Multiple-Dose Intravenous Tranexamic Acid Further Reduces Hidden Blood Loss After Total Hip Arthroplasty: A Randomized Controlled Trial. J Arthroplasty. 2018;33(9):2940-2945. [14] XU H, XIE J, LEI Y, et al. Closed suction drainage following routine primary total joint arthroplasty is associated with a higher transfusion rate and longer postoperative length of stay: a retrospective cohort study. J Orthop Surg Res. 2019;14(1):163. [15] LI C, NIJAT A, ASKAR M. No clear advantage to use of wound drains after unilateral total knee arthroplasty: a prospective randomized, controlled trial. J Arthroplasty. 2011;26(4):519-522. [16] PENNINGTON Z, LUBELSKI D, MOLINA C, et al. Prolonged Post-surgical Drain Retention Increases Risk for Deep Wound Infection After Spine Surgery. World Neurosurg. 2019;130:e846-e853. [17] ANDREW GLENNIE R, DEA N, STREET JT. Dressings and drains in posterior spine surgery and their effect on wound complications. J Clin Neurosci. 2015;22(7): 1081-1087. [18] MEREDITH DS, KEPLER CK, HUANG RC, et al. Postoperative infections of the lumbar spine: presentation and management. Int Orthop. 2012;36(2):439-444. [19] VARLEY GW, MILNER S, TURNER GM, et al. Ultrasound assessment of the efficacy of wound drains. J R Coll Surg Edinb. 1994;39(2):97-99. [20] MIRZAI H, EMINOGLU M, ORGUC S. Are drains useful for lumbar disc surgery? A prospective, randomized clinical study. J Spinal Disord Tech. 2006;19(3):171-177. [21] SEN O, KIZILKILIC O, AYDIN MV, et al. The role of closed-suction drainage in preventing epidural fibrosis and its correlation with a new grading system of epidural fibrosis on the basis of MRI. Eur Spine J. 2005;14(4):409-414. [22] KOTILAINEN E, ALANEN A, ERKINTALO M, et al. Magnetic resonance image changes and clinical outcome after microdiscectomy or nucleotomy for ruptured disc. Surg Neurol. 1994;41(6):432-440. [23] GUBIN AV, PRUDNIKOVA OG, SUBRAMANYAM KN, et al. Role of closed drain after multi-level posterior spinal surgery in adults: a randomised open-label superiority trial. Eur Spine J. 2019;28(1):146-154. [24] COBB JP. Why use drains? J Bone Joint Surg Br. 1990;72(6):993-995. [25] CHAHOUD J, KANAFANI Z, KANJ SS. Surgical site infections following spine surgery: eliminating the controversies in the diagnosis. Front Med (Lausanne). 2014;1:7. [26] SMITH JS, SHAFFREY CI, SANSUR CA, et al. Rates of infection after spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976). 2011;36(7):556-563. [27] WILLEMEN D, PAUL J, WHITE SH, et al. Closed suction drainage following knee arthroplasty. Effectiveness and risks. Clin Orthop Relat Res. 1991;(264):232-234. [28] YAMADA T, YOSHII T, EGAWA S, et al. Drain Tip Culture is Not Prognostic for Surgical Site Infection in Spinal Surgery Under Prophylactic Use of Antibiotics. Spine (Phila Pa 1976). 2016;41(14):1179-1184. [29] MACKI M, UZOSIKE A, KEREZOUDIS P, et al. Duration of indwelling drain following instrumented posterolateral fusion of the lumbar spine does not predict surgical site infection requiring reoperation. J Clin Neurosci. 2017;40:44-48. [30] BROWN MD, BROOKFIELD KF. A randomized study of closed wound suction drainage for extensive lumbar spine surgery. Spine (Phila Pa 1976). 2004;29(10): 1066-1068. [31] PATEL SB, GRIFFITHS-JONES W, JONES CS, et al. The current state of the evidence for the use of drains in spinal surgery: systematic review. Eur Spine J. 2017;26(11): 2729-2738. |
| [1] | Jiang Xiaocheng, Shi Lu, Wang Yinbin, Li Qiujiang, Xi Chuangzhen, Ma Zefeng, Cai Lijun. Systematical evaluation of bone fusion rate after interbody fusion in patients with osteoporosis and lumbar degenerative disease treated with teriparatide [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1427-1433. |
| [2] | Guo Zhuotao, Zhang Kai, Zha Guochun, Guo Kaijin. A matched controlled trial of lumbar fusion effect on mid-term outcomes after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(36): 5801-5805. |
| [3] | Niu Feng, Su Baotong, Chen Yulin, Xie Yajuan, Xu Yilang, Li Cong, Cheng Zhian. Establishment of Nomogram prediction model for postoperative blood transfusion in elderly hip fractures using R software [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(31): 4932-4936. |
| [4] | Jin Xinjie, Lu Xiangdong, Zhao Yibo, Zhao Xiaofeng, Qi Detai, Zhao Bin. Endoscopic transforaminal lumbar interbody fusion for degenerative diseases of the lumbar spine: decompression fusion and preservation of posterior spine anatomy [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(27): 4401-4407. |
| [5] | He Shiping, Jia Dazhou, Li Xiaolei, Wang Qiang. Establishment of prediction model of blood transfusion after proximal femoral nail anti-rotation fixation of femoral intertrochanteric fracture in elderly adults [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 929-933. |
| [6] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [7] | Chen Chaofeng, He Dadong, Liang Jincheng, He Zhijun. Predicting the possibility of blood transfusion after total knee arthroplasty based on machine learning algorithm [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(36): 5792-5797. |
| [8] | Hou Kunpeng, Zhao Quanlai, Wu Tianliang, Xiao Liang, Liu Chen, Xu Hongguang. Biomechanical stability of oblique lateral lumbar fusion and internal fixation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(33): 5362-5368. |
| [9] | Wang Yachao, Huang Jian. Relationship between prosthetic dislocation and lumbar pelvic sagittal parameters in patients undergoing total hip replacement after lumbar fusion [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(30): 4870-4876. |
| [10] | Zhang Mingyan, Liu Xiangyang, Chang Lei, Chen Jing, Shen Xiongjie, Liu Bin, Peng Shuai, Zhang Chao, Wu Huanyu, Zhu Feng, Mou Haipin . Relationship between the intraoperative endplate injury and cage retropulsion after lumbar interbody fusion [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2856-2862. |
| [11] | Zhong Yuanming, Fu Xiaopeng, Xu Wei, Zhao Qingrui, Huang Yong, Ye Weiquan. Nicardipine controlled hypotension applied to perioperative blood loss in orthopedics: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2930-2937. |
| [12] | Tian Lin, Shi Xiaoqing, Mao Jun, Zhang Nongshan, Zhang Li, Xing Runlin, Wang Peimin. Meta-analysis of vacuum-sealing drainage combined with antibiotic bone cement in the treatment of chronic osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2618-2624. |
| [13] | Cai Hongmei, Wang Wei, Wang Wenjuan, Zhou Xiaohong. Kinesiology taping combined with manual lymph drainage reduces postoperative lymphedema related to breast cancer [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(14): 2247-2251. |
| [14] | Qin Wenpin, Yang Yujie, Zhao Laihe, Shi Xiaowei, Lu Lei, Yang Hongxu, Huang Jinghui. Hemorrhage control of fluid gelatin SurgifloTM versus gelatin sponge in lumbar spine fusion surgery [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(4): 561-565. |
| [15] | Wang Jing, Xu Shuai, Liu Haiying. Hidden blood loss during posterior lumbar interbody fusion in lumbar spinal stenosis patients with and without rheumatoid arthritis [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(33): 5307-5314. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||