Chinese Journal of Tissue Engineering Research ›› 2023, Vol. 27 ›› Issue (25): 4006-4012.doi: 10.12307/2023.545
Previous Articles Next Articles
Terpinen-4-ol with antibacterial properties promotes osteogenic differentiation of MC3T3-E1 cells
Guo Pengda1, Liu Keke2, Duan Xin1, Liu Zhaohui1, Zhang Yuntao1
- 1Department of Stomatology, Binzhou Medical University Hospital, Binzhou 256600, Shandong Province, China; 2Department of Stomatology, Zhoukou Central Hospital, Zhoukou 466099, Henan Province, China
-
Received:2022-06-23Accepted:2022-09-06Online:2023-09-08Published:2023-01-17 -
Contact:Zhang Yuntao, Associate professor, Department of Stomatology, Binzhou Medical University Hospital, Binzhou 256600, Shandong Province, China -
About author:Guo Pengda, Master candidate, Department of Stomatology, Binzhou Medical University Hospital, Binzhou 256600, Shandong Province, China
CLC Number:
Cite this article
Guo Pengda, Liu Keke, Duan Xin, Liu Zhaohui, Zhang Yuntao. Terpinen-4-ol with antibacterial properties promotes osteogenic differentiation of MC3T3-E1 cells[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(25): 4006-4012.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

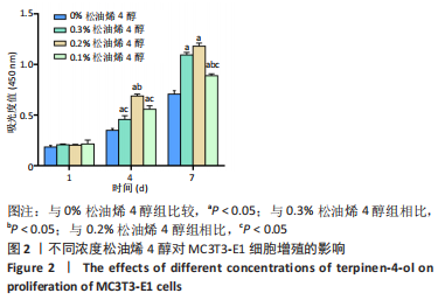
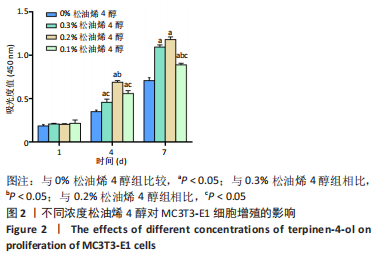
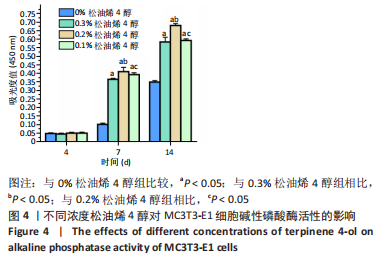
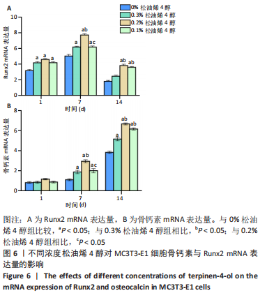
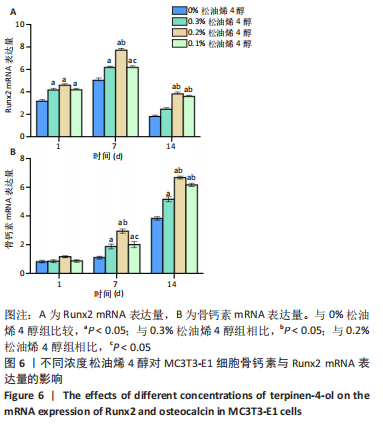
细胞钙化诱导1 d时,各组之间骨钙素 mRNA表达量比较差异无显著性意义(P > 0.05);各组间Runx2 mRNA表达量比较差异有显著性意义(P < 0.05),0.1%,0.2%,0.3%松油烯4醇组Runx2 mRNA表达量高于0%松油烯4醇组(P < 0.05)。7 d时,各组间骨钙素、Runx2 mRNA表达量比较差异均有显著性意义(P < 0.05),0.1%,0.2%,0.3%松油烯4醇组骨钙素、Runx2 mRNA表达量均高于0%松油烯4醇组(P < 0.05),0.2%松油烯4醇组骨钙素、Runx2 mRNA表达量高于0.1%,0.3%松油烯4醇组(P < 0.05)。14 d时,各组间骨钙素、Runx2 mRNA表达量差异有显著性意义(P < 0.05),0.1%,0.2%,0.3%松油烯4醇组骨钙素mRNA表达量高于0%松油烯4醇组(P < 0.05),0.2%,0.1%松油烯4醇组骨钙素mRNA表达量高于0.3%松油烯4醇组(P < 0.05);0.2%,0.1%松油烯4醇组Runx2 mRNA表达量高于0%,0.3%松油烯4醇组(P < 0.05)。"

| [1] PENG K, ZHOU Y, DAI Y, et al. The effect of denture restoration and dental implant restoration in the treatment of dentition defect: a systematic review and meta-analysis. Ann Palliat Med. 2021;10(3): 3267-3276. [2] ANDERSON N, LORDS A, LAUX R, et al. Retrospective Analysis of the Risk Factors of Peri-implantitis. J Contemp Dent Pract. 2020;21:1350-1353. [3] AHN DH, KIM HJ, JOO JY, et al. Prevalence and risk factors of peri-implant mucositis and peri-implantitis after at least 7 years of loading. J Periodontal Implant Sci. 2019;49:397-405. [4] 朱睿,刘蔚晴,张鹏,等.种植体周围炎小鼠模型的研究进展[J].四川大学学报(医学版),2020,51(6):767-770. [5] KARATAS O, BALCI YUCE H, TASKAN MM, et al. Histological evaluation of peri-implant mucosal and gingival tissues in peri-implantitis, peri-implant mucositis and periodontitis patients: a cross-sectional clinical study. Acta Odontol Scand. 2020;78:241-249. [6] BUSER D, INGIMARSSON S, DULA K, et al. Long—term stability of osseointegrated implants in augmented bone:a 5-year prospective study in partially edentulous patients. Int J Periodontics Restorative Dent. 2002;22(2):109-117. [7] ZHAO L, CHU PK, ZHANG Y, et al. Antibacterial coatings on titanium implants. J Biomed Mater Res B Appl Biomater. 2009;91(1):470-480. [8] KOMATSU K, SHIBA T, TAKEUCHI Y, et al. Discriminating Microbial Community Structure Between Peri-Implantitis and Periodontitis With Integrated Metagenomic, Metatranscriptomic, and Network Analysis.Front Cell Infect Microbiol. 2020;10:596490. [9] KENSARA A, HEFNI E, WILLIAMS MA, et al. Microbiological Profile and Human Immune Response Associated with Peri-Implantitis: A Systematic Review. J Prosthodont. 2021;30:210-234. [10] SALVI GE, FURST MM, LANG NP, et al. One-year bacterial colonization patterns of Staphylococcus aureus and other bacteria at implants and adjacent teeth. Clin Oral Implants Res. 2008;19(3):242-248. [11] SHIAU HJ. Limited Evidence Suggests That Adjunctive Antimicrobial Photodynamic Therapy May Not Provide Additional Clinical Benefit to Conventional Instrumentation Strategy Alone in Periodontitis and Peri-implantitis Patients. J Evid Based Dent Pract. 2019;19:101346. [12] 程刚,王留宏,杨惠,等.氯己定联合机械清创对种植体周围炎的治疗效果及对患者SF-36评分的影响[J].上海口腔医学,2020,29(4): 400-404. [13] BOROLOI AK. Essential oils of Zing ibercassumunar from north east India. JEOR. 1999;11(4):441-445. [14] YASIN M, YOUNIS A, JAVED T, et al. River Tea Tree Oil: Composition, Antimicrobial and Antioxidant Activities, and Potential Applications in Agriculture. Plants (Basel). 2021;10(10):2105. [15] PAZYAR N, YAGHOOBI R, BAGHERANI N, et al. A review of applications of tea tree oil in dermatology. Int J Dermatol. 2013;52(7):784-790. [16] RIPARI F, CERA A, FREDA M, et al. Tea Tree Oil versus Chlorhexidine Mouthwash in Treatment of Gingivitis: A Pilot Randomized, Double Blinded Clinical Trial. Eur J Dent. 2020;14(1):55-62. [17] NOUMI E, MERGHNI A, M ALRESHIDI M, et al. Chromobacterium violaceum and Pseudomonas aeruginosa PAO1: Models for Evaluating Anti-Quorum Sensing Activity of Melaleuca alternifolia Essential Oil and Its Main Component Terpinen-4-ol. Molecules. 2018;23(10):2672. [18] MAQUERA-HUACHO PM, TONON CC, CORREIA MF, et al. In vitro antibacterial and cytotoxic activities of carvacrol and terpinen-4-ol against biofilm formation on titanium implant surfaces. Biofouling. 2018;34(6):699-709. [19] 宋玉梦,周红艳,黄鑫,等.茶树精油对变异链球菌抑菌浓度及效力的探究[J].实用口腔医学杂志,2020,36(5):701-705. [20] BUCCI AR, MARCELINO L, MENDES RK, et al. The antimicrobial and antiadhesion activities of micellar solutions of surfactin, CTAB and CPCl with terpinen-4-ol: applications to control oral pathogens. World J Microbiol Biotechnol. 2018;34(6):86. [21] FERRINI AM, MANNONI V, AURELI P, et al. Melaleuca alternifolia essential oil possesses potent anti-staphylococcal activity extended to strains resistant to antibiotics. Int J Immunopathol Pharmacol. 2006; 19(3):539-544. [22] 周思佳,姜文学,尤佳.骨缺损修复材料:现状与需求和未来[J].中国组织工程研究,2018,22(14):2251-2258. [23] SCHWARZ F, DERKS J, MONJE A, et al. Peri-implantitis. J Periodontol. 2018;89 Suppl 1:S267-S290. [24] ALSAADI G, QUIRYNEN M, KOMÁREK A, et al. Impact of local and systemic factors on the incidence of late oral implant loss. Clin Oral Implants Res. 2008;19(7):670-676. [25] BERGLUNDH T, JEPSEN S, STADLINGER B, et al. Peri-implantitis and its prevention. Clin Oral Implants Res. 2019;30(2):150-155. [26] FU JH, WANG HL. Breaking the wave of peri-implantitis. Periodontol 2000. 2020;84(1):145-160. [27] ROCCUZZO M, LAYTON DM, ROCCUZZO A, et al. Clinical outcomes of peri-implantitis treatment and supportive care: A systematic review. Clin Oral Implants Res. 2018;29 Suppl 16:331-350. [28] WIEDEMANN TG. A Clinical Approach to Treatment of Retrograde Peri-Implantitis.Compend Contin Educ Dent. 2021;42(4):e5-e9. [29] BROOKES ZLS, BELFIELD LA, ASHWORTH A, et al. Effects of chlorhexidine mouthwash on the oral microbiome. J Dent. 2021;113:103768. [30] TETÈ G, CATTONI F, POLIZZI E. Anti-discoloration system: a new chlorhexidine mouthwash. J Biol Regul Homeost Agents. 2021;35(4 Suppl.1):113-118. [31] BORDINI EAF, TONON CC, FRANCISCONI RS, et al. Antimicrobial effects of terpinen-4-ol against oral pathogens and its capacity for the modulation of gene expression. Biofouling. 2018;34(7):815-825. [32] CORDEIRO L, FIGUEIREDO P, SOUZA H, et al. Terpinen-4-ol as an Antibacterial and Antibiofilm Agent against Staphylococcus aureus. Int J Mol Sci. 2020;21(12):4531. [33] LISTER JL, HORSWILL AR. Staphylococcus aureus biofilms: recent developments in biofilm dispersal. Front Cell Infect Microbiol. 2014; 4:178. [34] HENNEICKE H, GASPARINI SJ, BRENNAN-SPERANZA TC, et al. Glucocorticoids and bone: local effects and systemic implications. Trends Endocrinol Metab. 2014;25(4):197-211. [35] Komori T. Runx2, an inducer of osteoblast and chondrocyte differentiation. Histochem Cell Biol. 2018;149(4):313-323. [36] NARAYANAN A, SRINAATH N, ROHINI M, et al. Regulation of Runx2 by MicroRNAs in osteoblast differentiation. Life Sci. 2019;232:116676. [37] CHING HS, LUDDIN N, RAHMAN IA, et al. Expression of Odontogenic and Osteogenic Markers in DPSCs and SHED: A Review. Curr Stem Cell Res Ther. 2017;12(1):71-79. [38] WANG Z, USTRIYANA P, CHEN K, et al. Toward the Understanding of Small Protein-Mediated Collagen Intrafibrillar Mineralization. ACS Biomater Sci Eng. 2020;6(7):4247-4255. [39] LIU Y, LIU Q, LI Z, et al. Long non-coding RNA and mRNA expression profiles in peri-implantitis vs periodontitis. J Periodontal Res. 2020;55: 342-353. [40] CORDEIRO L, FIGUEIREDO P, SOUZA H, et al. Terpinen-4-ol as an Antibacterial and Antibiofilm Agent against Staphylococcus aureus. Int J Mol Sci. 2020;21(12):4531. |
| [1] | Wang Yuehui, Shang Jin, Yang Chen, Fu Dongge, Cao Can, Zhang Xiaodong, Wang Jingfu. Evaluation of FTA-LAMP direct extraction method for extracting DNA from Streptococcus mutans [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1040-1049. |
| [2] | Zheng Qian, Liu Pingping, Gu Yujie, Xie Lei. Effect of ursolic acid on osteogenic differentiation of human periodontal ligament stem cells#br# [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(1): 80-86. |
| [3] | Li Zhiyao, Hu Zheng, Li Xuan, Lu Peijun. Effects of enamel adhesives with different components on Porphyromonas gingivalis and Streptococcus mutans [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 329-335. |
| [4] | Qiu Xiaoming, Li Jidong, Kang Guan, Qiao Yongjie, Li Wenbo, Feng Qiangsheng, Zhen Ping, Lan Xu. Size of the borehole affects rabbit tibial osteomyelitis models [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(28): 4429-4434. |
| [5] | Chen Xiaosi, Tan Xiaoyan, Liu Tianfeng, Han Dengpeng, Wei Bo, Hu Zibing, Wu Shaoke. Effects of asiatic acid on biomechanical properties, trabecular area and Runx2 protein in osteoporotic rats [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(2): 246-251. |
| [6] | Zhang Yaotian, Cui Jun, Liu Jingyi. miR-889-3p inhibits osteogenic differentiation of adipose-derived mesenchymal stem cells by targeting Runx2 [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(19): 3023-3028. |
| [7] | Liang Weiye, Duan Qinghong. Correlation between femur bone morphogenetic protein 2 expression and bone fluoride content in fluorosis rabbits [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(17): 2675-2680. |
| [8] | Huang Yanni, Yang Hua, Yang Dongmei, Hu Xulin, Gao Hong, Huang Yina. Rat bone defect repaired with polytrimethylene carbonate/beta-tricalcium phosphate microsphere scaffold [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(12): 1856-1862. |
| [9] | Hu Jinlong, Quan Huahong, Wang Jingcheng, Zhang Pei, Zhang Jiale, Chen Pengtao, Liang Yuan. Effect of copper sulfide nanoparticles loaded thermosensitive hydrogel Pluronic F127 on infected wound healing in rats [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(12): 1927-1931. |
| [10] | Wang Lei, Bai Xuesong, Du Yu, He Aimin, Zheng Jun, Zhang Zhipeng, Lyu Huicheng. Significance of miR-27b/peroxisome proliferators-activated receptor gamma 2 axis for proliferation and osteoblast differentiation of mouse embryonic osteogenic precursor cells [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(11): 1780-1786. |
| [11] | Feng Jianbo, Li Chencheng, Liu Jinyue, Wang Xiaomin, Peng Jiachen. Implantation of Kirschner wire with Staphylococcus aureus biofilm establishes a traumatic osteomyelitis model in rats [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 700-705. |
| [12] | Li Kongmei, Luo Yicai, Li Hao. Effect of inhibiting miR-203-3p expression on bone formation around dental implants in diabetic mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(32): 5102-5106. |
| [13] | Huang Wei, Dong Panfeng, Huang Yourong, Xia Tian. Epimedium in regulating bone marrow mesenchymal stem cell differentiation and preventing osteoporosis related signaling pathways [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(30): 4889-4895. |
| [14] | Hu Pengyu, Yu Zhiping, Jia Guanghou, Cong Zhichao, Cong Haibo. Adjuvant treatment of nonunion of tibial fractures with platelet-rich plasma evaluated by bone turnover markers [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(27): 4367-4373. |
| [15] | Li Hu, Guan Xiaoyan, Li Min, Dong Jingnan, Xiao Qianwen, Bai Guohui, Wang Mingwei, Liu Jianguo. Hydrogel loaded anti-caries DNA vaccine pVAX1-SpaP/P produces immune effects in four ways [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(27): 4340-4345. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||