Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (27): 4367-4373.doi: 10.12307/2022.869
Previous Articles Next Articles
Adjuvant treatment of nonunion of tibial fractures with platelet-rich plasma evaluated by bone turnover markers
Hu Pengyu, Yu Zhiping, Jia Guanghou, Cong Zhichao, Cong Haibo
- Weihai Central Hospital Affiliated to Qingdao University, Weihai 264400, Shandong Province, China
-
Received:2021-03-19Accepted:2021-05-17Online:2022-09-28Published:2022-03-11 -
Contact:Cong Haibo, Professor, Chief physician, Doctoral supervisor, Weihai Central Hospital Affiliated to Qingdao University, Weihai 264400, Shandong Province, China -
About author:Hu Pengyu, Master, Physician, Weihai Central Hospital Affiliated to Qingdao University, Weihai 264400, Shandong Province, China -
Supported by:Special Foundation for Taishan Scholars Project, No. ts201511110 (to CHB)
CLC Number:
Cite this article
Hu Pengyu, Yu Zhiping, Jia Guanghou, Cong Zhichao, Cong Haibo. Adjuvant treatment of nonunion of tibial fractures with platelet-rich plasma evaluated by bone turnover markers[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(27): 4367-4373.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
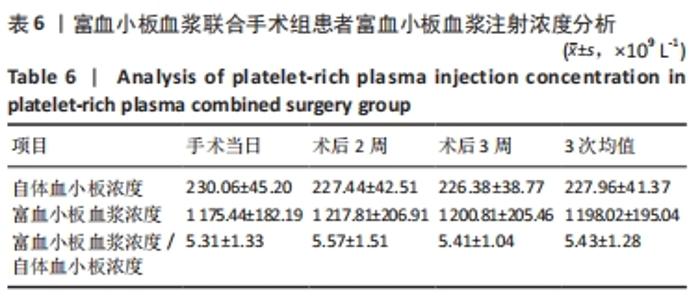
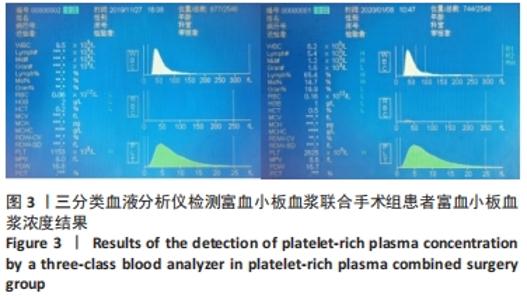
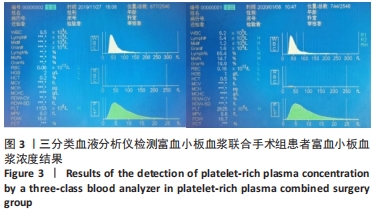
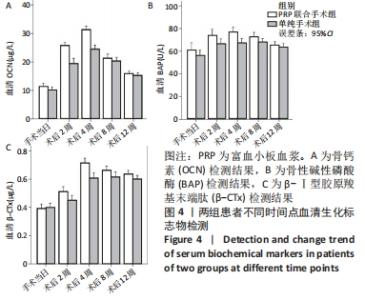
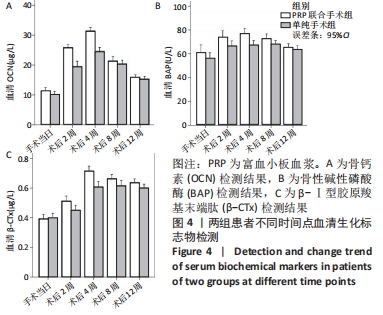
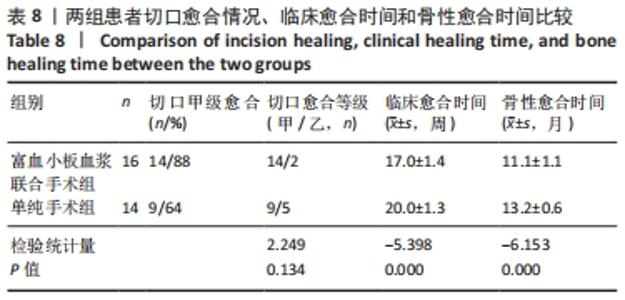
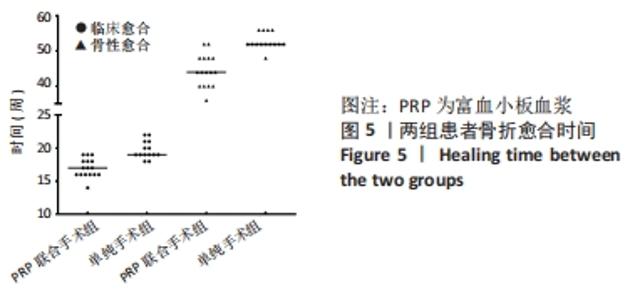
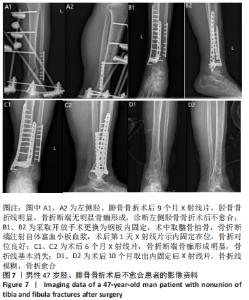
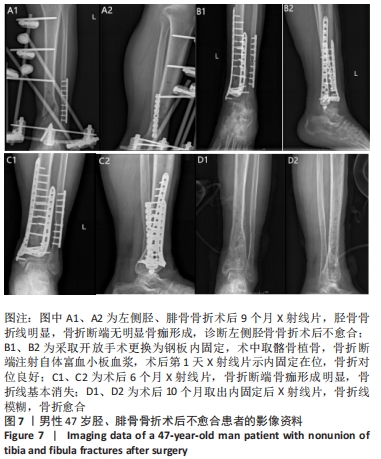
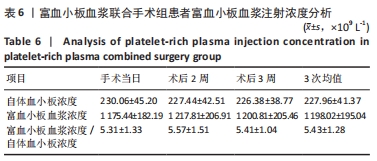
2.4 两组患者随访时间 30例患者术后均获得随访,随访时间9-14个月,平均(12.10±1.40)个月,两组患者骨折均愈合,无不良反应发生。 2.5 富血小板血浆联合手术组患者富血小板血浆注射浓度 富血小板血浆联合手术组患者中,3次注射的富血小板血浆浓度分别为(1 175.44±182.19)×109,(1 217.81±206.91)×109,(1 200.81±205.46)×109 L-1,分别为自体血小板浓度的(5.31±1.33),(5.57±1.51),(5.41±1.04)倍,平均(5.43±1.28)倍,符合当前所认同的3-7倍值,结果见表6。验证富血小板血浆浓度结果,见图3。"
| [1] KHATKAR H, SEE A. Stem Cell Therapy in the Management of Fracture Non-Union - Evaluating Cellular Mechanisms and Clinical Progress. Cureus. 2021;13(3):e13869. [2] 刘璠,祁俊.骨折不愈合与延迟愈合的成因与治疗[J].中华创伤骨科杂志, 2005,7(5):405-408. [3] 刘金伟,陈允震,万春友.应力作用下骨不连断端组织中成骨因子的变化[J].中国组织工程研究,2021,25(23):3619-3624. [4] KASTIRR I, REICHARDT M, ANDRESEN R, et al. Therapy of aseptic nonunions with parathyroid hormone. Eur J Orthop Surg Traumatol. 2019;29(1):169-173. [5] ANDERSEN C, WRAGG NM, SHARIATZADEH M, et al. The Use of Platelet-Rich Plasma (PRP) for the Management of Non-union Fractures. Curr Osteoporos Rep. 2021;19(1):1-14. [6] SCHMAL H, BRIX M, BUE M, et al. Nonunion - consensus from the 4th annual meeting of the Danish Orthopaedic Trauma Society. EFORT Open Rev. 2020;5(1): 46-57. [7] MARCK RE, GARDIEN K, VLIG M, et al. Growth Factor Quantification of Platelet-Rich Plasma in Burn Patients Compared to Matched Healthy Volunteers. Int J Mol Sci. 2019;20(2):288. [8] MIDDLETON KK, BARRO V, MULLER B, et al. Evaluation of the effects of platelet-rich plasma (PRP) therapy involved in the healing of sports-related soft tissue injuries. Iowa Orthop J. 2012;32:150-163. [9] ALSOUSOU J, THOMPSON M, HULLEY P, et al. The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: a review of the literature. J Bone Joint Surg Br. 2009;91(8):987-996. [10] ALVES R, GRIMALT R. A Review of Platelet-Rich Plasma: History, Biology, Mechanism of Action, and Classification. Skin Appendage Disord. 2018;4(1):18-24. [11] HALPERN BC, CHAUDHURY S, RODEO SA. The role of platelet-rich plasma in inducing musculoskeletal tissue healing. HSS J. 2012;8(2):137-145. [12] RODRIGUEZ-MERCHAN EC, FORRIOL F. Nonunion: general principles and experimental data. Clin Orthop Relat Res. 2004;(419):4-12. [13] EINHORN TA, GERSTENFELD LC. Fracture healing: mechanisms and interventions. Nat Rev Rheumatol. 2015;11(1):45-54. [14] FISHER JS, KAZAM J J, FUFA D, et al. Radiologic evaluation of fracture healing. Skeletal Radiol. 2019;48(3):349-361. [15] 姜苗苗,谭勇海,金鑫,等.富血小板血浆联合体外冲击波治疗骨不连的临床研究[J].中医正骨,2020,32(2):30-35. [16] MEDDA S, SNOAP T, CARROLL EA. Treatment of Young Femoral Neck Fractures. J Orthop Trauma. 2019;33 Suppl 1:S1-S6. [17] MILGRAM JW. Nonunion and pseudarthrosis of fracture healing. A histopathologic study of 95 human specimens. Clin Orthop Relat Res. 1991;(268):203-213. [18] HAUGSTVEDT JR, WONG CW. Arthroscopic treatment for nonunion of the scaphoid. Handchir Mikrochir Plast Chir. 2020;52(5):413-418. [19] LAMMENS J, VAN LAER M, MOTMANS R. Ilizarov treatment for femoral mal-union or non-union associated with fatigue fracture of an intramedullary nail. Injury. 2008;39(2):256-259. [20] KURKLU M, YURTTAS Y, KOSE O, et al. Adjunctive hyperbaric oxygen therapy in the treatment of atrophic tibial nonunion with Ilizarov external fixator: a radiographic and scintigraphic study in rabbits. Acta Orthop Traumatol Turc. 2012;46(2):126-131. [21] HANNEMANN PF, MOMMERS EH, SCHOTS JP, et al. The effects of low-intensity pulsed ultrasound and pulsed electromagnetic fields bone growth stimulation in acute fractures: a systematic review and meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg. 2014;134(8):1093-1106. [22] PADILLA F, PUTS R, VICO L, et al. Stimulation of bone repair with ultrasound: a review of the possible mechanic effects. Ultrasonics. 2014;54(5):1125-1145. [23] BOTTEGONI C, DEI GL, SALVEMINI S, et al. Homologous platelet-rich plasma for the treatment of knee osteoarthritis in selected elderly patients: an open-label, uncontrolled, pilot study. Ther Adv Musculoskelet Dis. 2016;8(2):35-41. [24] DALLARI D, STAGNI C, RANI N, et al. Ultrasound-Guided Injection of Platelet-Rich Plasma and Hyaluronic Acid, Separately and in Combination, for Hip Osteoarthritis: A Randomized Controlled Study. Am J Sports Med. 2016;44(3): 664-671. [25] KANCHANATAWAN W, ARIRACHAKARAN A, CHAIJENKIJ K, et al. Short-term outcomes of platelet-rich plasma injection for treatment of osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1665-1677. [26] KASTIRR I, REICHARDT M, ANDRESEN R, et al. Therapy of aseptic nonunions with parathyroid hormone. Eur J Orthop Surg Traumatol. 2019;29(1):169-173. [27] FAN T, HUANG G, WU W, et al. Combined treatment with extracorporeal shock-wave therapy and bone marrow mesenchymal stem cell transplantation improves bone repair in a rabbit model of bone nonunion. Mol Med Rep. 2018;18(4):4156. [28] ZHANG L, JIAO G, REN S, et al. Exosomes from bone marrow mesenchymal stem cells enhance fracture healing through the promotion of osteogenesis and angiogenesis in a rat model of nonunion. Stem Cell Res Ther. 2020;11(1):38. [29] LOPEZ S, VILAR JM, SOPENA JJ, et al. Assessment of the Efficacy of Platelet-Rich Plasma in the Treatment of Traumatic Canine Fractures. Int J Mol Sci. 2019; 20(5):1075. [30] XU PC, XUAN M, CHENG B. Effects and mechanism of platelet-rich plasma on military drill injury: a review. Mil Med Res. 2020;7(1):56. [31] CHU W. Treatment of nonunion with autologous bone transplantation combined with platelet-rich plasma and extracorporeal shock wave. Zhongguo Gu Shang. 2019;32(5):434-439. [32] ANDERSEN C, WRAGG NM, SHARIATZADEH M, et al. The Use of Platelet-Rich Plasma (PRP) for the Management of Non-union Fractures. Curr Osteoporos Rep. 2021;19(1):1-14. [33] LYNCH MD, BASHIR S. Applications of platelet-rich plasma in dermatology: A critical appraisal of the literature. J Dermatolog Treat. 2016;27(3):285-289. [34] YU W, JINGXIN Z, LINGWEI K, et al. Involvement of bone-specific alkaline phosphatase and procollagen I carboxy-terminal propeptide as predictors of early fracture risk in Chinese Children with juvenile osteoporosis: An interventional clinical trial. Bangl J Pharmacol. 2018;13(2):164. [35] URAKAWA H, ANDO Y, HASE T, et al. Clinical value of serum bone resorption markers for predicting clinical outcomes after use of bone modifying agents in metastatic bone tumors: A prospective cohort study. Int J Cancer. 2020;146(12): 3504-3515. [36] VALLET S, HOYLE NR, KYLE RA, et al. A role for bone turnover markers beta-CrossLaps (CTX) and amino-terminal propeptide of type I collagen (PINP) as potential indicators for disease progression from MGUS to multiple myeloma. Leuk Lymphoma. 2018;59(10):2431-2438. |
| [1] | Yuan Jiabin, Zhu Zongdong, Tang Xiaoming, Wei Dan, Tan Bo, Xiao Chengwei, Zhao Ganlinwei, Liao Feng. Classification and reduction strategies for irreducible intertrochanteric femoral fracture based on anatomy [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1341-1345. |
| [2] | Pan Baoshun, Fang Zhen, Gao Mingjie, Fang Guiming, Chen Jinshui. Design for posterior atlantoaxial internal fixation system with fusion cage based on imaging data [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1372-1376. |
| [3] | Li Kun, Gao Erke, Xiong Feng, Wang Xing, Wu Danqi, Li Zhijun, Zhang Shaojie, Liu Yanan, Duo Lan, Li Ziyu. Feasibility of axial transpedicle screw internal fixation in children aged 1 to 6 years [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1383-1387. |
| [4] | Zhang Xinlong, Ci Wentao, Luo Kaiwen, Yan shi. Internal fixation failure after proximal femoral nail antirotation: causes and reoperation strategies [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 973-979. |
| [5] | Yang Jun, Yang Qun, Zhang Rui, Jiang Chang. A novel slidable pedicle screw-rod system for lumbar tuberculosis: promoting bone graft fusion by producing stress stimulation to fused segment [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 914-918. |
| [6] | Liang Haoran, Zhou Xin, Yang Yanfei, Niu Wenjie, Song Wenjie, Ren Zhiyuan, Wang Xueding, Liu Yang, Duan Wangping. Pathogenesis of femoral head necrosis after internal fixation of femoral neck fractures in young adults [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 456-460. |
| [7] | Liu Zemin, Lü Xin. Application of intramedullary nailing in the treatment of long tubular bone fractures of the extremities: reaming and non-reaming [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 461-467. |
| [8] | Yang Ruijia, Jiang Lingkai, Dong Zhengquan, Wang Yunfei, Ma Zhou, Cong Linlin, Guo Yanjing, Gao Yangyang, Li Pengcui. Open reduction and internal fixation versus circular external fixation for tibial plateau fractures: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 480-486. |
| [9] | Cai Feng, Yu Bo, Zeng Duo, Chen Qincan, Liao Qi. Cortical bone trajectory in elderly patients with osteoporosis of lumbar disease [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 403-407. |
| [10] | Yu Xue, Li Xiaofeng, Shu Kegang, Wu Liwei, Wang Yonglin, Lyu Dingkang, Zhou Anyuan, Liang Chaoxin, Yang Yuan. Hyperbaric oxygen improves fracture healing by promoting osteoblast proliferation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(26): 4136-4140. |
| [11] | Liu Chao, Zhang Lijun, Du Xinjie, Xu Qian, Lü Hongjuan, Fan Dongmei, Tian Huanling, Huang Jian, Huang Yuxiang. Mechanism of human umbilical cord mesenchymal stem cells to promote platelet plasma coagulation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(25): 4010-4015. |
| [12] | Tian Chong, Gao Bo, Yu Hongwei, Wang Pei. Theoretical research and technical application of bone repair materials in the treatment of calcaneal fractures [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(22): 3586-3591. |
| [13] | Yang Jiaojiao, Hu Ming, Li Yan, Xia Delin. Effect of hydroxyapatite three-dimensional scaffolds with different apertures on the biological properties of MC3T3-E1 cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(21): 3338-3344. |
| [14] | Zhan Yi, Kang Xin, Wang Yuhang, Zhang Haiping, He Simin, Sun Honghui, Hao Dingjun, Wang Biao. Biomechanical properties of a novel bone cement screw and traditional methods for Kummell’s disease [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(21): 3381-3388. |
| [15] | Yan Qifang, Xie Cuiliu, Yan Guowei. Effect of concentrated growth factor and bioceramic material iRoot BP on survival, proliferation and mineralization of human dental pulp cells in vitro [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(21): 3363-3368. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||