[1] XU YQ, XING SM, FANG LQ, et al. Application of internal fixation with screws for thoracolumbar fractures through the muscular space approach of Wiltse. J Surg Res. 2019;8(20):29-31.
[2] LIU T, CUI J. Clinical Effect of Posterior Internal Fixation and Fusion in the Treatment of Thoracolumbar Fractures. Clin Nurs Stud. 2021; 5(2):4-5.
[3] YANGUO HE, HOSPITAL BP. Comparison of Therapeutic Effects between Across-traumatic and Trans-traumatic vertebral Internal Fixation for Thoracolumbar Spine Fracture. J Tradit Chin Med. 2019;9(2):91-93.
[4] HU D, FEI J, CHEN G, et al. Mini-open anterior approach focal cleaning combined with posterior internal fixation for thoracolumbar tuberculosis: Follow-up of 149 cases. Asian J Surg. 2019;1(4):54-57.
[5] 何人可,曹杨.胸腰椎骨折后路手术治疗研究进展[J].国际骨科学杂志,2020,41(2):100-103.
[6] CHENG Y, LIU Y. Percutaneous curved vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fractures. J Int Med Res. 2019;47(6):2424-2433.
[7] 赵星毅,王黎明,沙卫平,等.微创经皮与开放椎弓根螺钉内固定技术治疗胸腰段脊柱骨折的临床疗效对比[J].徐州医学院学报, 2020,40(2):122-125.
[8] 夏太宝,赵广超,薛双桃,等.经皮与Wiltse入路椎弓根螺钉治疗单节段胸腰椎骨折的疗效比较[J].临床骨科杂志,2018,21(4):415-418.
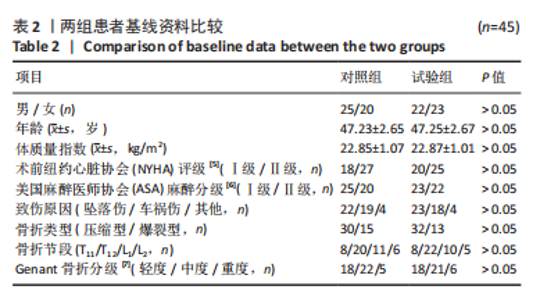
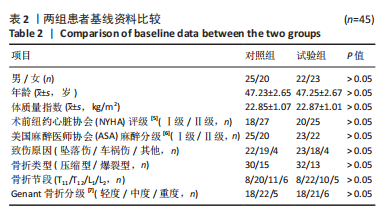
[9] DEMERS C, MCKELVIE RS, YUSUF S. Interobserver reliability and validity of the New York Heart Association Functional Classification (NYHA-FC) in heart failure patients. Eur J Heart Fail. 2000;2(1):73-79.
[10] MICHEL JP, KLOPFENSTEIN C, HOFFMEYER P, et al.Hip fracture surgery: Is the pre-operative American Society of Anesthesiologists (ASA) score a predictor of functional outcome? Aging Clin Exp Res. 2002;14(5): 389-394.
[11] GENANT HK, JERGAS M. Assessment of prevalent and incident vertebral fractures in osteoporosis research. Osteoporos Int. 2003;14(3 Supplement):43-55.
[12] HU D, FEI J, CHEN G, et al. Mini-open anterior approach focal cleaning combined with posterior internal fixation for thoracolumbar tuberculosis: Follow-up of 149 cases - ScienceDirect. Asian J Surg. 2020; 43(1):78-86.
[13] KANE RL, BERSHADSKY B, ROCKWOOD T, et al.Visual Analog Scale pain reporting was standardized. J Clin Epidemiol. 2005;58(6):618-623.
[14] FAIRBANK JCT, PYNSENT PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000;25(22):2940-2953.
[15] CAO YL, HAN YJ, CHEN P, et al. Surgical treatment of thoracolumbar fracture with incomplete lower limb paralysis in a patient with COVID-19. Chin J Traumatol. 2020;23(4):67-69.
[16] LAGHMOUCHE N, PROST S, FARAH K, et al. Minimally invasive treatment of thoracolumbar flexion-distraction fractur. Orthop Traumatol Surg Res. 2019;105(2):347-350.
[17] 于召龙,梁鹤,王云浩,等.骨质疏松性椎体骨折并胸腰椎后凸畸形的诊治进展[J].医学综述,2020,26(11):2218-2222.
[18] 郭钟义,马俊,黄亮亮,等.经伤椎置钉治疗胸腰椎骨折的研究进展[J].脊柱外科杂志,2021,19(4):280-285.
[19] 路多,代文杰,李海涛,等.经伤椎置钉短节段内固定术治疗单节段胸腰椎骨折的临床疗效及术后并发症发生情况[J].脊柱外科杂志,2020,18(5):321-324.
[20] 冯学武,郝虎萍,刘小军.短节段经皮微创与传统椎弓根螺钉内固定治疗伴后方韧带复合体损伤的胸腰椎骨折的比较[J].贵州医药, 2020,44(10):1610-1612.
[21] 张世磊,闫铭,丁子毅,等.微创经皮单平面椎弓根螺钉间接减压治疗胸腰椎骨折的椎管侵占率和椎体高度观察[J].骨科,2020,11(6): 513-517.
[22] 黄钟炼,张楠,张元涛.微创经皮与经肌间隙入路椎弓根螺钉内固定治疗胸腰椎骨折的临床效果比较[J].中国医药导报,2020,17(9): 73-77.
[23] 刘富强,郝佩佩,何荣,等.后路短节段非融合内固定治疗胸腰椎骨折的疗效观察[J].广东医学院学报,2019,37(4):434-436.
[24] SALLE H, MEYNARD A, AUDITEAU E, et al. Treating traumatic thoracolumbar spine fractures using minimally invasive percutaneous stabilization plus balloon kyphoplasty: a 102-patient series. J Neurointerv Surg. 2021;13(9):848-853.
[25] 刘福全,张世民.经后路伤椎单节段椎弓根螺钉内固定术治疗胸腰椎骨折的临床效果观察[J].中国医刊,2020,55(7):753-756.
[26] YUAN H, CHANG QY, CHEN J, et al. A retrospective analysis of the effects of different analgesics on the pain of patients with traumatic thoracolumbar fractures in the peri-treatment period. J Orthop Surg Res. 2021;16(1):62-67.
[27] TAN T, HUANG MS, MATHEW J, et al. Anterior versus posterior approach in the management of AO Type B1 & B2 traumatic thoracolumbar fractures: A level 1 trauma centre study. J Clin Neurosci. 2019;72(23):12-13.
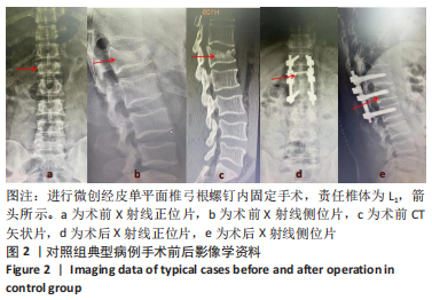
[28] 赵伟,乔虎云,李春江.单轴椎弓根螺钉内固定技术在胸腰段骨折治疗中的应用[J].中国药物与临床,2020,20(23):3971-3972.
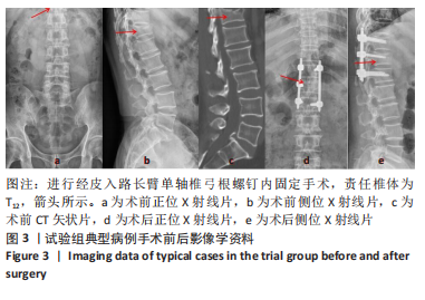
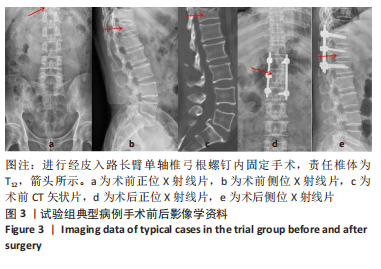
[29] 郝斌昌,李亮宇,孙科研.长臂单轴椎弓根螺钉经Wistle入路与经皮入路手术对创伤性胸腰椎压缩骨折患者疗效的影响[J].颈腰痛杂志,2021,42(3):404-406.
[30] Yi L, Qiao ZJ. Clinical effect of pedicle screw internal fixation+Fuyuan Huoxue decoction on thoracolumbar fractures. Clin Res Pract. 2019; 9(1):67-69.
[31] CHENG Z, YOU HE, WANG W, et al. Biomechanical Characteristics of Internal Fixation Methods for Treating Thoracolumbar Burst Fractures. J Med Biomech. 2019;11(3):12-17.
[32] SUN JW, LIU B, ORTHOPEDICS DO. Analysis of the effect of minimally invasive internal fixation on thoracolumbar spinal fracture. J Community Med. 2019;7912):612-613.
[33] LI M, HE EX, Yin ZX, et al. Percutaneous indirect decompression and internal fixation for treatment of thoracolumbar burst fracture with nerve injury. J Spine J. 2019;5(7):32-35. |