Chinese Journal of Tissue Engineering Research ›› 2023, Vol. 27 ›› Issue (18): 2903-2909.doi: 10.12307/2023.308
Previous Articles Next Articles
Analysis and reconstruction of sagittal lumbo-pelvic parameters in the elderly with lumbar spinal stenosis
Xiao Shipeng1, Guo Chen2, Li Shichun1, Li Qinliang1, Xu Yong1, Xu Shuai2
- 1Department of Orthopedics, Beijing Shijingshan Hospital, Beijing 100040, China; 2Department of Spinal Surgery, Peking University People’s Hospital, Beijing 100044, China
-
Received:2022-02-23Accepted:2022-05-17Online:2023-06-28Published:2022-09-19 -
Contact:Xu Shuai, MD, Attending physician, Department of Spinal Surgery, Peking University People’s Hospital, Beijing 100044, China -
About author:Xiao Shipeng, Master, Associate chief physician, Department of Orthopedics, Beijing Shijingshan Hospital, Beijing 100040, China -
Supported by:Research and Development Fund of Peking University People’s Hospital, No. RDY2021-12 (to XS)
CLC Number:
Cite this article
Xiao Shipeng, Guo Chen, Li Shichun, Li Qinliang, Xu Yong, Xu Shuai. Analysis and reconstruction of sagittal lumbo-pelvic parameters in the elderly with lumbar spinal stenosis[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(18): 2903-2909.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
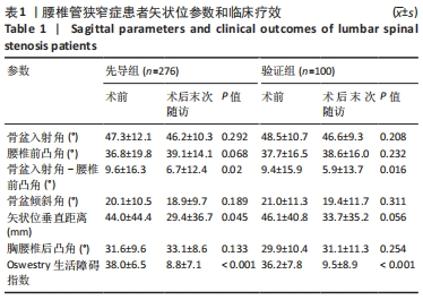
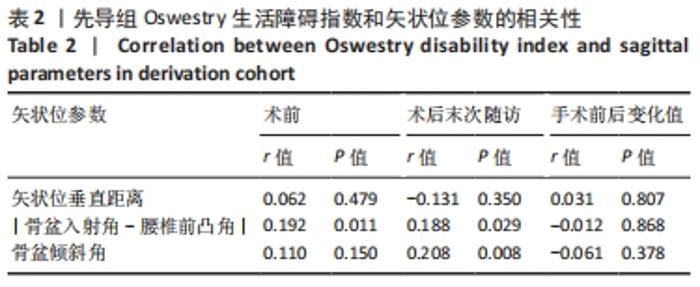
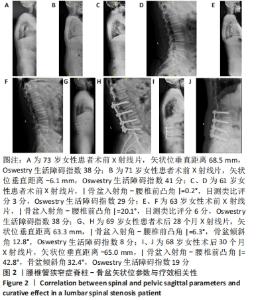
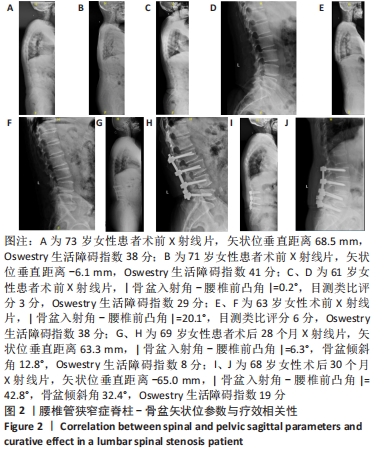
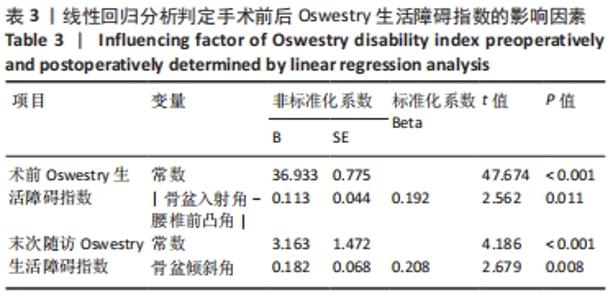
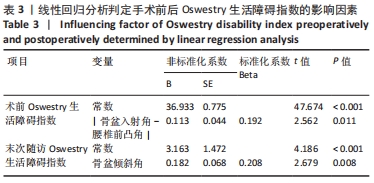
2.1 先导组与验证组患者一般资料 先导组276例患者中,男105例,女171例;平均年龄(68.8±7.7)岁;体质量指数(26.1±3.6) kg/m2;随访时间为(24.6±11.1)个月;单节段、双节段和3节段病例分别占20.8%,35.8%和43.4%。验证组100例患者中,男39例,女61例;平均年龄为(68.2±8.3)岁;体质量指数为(25.7±4.7) kg/m2;随访时间为(24.1±12.8)个月;单节段、双节段和3节段病例分别占15%,40%和45%。验证组与先导组在性别、年龄等人口统计学方面比较差异无显著性意义(P > 0.05)。 2.2 先导组患者矢状位参数与ODI的相关性 先导组与验证组手术前后矢状位参数与ODI变化,见表1。对比基线,先导组腰椎前凸角在术后末次随访时增加和减小者分别有130例和97例,|骨盆入射角-腰椎前凸角|和矢状位垂直距离均减小(P < 0.05),ODI平均减少29.9±9.9(P < 0.001)。先导组ODI轻度改善、中度改善和明显改善的人群分别为96.5%,68.2%和19.7%,其中仅2例术后末次随访ODI增加。先导组术前ODI与|骨盆入射角-腰椎前凸角|存在正相关(P=0.011),术后末次随访ODI与|骨盆入射角-腰椎前凸角|和骨盆倾斜角相关,与矢状位垂直距离无关,见表2、图2。此外,此次研究分析认为|骨盆入射角-腰椎前凸角|(r=0.027、P=0715)、骨盆倾斜角(r=0.065、P=0.031)、矢状位垂直距离(r=0.076、P=0.457)与年龄(55岁以上)无明确相关性。"
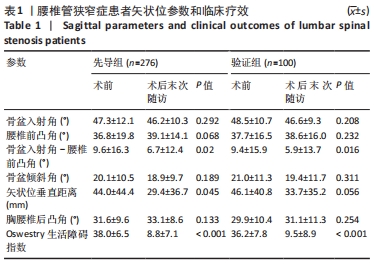
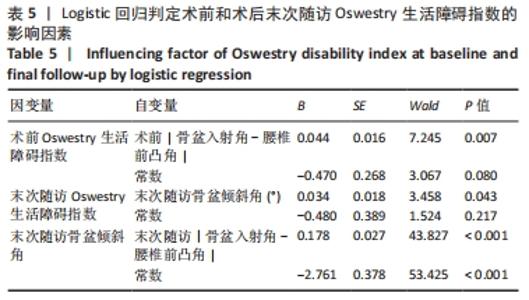
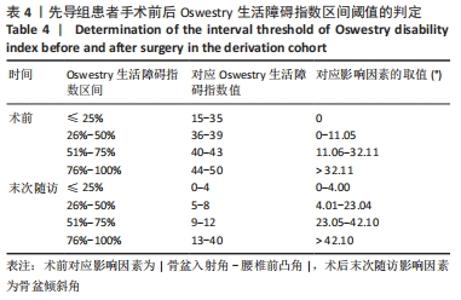
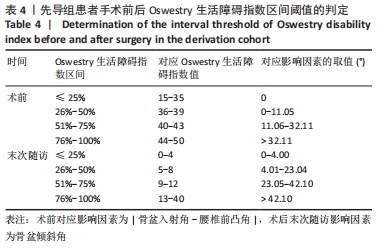
2.4 先导组患者脊柱-骨盆矢状位参数的合理匹配范围 术前ODI的独立正性影响因素为|骨盆入射角-腰椎前凸角|,确定代数关系式为:ODI=0.19×|骨盆入射角-腰椎前凸角|+36.9。根据ODI和|骨盆入射角-腰椎前凸角|的函数图像,结合临床意义,术前患者生活质量“轻度”受限所对应的|骨盆入射角-腰椎前凸角|为0°,生活质量“较轻度”受限对应的|骨盆入射角-腰椎前凸角|为0°-11.1°。而当|骨盆入射角-腰椎前凸角|超过32.1°时,患者生活质量将明显受限,见表4。 以术前|骨盆入射角-腰椎前凸角|=11.1°时所对应的术前ODI作为临界值(ODI=39),将术前ODI转换为二分类变量,进行Logistic回归分析,具体采用“输入”的方法,提示术前|骨盆入射角-腰椎前凸角|为术前ODI的影响因素(χ2=4.86,P=0.027,OR=1.97)。ROC曲线下面积(area under curve,AUC)为0.597,Youden指数=0.188,此时对应的术前|骨盆入射角-腰椎前凸角|临界值为10.4°,因此平均术前|骨盆入射角-腰椎前凸角|阈值为10.7°。即当术前|骨盆入射角-腰椎前凸角|≤10.7°时,患者生活质量“较轻度”受限,见表4,5。 "
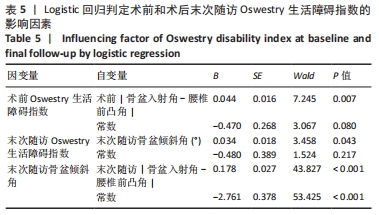
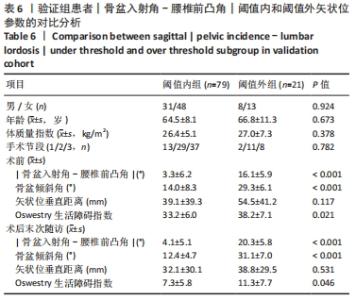
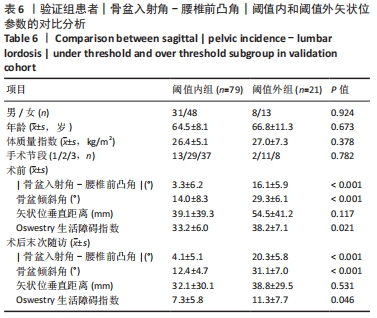
末次ODI正性影响因素为骨盆倾斜角,存在代数关系式为ODI=0.21×骨盆倾斜角+3.16。术后患者生活质量“优”和“良”者所对应的骨盆倾斜角分别为0°-4°和4°-23.0°。以术后骨盆倾斜角=23.0°时所对应的ODI作为临界值(ODI=8),进行Logistic回归分析,提示术后骨盆倾斜角为ODI的影响因素(χ2=7.20,P=0.007,OR=2.59)。ROC-AUC=0.602,Youden指数=0.245,此时对应的术后骨盆倾斜角临界值为23.2°,因此平均术后骨盆倾斜角阈值为23.1°,见表4,5。 通过线性回归分析获得拟合方程:骨盆倾斜角=0.60×|骨盆入射角-腰椎前凸角|+12.22,当骨盆倾斜角< 23.1°时,|骨盆入射角-腰椎前凸角|< 18.1°,可获得相对满意的术后疗效;当骨盆倾斜角> 42.1°,推导出|骨盆入射角-腰椎前凸角|> 49.8°,此时术后疗效欠佳。以术后骨盆倾斜角=23.1°作为临界值,将术后骨盆倾斜角转换为二分类变量,进行Logistic回归分析,提示术后|骨盆入射角-腰椎前凸角|为术后骨盆倾斜角的影响因素(χ2=62.71,P < 0.001,OR=16.19)。ROC-AUC=0.836,Youden指数=0.578,此时对应的术后|骨盆入射角-腰椎前凸角|临界值为13.9°,因此平均术后|骨盆入射角-腰椎前凸角|阈值为16.0°,见表4,5。 2.5 验证组矢状位参数与临床疗效的关系 研究主要依据术后|骨盆入射角-腰椎前凸角|的阈值(16°),将验证队列病例分为|骨盆入射角-腰椎前凸角|阈值内和超过|骨盆入射角-腰椎前凸角|阈值两亚组。 两亚组在性别(P=0.924)、年龄(P=0.673)方面无统计学差异。术前患者|骨盆入射角-腰椎前凸角|平均小于10.7°,且阈值内组|骨盆入射角-腰椎前凸角|和骨盆倾斜角小于阈值外组(P < 0.001),而矢状位垂直距离无统计学差异,两组术前ODI存在统计学差异。术后末次随访,两组|骨盆入射角-腰椎前凸角|和骨盆倾斜角存在统计学差异(P均< 0.001),且阈值内组骨盆倾斜角平均< 23°,阈值内组ODI优于阈值外组(P=0.046),见表6。 "
| [1] LAI M, CHEUNG P, CHEUNG J. A systematic review of developmental lumbar spinal stenosis. Eur Spine J. 2020;29(9):2173-2187. [2] HATAKKA J, PERNAA K, RANTAKOKKO J, et al. Effect of lumbar laminectomy on spinal sagittal alignment: a systematic review. Eur Spine J. 2021;30(9):2413-2426. [3] SIMMONS ED. Surgical treatment of patients with lumbar spinal stenosis with associated scoliosis. Clin Orthop Relat Res. 2001;(384): 45-53. [4] AEBI M. The adult scoliosis. Eur Spine J. 2005;14(10):925-948. [5] SILVA FE, LENKE LG. Adult degenerative scoliosis: evaluation and management. Neurosurg Focus. 2010;28(3):E1. [6] SCHWAB F, UNGAR B, BLONDEL B, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976). 2012;37(12):1077-1082. [7] BERJANO P, LAMARTINA C. Classification of degenerative segment disease in adults with deformity of the lumbar or thoracolumbar spine. Eur Spine J. 2014;23(9):1815-1824. [8] LAFAGE R, SCHWAB F, CHALLIER V, et al. Defining Spino-Pelvic Alignment Thresholds: Should Operative Goals in Adult Spinal Deformity Surgery Account for Age? Spine (Phila Pa 1976). 2016;41(1):62-68. [9] DIEBO BG, VARGHESE JJ, LAFAGE R, et al. Sagittal alignment of the spine: What do you need to know? Clin Neurol Neurosurg. 2015;139: 295-301. [10] HASEGAWA K, OKAMOTO M, HATSUSHIKANO S, et al. Normative values of spino-pelvic sagittal alignment, balance, age, and health-related quality of life in a cohort of healthy adult subjects. Eur Spine J. 2016;25(11):3675-3686. [11] SCHWAB F, FARCY JP, BRIDWELL K, et al. A clinical impact classification of scoliosis in the adult. Spine (Phila Pa 1976). 2006;31(18):2109-2114. [12] FAIRBANK JC. Oswestry disability index. J Neurosurg Spine. 2014;20(2): 239-241. [13] TANG JA, SCHEER JK, SMITH JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery. 2015;76 Suppl 1:S14-S21,S21. [14] ZHANG HC, YU HL, YANG HF, et al. Short-segment decompression/fusion versus long-segment decompression/fusion and osteotomy for Lenke-Silva type VI adult degenerative scoliosis. Chin Med J (Engl). 2019;132(21):2543-2549. [15] ZHANG HC, ZHANG ZF, WANG ZH, et al. Optimal Pelvic Incidence Minus Lumbar Lordosis Mismatch after Long Posterior Instrumentation and Fusion for Adult Degenerative Scoliosis. Orthop Surg. 2017;9(3):304-310. [16] PICHELMANN MA, LENKE LG, BRIDWELL KH, et al. Revision rates following primary adult spinal deformity surgery: six hundred forty-three consecutive patients followed-up to twenty-two years postoperative. Spine (Phila Pa 1976). 2010;35(2):219-226. [17] MACIEJCZAK A, JABLONSKA-SUDOL K. Correlation between correction of pelvic balance and clinical outcomes in mid- and low-grade adult isthmic spondylolisthesis. Eur Spine J. 2017;26(12):3112-3121. [18] LE HUEC JC, FAUNDEZ A, DOMINGUEZ D, et al. Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: a literature review. Int Orthop. 2015;39(1):87-95. [19] GLASSMAN SD, BRIDWELL K, DIMAR JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005; 30(18):2024-2029. [20] GELB DE, LENKE LG, BRIDWELL KH, et al. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine (Phila Pa 1976). 1995;20(12):1351-1358. [21] SCHWAB F, PATEL A, UNGAR B, et al. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010;35(25):2224-2231. [22] CHEN YY, PAO JL, LIAW CK, et al. Image changes of paraspinal muscles and clinical correlations in patients with unilateral lumbar spinal stenosis. Eur Spine J. 2014;23(5):999-1006. [23] BANNO T, ARIMA H, HASEGAWA T, et al. The Effect of Paravertebral Muscle on the Maintenance of Upright Posture in Patients With Adult Spinal Deformity. Spine Deform. 2019;7(1):125-131. [24] LE HUEC JC, THOMPSON W, MOHSINALY Y, et al. Sagittal balance of the spine. Eur Spine J. 2019;28(9):1889-1905. |
| [1] | Cao Sheng, Kong Lingwei, Xu Kun, Sun Zhijie. Correlation of cervical sagittal force line parameters with degenerative segment and Pfirrmann classification in patients with cervical intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1319-1324. |
| [2] | Wang Jianye, Liu Xin, Tian Lin, Sun Ning, Li Yuefei, Bi Jingwei, Liu Changzhen, Sun Zhaozhong . Measuring the position relation between nerve tissue and bony structure in lumbar spinal canal decompression area by constructing a three-dimensional model of the lumbar spine [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 539-546. |
| [3] | Zhang Hanshuo, Ding Yu, Jiang Qiang, Lu Zhengcao, Lian Shilin, Li Tusheng. Biomechanical stability and finite element analysis of endoscopic LOVE decompression technique and endoscopic unilateral laminotomy for bilateral decompression technique for lumbar spinal stenosis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(13): 1981-1986. |
| [4] | Jiang Huanchang, Zhang Zhaofei, Liang De, Jiang Xiaobing, Yang Xiaodong, Liu Zhixiang. Comparison of advantages between unilateral multidirectional curved and straight vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1407-1411. |
| [5] | Yu Chengxiang, Liu Lehong, Li Wenbo, Chen Jinshi, Ran Chunlei, Wang Zhongping. Correlation between spine-pelvic sagittal parameters and prognosis of vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1412-1417. |
| [6] | Li Yuqiao, Sun Tianwei, Ma Bin, Zhou Zhaohong, Dong Runbei, Wu Haiyang. A comparative study of imaging parameters and quality of life scores between subtypes of lumbar spondylolisthesis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 943-948. |
| [7] | Pan Xian, Liang Simin, Liu Bingxia, Song Tianzeng, Ma He, Wu Peng, Ge Zhaohui. Correlation between pelvic incidence-lumbar lordosis and clinical outcome in patients with degenerative lumbar scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(33): 5370-5375. |
| [8] | Yao Rubin, Wang Shiyong, Yang Kaishun. Minimally invasive transforaminal lumbar interbody fusion for treatment of single-segment lumbar spinal stenosis improves lumbar-pelvic balance [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1387-1392. |
| [9] | Xie Jiang, Dai Jie, Li Hui, Zhu Xu. Biomechanical analysis of sagittal balance restoration of ankylosing kyphosis based on pelvic sagittal parameters [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(30): 4762-4766. |
| [10] | Tian Yang, Tang Chao, Liao Yehui, Tang Qiang, Ma Fei, Zhong Dejun. Consistency and repeatability of CT and MRI in measurement of spinal canal area in patients with lumbar spinal stenosis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3882-3887. |
| [11] | Li Qiang, Li Jun, Luan Jian, Jin Canghai, Hao Meng, Lin Yong. Bone cement distribution of percutaneous curved vertebroplasty for the treatment of osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2466-2471. |
| [12] | Chen Jiang, Li Jinyu, Zheng Chenying, Bai Chunxiao, Zhang Fan, Liu Chuyin, Zhao Xueqian, Yuan Qiaomei, Di Xueshi, Kang Shengqian, Jia Yusong . Changes in sagittal parameters of cervical spine after double-segment artificial cervical disc replacement and anterior cervical discectomy and fusion [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2341-2346. |
| [13] | Zhang Le, Pan Bin, Ruan Ruxin, Guo Kaijin. Effect of lumbopelvic sagittal parameters on secondary adjacent vertebral fracture after percutaneous kyphoplasty for osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2370-2374. |
| [14] | Wang Jing, Xu Shuai, Liu Haiying. Hidden blood loss during posterior lumbar interbody fusion in lumbar spinal stenosis patients with and without rheumatoid arthritis [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(33): 5307-5314. |
| [15] | Cao Bin, Zuo Yuqiang, Du Hanyang, Yu Haiquan, Su Jingyang, Meng Haoyong. Correlation of saggital parameters of cervical and thoracic junction areas in asymptomatic adults [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(33): 5354-5357. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||