[1] BURR DB, GALLANT MA. Bone remodelling in osteoarthritis. Nat Rev Rheumatol. 2012;8(11):665-673.
[2] MADRY H, VAN DIJK CN, MUELLER-GERBL M. The basic science of the subchondral bone. Knee Surg Sports Traumatol Arthrosc. 2010; 18(4):419-433.
[3] LI G, YIN J, GAO J, et al. Subchondral bone in osteoarthritis: insight into risk factors and microstructural changes. Arthritis Res Ther. 2013; 15(6):223.
[4] WEBER A, CHAN P, WEN C. Do immune cells lead the way in subchondral bone disturbance in osteoarthritis? Prog Biophys Mol Biol. 2019;148:21-31.
[5] SU W, LIU G, LIU X, et al. Angiogenesis stimulated by elevated PDGF-BB in subchondral bone contributes to osteoarthritis development. JCI Insight. 2020;5(8):e135446.
[6] JAIPRAKASH A, PRASADAM I, FENG JQ, et al. Phenotypic characterization of osteoarthritic osteocytes from the sclerotic zones: a possible pathological role in subchondral bone sclerosis. Int J Biol Sci. 2012;8(3):406-417.
[7] BONEWALD LF. The amazing osteocyte. J Bone Miner Res. 2011;26(2): 229-238.
[8] ZHOU X, CAO H, YUAN Y, et al. Biochemical Signals Mediate the Crosstalk between Cartilage and Bone in Osteoarthritis. Biomed Res Int. 2020;2020:5720360.
[9] LORENZ J, GRASSEL S. Experimental osteoarthritis models in mice. Methods Mol Biol. 2014;1194:401-419.
[10] KADRI A, EA HK, BAZILLE C, et al. Osteoprotegerin inhibits cartilage degradation through an effect on trabecular bone in murine experimental osteoarthritis. Arthritis Rheum. 2008;58(8):2379-2386.
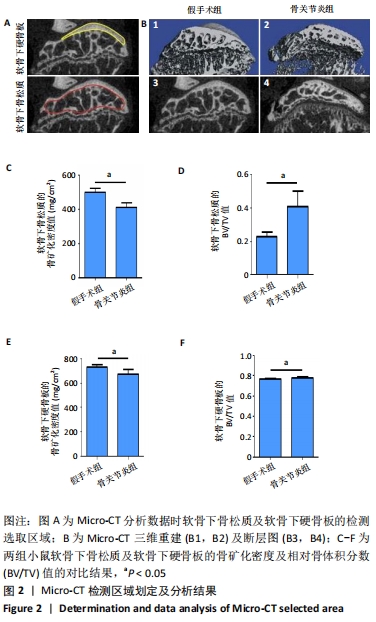
[11] FANG H, HUANG L, WELCH I, et al. Early Changes of Articular Cartilage and Subchondral Bone in The DMM Mouse Model of Osteoarthritis. Sci Rep. 2018;8(1):2855.
[12] LORENZ J, GRASSEL S. Experimental osteoarthritis models in mice. Methods Mol Biol. 2014;1194:401-419.
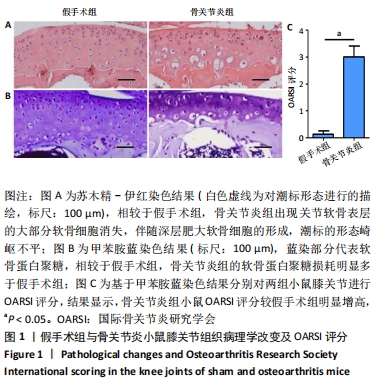
[13] GLASSON SS, CHAMBERS MG, VAN DEN BERG WB, et al. The OARSI histopathology initiative - recommendations for histological assessments of osteoarthritis in the mouse. Osteoarthritis Cartilage. 2010;18 Suppl 3:S17-S23.
[14] DOBSON GP, LETSON HL, GRANT A, et al. Defining the osteoarthritis patient: back to the future. Osteoarthritis Cartilage. 2018;26(8):1003-1007.
[15] DONELL S. Subchondral bone remodelling in osteoarthritis. EFORT Open Rev. 2019;4(6):221-229.
[16] MAZUR CM, WOO JJ, YEE CS, et al. Osteocyte dysfunction promotes osteoarthritis through MMP13-dependent suppression of subchondral bone homeostasis. Bone Res. 2019;7:34.
[17] STAPLEDON C, TSANGARI H, SOLOMON LB, et al. Human osteocyte expression of Nerve Growth Factor: The effect of Pentosan Polysulphate Sodium (PPS) and implications for pain associated with knee osteoarthritis. PLoS One. 2019;14(9):e222602.
[18] 钟京谕, 姚伟武. 骨关节炎中软骨及软骨下骨间信号交流[J]. 国际骨科学杂志,2019,40(4):207-210,214.
[19] GOLDRING SR, GOLDRING MB. Changes in the osteochondral unit during osteoarthritis: structure, function and cartilage-bone crosstalk. Nat Rev Rheumatol. 2016;12(11):632-644.
[20] HOPWOOD B, TSYKIN A, FINDLAY DM, et al. Microarray gene expression profiling of osteoarthritic bone suggests altered bone remodelling, WNT and transforming growth factor-beta/bone morphogenic protein signalling. Arthritis Res Ther. 2007;9(5):R100.
[21] GOLDRING SR. The role of bone in osteoarthritis pathogenesis. Rheum Dis Clin North Am. 2008;34(3):561-571.
[22] LI M, XIE WQ, HE M, et al. Characterization of the Subchondral Bone and Pain Behavior Changes in a Novel Bipedal Standing Mouse Model of Facet Joint Osteoarthritis. Biomed Res Int. 2020;2020:8861347.
[23] NAKASA T, IKUTA Y, OTA Y, et al. Bone Mineralization Changes in the Subchondral Bone of the Medial Gutter in Chronic Lateral Ankle Instability. Foot Ankle Int. 2020,41(11):1419-1426.
[24] 常亮, 秦江辉, 史冬泉, 等. 骨关节炎与软骨下骨研究进展[J]. 中华骨与关节外科杂志,2019,12(10):827-832.
[25] 李强, 张柳. 骨性关节炎中软骨下骨与软骨退变的关系研究进展[J]. 中国修复重建外科杂志,2009,23(2):245-248.
[26] MEYER EG, BAUMER TG, SLADE JM, et al. Tibiofemoral contact pressures and osteochondral microtrauma during anterior cruciate ligament rupture due to excessive compressive loading and internal torque of the human knee. Am J Sports Med. 2008;36(10):1966-1977.
[27] INTEMA F, HAZEWINKEL HA, GOUWENS D, et al. In early OA, thinning of the subchondral plate is directly related to cartilage damage: results from a canine ACLT-meniscectomy model. Osteoarthritis Cartilage. 2010;18(5):691-698.
[28] WANG Y, WLUKA AE, PELLETIER JP, et al. Meniscal extrusion predicts increases in subchondral bone marrow lesions and bone cysts and expansion of subchondral bone in osteoarthritic knees. Rheumatology (Oxford). 2010;49(5):997-1004.
[29] 邵毅杰, 姜华晔, 高超, 等. 膝关节应力负荷减少对小鼠早期骨关节炎软骨和软骨下骨的影响[J]. 中国组织工程研究,2019,23(35): 5611-5618.
[30] GOLDRING MB, GOLDRING SR. Articular cartilage and subchondral bone in the pathogenesis of osteoarthritis. Ann N Y Acad Sci. 2010;1192: 230-237.
[31] GALLI C, PASSERI G, MACALUSO M. Osteocytes and WNT: the mechanical control of bone formation. J Dent Res. 2010;89(4):331-343.
[32] ROBLING AG, CASTILLO AB, TURNER CH. Biomechanical and molecular regulation of bone remodeling. Annu Rev Biomed Eng. 2006;8:455-498.
[33] ZHENG CX, SUI BD, QIU XY, et al. Mitochondrial Regulation of Stem Cells in Bone Homeostasis. Trends Mol Med. 2020;26(1):89-104.
[34] HASEGAWA T, KIKUTA J, ISHII M. Imaging the Bone-Immune Cell Interaction in Bone Destruction. Front Immunol. 2019;10:596.
[35] PLOTKIN LI, BRUZZANITI A. Molecular signaling in bone cells: Regulation of cell differentiation and survival. Adv Protein Chem Struct Biol. 2019; 116:237-281.
[36] DAI G, XIAO H, LIAO J, et al. Osteocyte TGFbeta1Smad2/3 is positively associated with bone turnover parameters in subchondral bone of advanced osteoarthritis. Int J Mol Med. 2020;46(1):167-178.
[37] ZHU S, ZHU J, ZHEN G, et al. Subchondral bone osteoclasts induce sensory innervation and osteoarthritis pain. J Clin Invest. 2019;129(3): 1076-1093.
[38] BONEWALD LF, JOHNSON ML. Osteocytes, mechanosensing and Wnt signaling. Bone. 2008;42(4):606-615.
[39] PASZTY C, TURNER CH, ROBINSON MK. Sclerostin: a gem from the genome leads to bone-building antibodies. J Bone Miner Res. 2010; 25(9):1897-1904.
[40] BRUNKOW ME, GARDNER JC, VAN NESS J, et al. Bone dysplasia sclerosteosis results from loss of the SOST gene product, a novel cystine knot-containing protein. Am J Hum Genet. 2001;68(3):577-589.
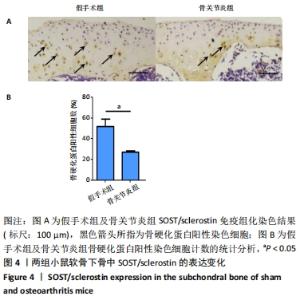
[41] LI J, XUE J, JING Y, et al. SOST Deficiency Aggravates Osteoarthritis in Mice by Promoting Sclerosis of Subchondral Bone. Biomed Res Int. 2019;2019:7623562.
|