Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (3): 376-382.doi: 10.12307/2022.062
Previous Articles Next Articles
Correlation between blood loss during primary total knee arthroplasty and hypoalbuminemia and hypocalcemia after arthroplasty
Qu Pengfei, Wang Huisheng, Li Xi
- Department of Sports Medicine and Joint Surgery, People’s Hospital of Liaoning Province, Shenyang 110000, Liaoning Province, China
-
Received:2021-03-05Revised:2021-03-06Accepted:2021-04-10Online:2022-01-28Published:2021-10-27 -
Contact:Wang Huisheng, Master, Associate chief physician, Department of Sports Medicine and Joint Surgery, People’s Hospital of Liaoning Province, Shenyang 110000, Liaoning Province, China -
About author:Qu Pengfei, Master, Department of Sports Medicine and Joint Surgery, People’s Hospital of Liaoning Province, Shenyang 110000, Liaoning Province, China
CLC Number:
Cite this article
Qu Pengfei, Wang Huisheng, Li Xi. Correlation between blood loss during primary total knee arthroplasty and hypoalbuminemia and hypocalcemia after arthroplasty[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 376-382.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
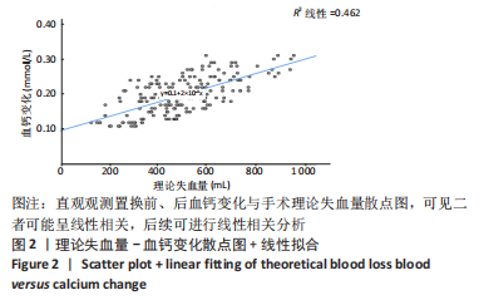
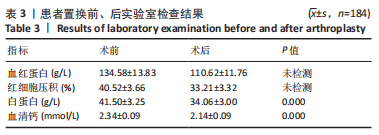
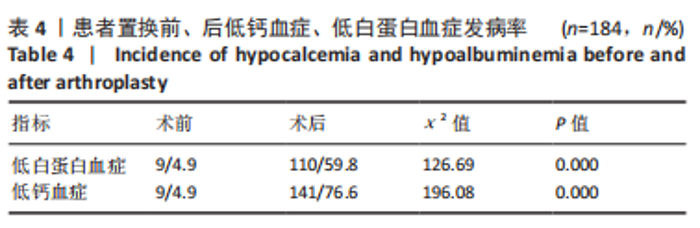
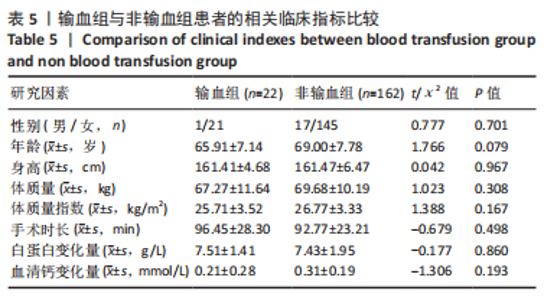
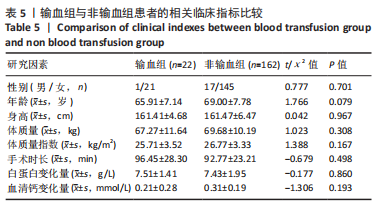
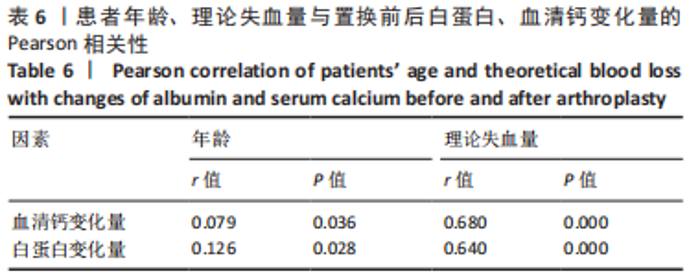
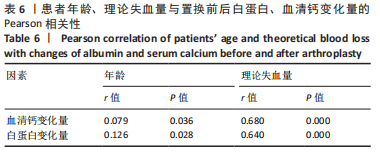
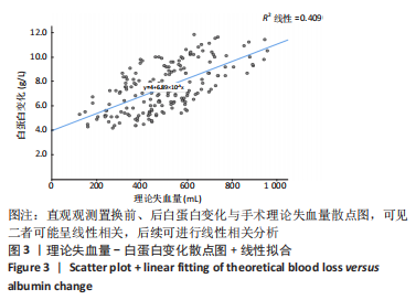
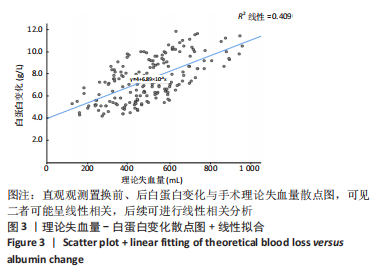
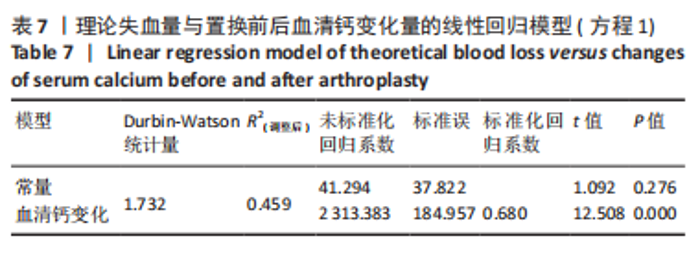
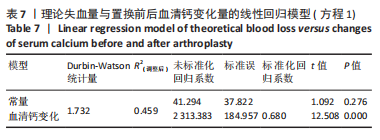
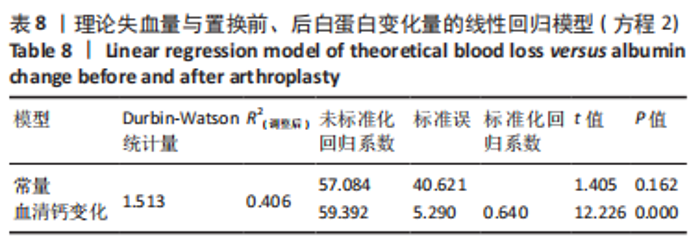
患者年龄与置换前后血清钙、白蛋白变化量均呈显著正相关性(P < 0.05),上述2个指标与患者年龄的相关性大小为:白蛋白变化量(r=0.126) >血清钙变化量(r=0.079)。 2.5.2 理论失血量与白蛋白变化量、血清钙变化量之间的关系 应用Pearson相关性分析法分析理论失血量与置换前后白蛋白变化量、血清钙变化量均呈极显著正相关性(P < 0.01),上述各指标与理论失血量相关性大小依次为血清钙变化量(r=0.680) >白蛋白变化量(r=0.640),详见表6。 2.6 散点图 分别绘制手术失血量与血清钙变化量、白蛋白变化量、手术时长的散点图。直观观察上述指标走势并行线性拟合观察其是否呈线性,见图2-4,若符合线性关系,后续行线性回归分析。观察发现手术时长与理论失血量不符合线性关系,在后续研究中予以排除。"
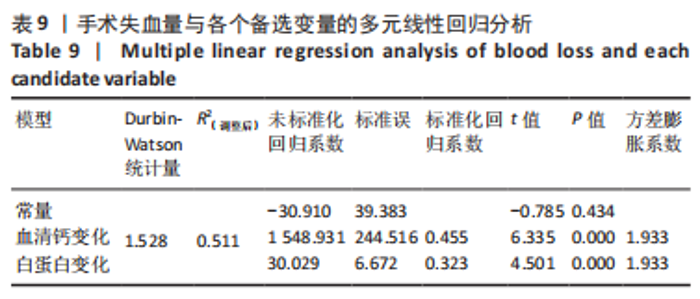
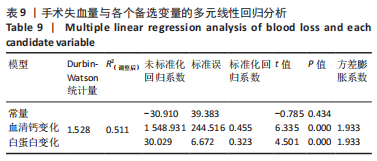
将此次试验数据统计得到的理论出血量平均值499.07 mL代入方程2可得:此时置换前后白蛋白变化量为7.44 g/L。 2.7.3 建立理论失血量与置换前后白蛋白变化量、血清钙变化量之间关系的多元线性回归方程 以术后白蛋白变化量(g/L)、 血钙变化量(mmol/L)为自变量,以理论失血量(mL)为因变量,进行多元线性回归,见表9。 由表可知,手术失血量与置换前后血清钙变化、白蛋白变化呈极显著相关性(P < 0.01);该线性回归模型的R2(调整后)=0.511,P < 0.01,Durbin-Watson统计量=1.528。以理论失血量(Y)为因变量,以血清钙变化量(X1)、白蛋白变化量(X2)为自变量,建立最优线性回归方程:Y=-30.91+1 548.931X1+30.029X2(方程3),即当理论失血量每增加100 mL,在另一变量不变的情况下,血清钙变化量(X1)增加0.065 mmol/L或白蛋白变化量(X2)增加3.33 g/L。 "
| [1] LI J, ZHU H, LIAO R. Enhanced recovery after surgery (ERAS) pathway for primary hip and knee arthroplasty: study protocol for a randomized controlled trial. Trials. 2019;20:599. [2] TILLE E, MYSLIWIETZ J, BEYER F, et al.Intraarticular use of tranexamic acid reduces blood loss and transfusion rate after primary total knee arthroplasty. BMC Musculoskelet Disord. 2019;20(1):341. [3] LI ZJ, ZHAO MW, ZENG L. Additional Dose of Intravenous Tranexamic Acid after Primary Total Knee Arthroplasty Further Reduces Hidden Blood Loss. Chin Med J (Engl). 2018;131(6):638-642. [4] VORA M, SING DC, YI PH, et al. Hypoalbuminemia is a risk factor for predicting early postoperative complications after proximal humerus fracture fixation. J Orthop. 2019;19:106-110. [5] BLEVINS K, AALIREZAIE A, SHOHAT N, et al. Malnutrition and the Development of Periprosthetic Joint Infection in Patients Undergoing Primary Elective Total Joint Arthroplasty. J Arthroplasty. 2018;33(9): 2971-2975. [6] NWACHUKWU BU, DY CJ, BURKET JC, et al. Risk for Complication after Total Joint Arthroplasty at a Center of Excellence: The Impact of Patient Travel Distance. J Arthroplasty. 2015;30:1058-1061. [7] ROBINSON TN, RAEBURN CD, TRAN ZV, et al. Postoperative Delirium in the Elderly: Risk Factors and Outcomes. Ann Surg. Ann Surg. 2009; 249(1):173-178. [8] YATES AJ JR; AMERICAN ASSOCIATION OF HIP AND KNEE SURGEONS EVIDENCE-BASED MEDICINE COMMITTEE. Postoperative prophylactic antibiotics in total joint arthroplasty. Arthroplast Today. 2018;4(1): 130-131. [9] SCHIAVON CA, BERSCH-FERREIRA AC, SANTUCCI EV, et al. Effects of Bariatric Surgery in Obese Patients With Hypertension: The GATEWAY Randomized Trial (Gastric Bypass to Treat Obese Patients With Steady Hypertension). Circulation. 2018;137(11):1132-1142. [10] YU Q, LIU K, MA D, et al. Do Symptoms and Serum Calcium Levels Affect the Results of Surgical Treatment of Primary Hyperparathyroidism? Biomed Res Int. 2019;2019:2150159. [11] GAI P, SUN H, SUI L, et al. Hypocalcaemia After Total Knee Arthroplasty and its Clinical Significance. Anticancer Res. 2016;36(3):1309-1311. [12] 刘子桃, 黄永明. 膝关节置换患者围手术期钠、钾、钙离子水平的变化及临床意义[J]. 当代医学,2012,18(23):22-24. [13] MATTSSON JP, VÄÄNÄNEN K, WALLMARK B, et al. Omeprazole and bafilomycin, two proton pump inhibitors: Differentiation of their effects on gastric, kidney and bone H+-translocating ATPases. Biochim Biophys Acta. 1991;1065(2):261-268. [14] BAHTIRI E, ISLAMI H, HOXHA R, et al. Proton pump inhibitor use for 12 months is not associated with changes in serum magnesium levels: a prospective open label comparative study. Turk J Gastroenterol. 2017;28(2):104-109. [15] LEE L, RAMOS-ALVAREZ I, ITO T, et al. Insights into Effects/Risks of Chronic Hypergastrinemia and Lifelong PPI Treatment in Man Based on Studies of Patients with Zollinger–Ellison Syndrome. Int J Mol Sci. 2019;20(20):5128. [16] BIHORAC A, ROSS EA. Continuous Venovenous Hemofiltration With Citrate-Based Replacement Fluid: Efficacy, Safety, and Impact on Nutrition. Am J Kidney Dis. 2005;46(5):908-918. [17] KUO IY, EHRLICH BE. Signaling in muscle contraction. Cold Spring Harb Perspect Biol. 2015;7(2):a006023. [18] HARVEY NC, BIVER E, KAUFMAN J, et al. The role of calcium supplementation in healthy musculoskeletal ageing : An expert consensus meeting of the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) and the International Foundation for Osteoporosis (IOF). Osteoporos Int. 2017;28(2):447-462. [19] ANASTASIO AT, FARLEY KX, BODEN SD, et al. Modifiable, Postoperative Risk Factors for Delayed Discharge Following Total Knee Arthroplasty: The Influence of Hypotension and Opioid Use. J Arthroplasty. 2020; 35(1):82-88. [20] TANG MJ, DING SB, HU WY. Fibrinogen and Albumin Score Changes during Preoperative Treatment Can Predict Prognosis in Patients with Locally Advanced Rectal Cancer. Gastroenterol Res Pract. 2019; 2019:3514586. [21] LAI R, CHEN T, WU Z, et al. Associations between body mass index and mortality in acute-on-chronic liver failure patients. Ann Hepatol. 2019;18(6):893-897. [22] UENO K, AJIKI T, TSUGAWA D, et al. Effectiveness of omega-3 fatty acid administration on completion rate of adjuvant chemotherapy for biliary tract cancer: study protocol for a single-centre, open-label, single-arm, historically controlled study. BMJ Open. 2019;9(8):e029915. [23] OKAMOTO N, AMANO N, NAKAMURA T, et al. Relationship between tooth loss, low masticatory ability, and nutritional indices in the elderly: a cross-sectional study. BMC Oral Health. 2019;19(1):110. [24] SŁOTWIŃSKI R, SARNECKA A, DĄBROWSKA A, et al. Innate immunity gene expression changes in critically ill patients with sepsis and disease-related malnutrition. Cent Eur J Immunol. 2015;40(3):311-324. [25] HE Y, XIAO J, SHI Z, et al. Supplementation of enteral nutritional powder decreases surgical site infection, prosthetic joint infection, and readmission after hip arthroplasty in geriatric femoral neck fracture with hypoalbuminemia. J Orthop Surg Res. 2019;14(1):292. [26] ALFARGIENY R, BODALAL Z, BENDARDAF R, et al. Nutritional status as a predictive marker for surgical site infection in total joint arthroplasty. Avicenna J Med. 2015;5(4):117-122. [27] KHANNA R, YI PH, SING DC, et al. Hypoalbuminemia Is Associated With Septic Revisions After Primary Surgery and Postoperative Infection After Revision Surgery. Spine (Phila Pa 1976). 2018;43(6):454-460. [28] IBRAHIM MS, TWAIJ H, GIEBALY DE, et al. Enhanced recovery in total hip replacement: a clinical review. Bone Joint J. 2013;95-B(12):1587-1594. [29] PEARSON TC, GUTHRIE DL, SIMPSON J, et al. Interpretation of measured red cell mass and plasma volume in adults: Expert Panel on Radionuclides of the International Council for Standardization in Haematology. Br J Haematol. 1995;89(4):748-756. [30] GOOD L, PETERSON E, LISANDER B. Tranexamic acid decreases external blood loss but not hidden blood loss in total knee replacement. Br J Anaesth. 2003;90(5):596-599. [31] MARX G, SCHUERHOLZ T, PEDDER S, et al. Blood volume measurements using an integrated fiberoptic monitoring system in a porcine septic shock model. Crit Care Med. 2006;34:1483-1488. |
| [1] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [2] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [3] | Yuan Jun, Yang Jiafu. Hemostatic effect of topical tranexamic acid infiltration in cementless total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 873-877. |
| [4] | Wan Dadi, Duan Xiangrui, Fan Xinchao, Yuan Ye, Huang Teng, Pan Dikang, Liu Jingyan, Li Xicheng. Efficacy of posterior cruciate ligament retaining versus posterior stabilized prostheses in total knee arthroplasty: a systematic review and a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(36): 5897-5904. |
| [5] | Gao Tianhao, Qian Huifang, Yang Shangliang, Xin Chaofei, Lu Shitao, Xu Jianzhong. Calcium sulfate antibiotic carrier in the treatment of periprosthetic infection after arthroplasty and its effect on serum calcium [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(30): 4823-4827. |
| [6] | Lü Zexiang, Wu Jutai, Jiang Jian, Feng Xiao, Li Tengfei, Wang Yehua. Effect of tranexamic acid combined with carbazochrome sodium sulfonate on blood loss and safety after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 386-390. |
| [7] | Wang Hao, Wang Yitao, Lü Zexiang, Li Tengfei, Wang Shaolong, Wang Yehua. Effect of repeated intravenous tranexamic acid in the perioperative period of proximal femoral nail antirotation for femoral intertrochanteric fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3319-3323. |
| [8] | Fu Panfeng, Shang Wei, Kang Zhe, Deng Yu, Zhu Shaobo. Efficacy of anterolateral minimally invasive approach versus traditional posterolateral approach in total hip arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3409-3415. |
| [9] | Liu Jinlei, Yin Li, Zhang Yi, Wang Haitao, Li Zhuangyan, Xia Peige, Qiao Renqiu. Effects of intravenous tranexamic acid combined with periarticular multipoint injection of tranexamic acid cocktail on blood loss and pain after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2833-2839. |
| [10] | Zhong Yuanming, Fu Xiaopeng, Xu Wei, Zhao Qingrui, Huang Yong, Ye Weiquan. Nicardipine controlled hypotension applied to perioperative blood loss in orthopedics: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2930-2937. |
| [11] | Gao Zhixiang, Xiao Cong, Yang Hongtao, Meng Xiangyu. Statistical decision tree model analysis on hidden blood loss in the perioperative period of thoracolumbar burst fracture accompanied with neurological deficiency [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2364-2369. |
| [12] | Chen Wang, Feng Shuo, Zhang Yu, Chen Xiangyang. Efficacy and safety of tranexamic acid and epsilon-aminocaproic acid in reducing perioperative blood loss during total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2430-2436. |
| [13] | Gao Fenghe, Chen Tongying, Lin Jiebin, Liang Zujian. Efficacy and safety of tranexamic acid combined with rivaroxaban in primary total knee and hip arthroplasties: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2453-2460. |
| [14] | Zheng Zhihui, Chen Sheng, Guan Keli, Zheng Xun, Chen Haibo, Zeng Qingqiang. Relationship between blood loss of proximal femoral nail anti-rotation fixation and local use combined with intravenous injection of tranexamic acid [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(9): 1359-1364. |
| [15] | Jiang Biantong, Zhang Zhigang, Jin Xiu, Wang Haiye, Wu Yuchen, Zhang Caiyun. Effects of different calcium supplementation pathways on calcium ion in calcium-free regional citrate anticoagulation-continuous renal replacement therapy: study protocol for a prospective randomized cross-over trial [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(5): 726-730. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||