[1] XU R, GRABOW R, EBRAHEIM NA, et al. Anatomic considerations of a modified anterior approach to the cervicothoracic junction.Am J Orthop(Belle Mead NJ). 2000; 29(1):37-40.
[2] MILLER DJ, LANG FF, WALSH GL, et al.Coaxial double-lumen methylmethacrylate reconstruction in the anterior cervical and upper thoracic spine after tumor resection.J Neurosurg. 2000;92(2 Suppl):181-190.
[3] 陈伟,王文军.上胸椎前路手术入路的研究综述[J],中国医药指南, 2010,8(13):34-35.
[4] CAUCHOIX J, BINET JP. Anterior surgical approaches to the spine.Ann R Coll Surg Engl.1957;21(4):234-43.
[5] 杨渊,温超海,李小峰,等.上胸椎手术前方入路研究进展[J].辽宁中医药大学学报, 2013,15(5):8-10.
[6] 侯俊.经腋中线胸腔入路显露上胸椎的解剖学研究[D].南宁:广西医科大学,2014.
[7] 张笑汝,陈前芬.经腋中线胸腔入路治疗上中胸椎结核[J].分子影像学杂志,2016,39(3):221-224.
[8] 刘会江,詹新立,肖增明,等. 上胸椎前路钛板与颈前路钛板内固定装置的拔出强度实验[J].中国组织工程研究, 2012,16(4): 605-608.
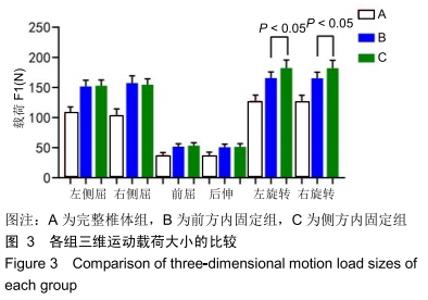
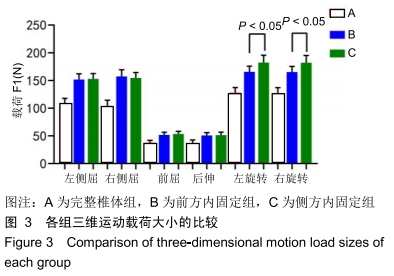
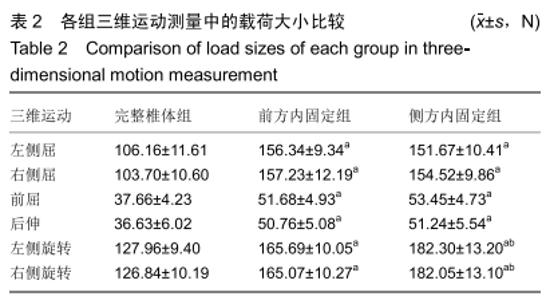
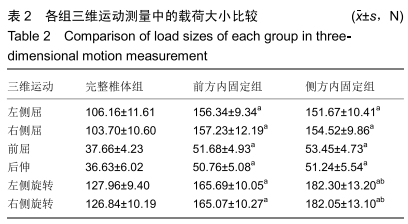
[9] 罗巨利,詹新立,肖增明,等. 体外生物力学评价上胸椎前路钛板内固定装置的三维运动稳定性[J].中国组织工程研究与临床康复,2011,15(17):3119-3123.
[10] CRAWFORD NR, BRANTLEY AG, DICKMAN CA, et al. An apparatus for applying pure nonconstraining moments to spine segments in vitro.Spine(Phila Pa 1976). 1995;20(19): 2097-2100.
[11] STAUDT MD, RABIN D, BAAJ AA, et al. Biomechanical evaluation of the ProDisc-C stability following graded posterior cervical injury.J Neurosurg Spine. 2018;29(5): 515-524.
[12] KAO FC, TSAI TT, NIU CC, et al.One-stage posterior approaches for treatment of thoracic spinal infection: Transforaminal and costotransversectomy, compared with anterior approach with posterior instrumentation. Medicine (Baltimore).2017;96(42):e8352.
[13] LAM FC, GROFF MW. An anterior approach to spinal pathology of the upper thoracic spine through a partial manubriotomy.J Neurosurg Spine.2011;15(5):467-471.
[14] 张笑汝.经腋中线胸腔入路病灶清除减压植骨内固定治疗上中胸椎结核的临床研究[D].南宁:广西医科大学,2014.
[15] 于德军,刘丽晶,金松,等.胸椎钉棒系统置入方式的生物力学特征[J].中国组织工程研究,2015,19(22):3579-3583.
[16] WILKE HJ, JUNGKUNZ B, WENGER K, et al.Spinal segment range of motion as a function of in vitro test conditions: effects of exposure period, accumulated cycles, angular-deformation rate, and moisture condition.Anat Rec.1998;251(1):15-19.
[17] WANG JL, PARNIANPOUR M, SHIRAZI-ADL A, et al. Viscoelastic finite-element analysis of a lumbar motion segment in combined compression and sagittal flexion. Effect of loading rate.Spine(Phila Pa 1976).2000;25(3):310-318.
[18] WILKE HJ, KETTLER A, CLAES LE.Are sheep spines a valid biomechanical model for human spines?Spine(Phila Pa 1976). 1997;22(20):2365-2374.
[19] WILKE HJ, KRISCHAK S, CLAES L. Biomechanical comparison of calf and human spines.J Orthop Res. 1996; 14(3):500-503.
[20] 刘冲,詹新立,肖增明,等.上胸椎前路钛板内固定系统在山羊胸椎椎体次全切除植骨内固定术中的应用效果[J].中国脊柱脊髓杂志,2013,23(8):744-748.
[21] 镫邦芳,冷重光.胸椎、腰椎器械固定的生物力学[J].日本医学介绍,1988,9(8):350-351,367.
[22] MIELE VJ, PANJABI MM, BENZEL EC. Anatomy and biomechanics of the spinal column and cord.Handb Clin Neurol.2012;109:31-43.
[23] PANJABI MM, DURANCEAU JS, OXLAND TR, et al. Multidirectional instabilities of traumatic cervical spine injuries in a porcine model.Spine(Phila Pa 1976). 1989;14(10): 1111-1115.
[24] PANJABI MM, ISOMI T, WANG JL. Loosening at the screw-vertebra junction in multilevel anterior cervical plate constructs.Spine(Phila Pa 1976).1999;24(22):2383-2388.
[25] SHASTI M, KOENIG SJ, NASH AB, et al.Biomechanical evaluation of lumbar lateral interbody fusion for the treatment of adjacent segment disease.Spine J.2019;19(3):545-551.
[26] KETTLER A, WILKE HJ, HAID C, et al.Effects of specimen length on the monosegmental motion behavior of the lumbar spine.Spine(Phila Pa 1976).2000;25(5):543-550.
[27] CUNNINGHAM BW, SEFTER JC, SHONO Y, et al.Static and cyclical biomechanical analysis of pedicle screw spinal constructs.Spine(Phila Pa 1976).1993;18(12):1677-1688.
[28] EBELKE DK, ASHER MA, NEFF JR, et al.Survivorship analysis of VSP spine instrumentation in the treatment of thoracolumbar and lumbar burst fractures. Spine (Phila Pa 1976).1991;16(8 Suppl):S428-S432.
[29] WANG K, ZHANG ZJ, WANG JL, et al.Risk Factor of Failed Reduction of Posterior Ligamentatoxis Reduction Instrumentation in Managing Thoracolumbar Burst Fractures: A Retrospective Study.World Neurosurg.2018;119:e475-e481.
[30] LAZARO BC, DENIZ FE, BRASILIENSE LB, et al. Biomechanics of thoracic short versus long fixation after 3-column injury.J Neurosurg Spine.2011;14(2):226-234.
|