Chinese Journal of Tissue Engineering Research ›› 2019, Vol. 23 ›› Issue (32): 5203-5208.doi: 10.3969/j.issn.2095-4344.1460
Previous Articles Next Articles
Total knee arthroplasty for osteoarthritis with femoral bowing: comparison of conventional method and computer-assisted navigation
Qing Mingsong, Peng Jiachen, Yang Lidan, Zhao Chuntao
- Department of Joint Surgery, Affiliated Hospital of Zunyi Medical University, Zunyi 563000, Guizhou Province, China
-
Online:2019-11-18Published:2019-11-18 -
Contact:Peng Jiachen, MD, Professor, Chief physician, Department of Joint Surgery, Affiliated Hospital of Zunyi Medical University, Zunyi 563000, Guizhou Province, China -
About author:Qing Mingsong, Master candidate, Department of Joint Surgery, Affiliated Hospital of Zunyi Medical University, Zunyi 563000, Guizhou Province, China
CLC Number:
Cite this article
Qing Mingsong, Peng Jiachen, Yang Lidan, Zhao Chuntao. Total knee arthroplasty for osteoarthritis with femoral bowing: comparison of conventional method and computer-assisted navigation[J]. Chinese Journal of Tissue Engineering Research, 2019, 23(32): 5203-5208.
share this article
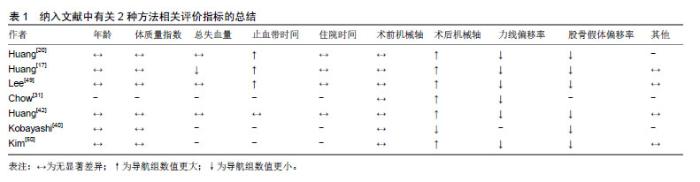
2.1 股骨侧弓定义及测量 股骨在解剖上存在向前的弓形[10],但在冠状位上同样存在着侧弓。Tang等[11]不仅在下肢全长侧位片上发现股骨存在着朝前的弓状弯曲,而且在下肢全长正位片上还发现存在着股骨侧向的弓状弯曲,当侧弓程度超过一定范围时,会出现髓内杆插入困难、髓内固定装置不稳、置换术后膝关节假体周围骨折以及术后疼痛等问题。股骨侧弓角又称为股骨弯曲角度,定义是在下肢股骨全长正位片中将股骨全长等分为3等分,股骨颈中线与股骨近端1/3解剖轴交点标记为A,股骨干近端1/3处的中点标记为B,A、B两点组成线段LAB,股骨干远端1/3处的中点标记为C,股骨髁间窝最高点或者股骨假体髁间最高点标记为D,C、D两点组成线段LCD,线段LAB与LCD之间的夹角为股骨侧弓的角度[12]。该角度方向也有规定,连接股骨髁间窝和股骨大转子,当该线段经过股骨干内侧,则定义为外侧弓,反之则为内侧弓[13]。也有文献报道股骨侧弓角指的是经过股骨小转子处和小转子以下5 cm处的2条水平线在股骨干的中点的连接线L1,股骨外侧髁上5 cm和10 cm处的2条水平线在股骨干中点的连接线L2,线段L1与L2之间的夹角,并规定该夹角>5°即为明显冠状位股骨侧弓[14-16]。和西方人相比,亚洲人种比如中国、日本、印度、韩国的人普遍存在着不同程度的股骨侧弓[14-21]。其中Yau等[16]报道中国终末期膝关节炎患者中普遍存在股骨侧弓,侧弓角>2°的发生率高达62%。 2.2 侧弓存在的原因 Shi等[13]认为造成股骨侧弓在亚洲人群中普遍出现的原因是维生素D和钙的营养缺乏以及种族因素;还有一种观点则是,膝关节炎导致下肢机械轴改变,膝关节出现内翻畸形,股骨为了适应内翻而做出的结构性改变,这种现象更可能是骨质疏松导致的,反过来股骨侧弓也影响着膝关节,使关节炎进一步加重[22]。 2.3 侧弓角的影响 2.3.1 侧弓角与力线 下肢力线在术后对齐是否能够影响术后功能和假体寿命仍然存在着争议[23-24],Bellemans等[25]提出了一个新的概念:“结构性膝内翻”或者“体质性膝内翻”(constitutional varus),在20-27岁年轻人群中,17%的正常女性和32%的正常男性的下肢的机械轴存在3°以上的内翻,即称之为结构性膝内翻,并且往往存在着股骨侧弓。若对这类“结构性/体质性膝内翻”的终末期膝关节炎患者经保守治疗无效后需行膝关节置换术,如果将下肢力线纠正恢复至中立位,这往往会适得其反。左右两侧下肢髋-膝-踝轴线角度存在着1°差异,那么彼此股骨侧弓角就有0.199°的差异[26]。 2.3.2 侧弓角与股骨外翻截骨角 但是下肢力线的精确重建仍然是外科医生追求的手术目标[27-28]。全膝关节置换术中精准的股骨、胫骨截骨对于术后下肢力线的重建至关重要,特别是股骨截骨。股骨远端外翻截骨角度是由股骨解剖轴与股骨机械轴(即股骨头旋转中心和膝关节中心的连线)构成的夹角,该夹角与股骨侧弓角度有很强的相关性,其中吴鹏等[9]、Kim等[19]、Lee等[29]研究发现,两者相关系数分别是0.501,0.720,0.845,不同的股骨远端外翻截骨角度组间术后下肢力线存在着明显差异。这就是说,当股骨存在侧弓时,股骨远端外翻截骨角度会受到相应的改变,那么也将影响着术后假体的精确定位以及术后下肢力线的重建。谢树峰等[30]通过对192例行膝关节置换术患者研究发现,股骨远端外翻角度与股骨侧弓角度呈正相关,与性别、颈干角、偏心距和股骨长度无关,股骨侧弓角只要增加1°,股骨远端外翻角则相应地增加0.5°,当股骨侧弓<-6°或>6°时,股骨远端截骨角度必须根据股骨远端解剖轴线来确定。股骨侧弓用肉眼观察或者膝关节正侧位X射线检查,是不能够观测到的,手术医生就有可能忽略了侧弓,造成截骨的失误,故而Chow等[31]建议术前、术后均应行双下肢全长负重位片,针对性制定术前计划和评估术后影像学指标。双下肢负重位全长片通过数字化图像的方式能够较为全面地反映关节结构、下肢力线及相关角度等参数指标,尤其对人工全膝关节置换的术前计划制定和术后评价起到重要作用[32]。国内学研究认为,拍摄下肢全长X射线片并测量下肢力线、股骨外翻角度,两者易受股骨侧弓角的影响,在行双下肢全长片检查时应采用标准体位拍照,因为测量的股骨侧弓角大小会伴随着下肢内外旋变化而变化,那么所测量的股骨远端外翻角度大小也会受到影响,当股骨的侧弓程度越大,它对股骨远端截骨产生的影响也越大者[33]。 2.4 传统全膝关节置换对伴股骨侧弓的膝关节炎处理 2.4.1 传统全膝关节置换手术步骤 传统全膝关节置换是经保守治疗无效后,对终末期膝关节炎有效的方法,步骤如下:首先就是股骨髓内定位,若术前未行双下肢标准负重站立位全长片检查,通常是采用固定的外翻截骨角度进行股骨截骨[34],或者根据术前双下肢全长片测量的结果来个体化选择外翻截骨角度[13,35]。然后是胫骨髓外定位,将定位杆远端放置于踝关节中心线(或第 1,2 跖骨中线),截骨参考点为胫骨平台相对软骨磨损不严重一侧并以此进行截骨。接下来被动活动膝关节评估下肢力线情况及关节屈伸间隙,适当地松解膝关节内外侧及后方的软组织并使屈曲间隙和伸直间隙相等。放置假体试模后观察髌骨的运动轨迹,必要时可行髌股外侧支持带松解。 2.4.2 固定外翻截骨角度截骨 为了获得下肢中立位力线,在传统全膝关节置换术中采用股骨髓内定位和胫骨髓外定位,分别垂直于股骨、胫骨机械轴行冠状面截骨。与胫骨近端截骨不同,精确地股骨远端截骨对于关节外科医生来说是一个挑战。股骨髓内定位杆在传统上采取5°或6°的外翻截骨角度来行股骨远端截骨,并认为该角度在西方人中是安全可靠的并能使力线恢复接近于中立位(3°以内误差范围)[36]。Mason等[37]对固定外翻截骨角度的研究中发现,传统组术后下肢机械轴离群值是31.8%,其中股骨假体离群值是34.1%。当术中所采用的固定外翻截骨角度小于实际外翻角时,那么时候股骨假体很容易出现内翻,进而影响术后下肢力线[38]。 2.4.3 个体化外翻截骨角度截骨 依据不同的个体测量股骨解剖轴与机械轴的夹角,选择契合个体的外翻截骨角度。股骨髓内定位易受股骨形态影响,例如股骨干畸形、骨干扭曲、股骨解剖学特征性变化,都可能进一步降低准确性[39]。患有严重股骨侧弓时,股骨外翻截骨角度变化范围大,平均大于7°,如果采用固定外翻角度截骨,那将导致下肢力线异常,进而影响假体的寿命[40-42]。 2.4.4 髓内定位系统 采用股骨髓内定位系统行股骨远端的截骨,股骨开髓点以及股骨干的解剖形态易影响到股骨假体位置安放[43-44]。开髓点位置偏差、髓内杆因解剖原因导致插入不完全或者方向偏离都会使假体的安放出现失误。开髓点位于股骨髁间窝处,当股骨外侧弓角度大于5°时,开髓点应向外移动,移动的距离以外弓角度每增加1°,则向外偏移1.04 mm,采用该方法术后下肢力线达到中立位比例是90%,而且将术前预估假体位置不良率40%降至7%[43]。Reed等[45]认为较为理想的开髓点位置应位于股骨髁中心偏内6.6 mm。髓内杆采用直径9 mm,长度为228.6 mm规格,开髓点位置与外侧皮质的距离是股骨髁宽度的0.55倍是较为理想的,还能够降低定位的误差[46]。从而得出股骨偏向外侧弓形角度较大时,术前应行双下肢负重站立位全长X射线检查,行股骨远端截骨所选角度参照全长片上测量股骨外翻角度结果,以得到较好的股骨假体位置。 2.4.5 小结 在传统膝关节置换术中,股骨、胫骨截骨是依靠股骨髓内定位和胫骨髓外定位来实现的,术中判断截骨、假体位置安放和软组织的平衡等情况主要是依靠术者手感、目测以及手术经验,手术的精确性受到这些人为的主观因素的影响,容易出现术后下肢力线不稳、假体安放位置不满意等情况,尤其是存在着严重畸形、解剖标志异常的关节置换,无法进行髓内外定位,给手术带来了极大的困难。如果在术前不考虑股骨侧弓存在,将导致股骨外翻截骨量不足,术后股骨远端出现内翻,从而导致下肢力线重建失败,使假体长期生存率受到严重影响。个性化股骨外翻截骨角度分别选用股骨机械轴与股骨远端1/3解剖轴夹角、股骨解剖轴与力线轴夹角,前者术后股骨假体冠状面位置更佳[12]。股骨侧弓角与股骨外翻角是强相关性,随着股骨侧弓角大小变化时,股骨远端截骨角度也要相应作出调整,才能保证术后下肢力线重建和假体安放,采用固定5°或6°股骨外翻角截骨,有时难免出现下肢力线不稳[47]。但是当个体化测量的外翻截骨角度超过常规截骨装置的最大值9°,那么髓内杆就不得不偏移既定的开髓点以适应截骨装置,在全膝关节置换术中插入点微小的差别也可能导致术后下肢力线不稳。 2.5 计算机导航辅助全膝关节置换的处理 2.5.1 计算机导航的工作原理 计算机红外线导航系统与全球定位系统的工作原理相似,它是将红外线示踪器固定于股骨下段及胫骨上段,通过红外线主动发射或反射方式传递下肢髋膝踝信号,计算机接收到定位器信号,通过预置图像处理,描绘出下肢整体力线情况。判断股骨及胫骨截骨是否正确则是通过使用带示踪器的截骨平面探针来探测,安装试模假体后进行膝关节伸屈活动,通过计算机屏幕显示的图像以及数值,观察其中运动学参数变化,并以此为依据客观地进行软组织的松解或通过调整衬垫的厚度来获得良好的软组织平衡。最后在计算机导航确认下置入假体。手术过程中通过导航系统的红外线摄像头,术者能够动态追踪手术器械相对于患者解剖结构的实时空间位置关系。术者通过计算机的显示屏可以从各个方位观察操作过程和位置变化,每一步操作结果均以客观的数字反映。 2.5.2 计算机导航的应用 从已检索的文献中筛选出7篇关于计算机导航与传统方法对伴有股骨侧弓的膝关节置换疗效的研究,并总结相关评价指标见表1。 "
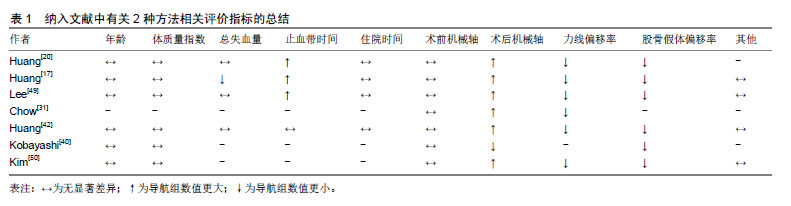

(1)年龄与体质量指数:6个研究通过比较术前患者年龄与体质量指数后[17,20,40,42,49-50],均一致得出这2项资料差异均无显著性意义。 (2)总失血量:共有4个研究对2种方法总失血量进行了比较分析,其中Huang等[17]得出结论,计算机导航组总失血量(497±201)mL,传统组(621±291)mL,2组间差异有显著性意义(P=0.048);其余3项研究对2组总失血量进行比较[20,42,49],均提示差异无显著性意义,但是导航组平均失血量少于传统组。 (3)止血带时间:4项研究比较了2组止血带使用时间,除了Huang等[42]认为导航组(111 min)、传统组(109 min),差异无显著性意义(P=0.532),其余研究均提示差异有显著性意义(P < 0.05)[17,20,49]。从上述研究中还可得知,导航组止血带使用时间平均长于传统组。 (4)住院时间:4个研究对2组的住院时间比 较[17、20、42、49],均提示差异无显著性意义。 (5)术前/术后机械轴:7项研究对比2组术前机械轴,均提示差异无显著性意义;但是在术后机械轴比较中,差异均有显著性意义,除了Kobayashi等[40]研究发现,导航组术后髋-膝-踝角为-1.2°,传统组为1.0°,差异有显著性意义(P=0.035),提示导航组在重建下肢力线中立位方面,略微不如传统组,其他研究均提示对比传统方法,计算机导航在重建下肢力线方面更有优势[17,20,31,42,49-50]。 (6)下肢力线偏移率:对比2组术后下肢力线偏移率,6个研究结果均提示差异有显著性意义(P < 0.05)[17,20,31,42,49-50],其中Lee等[49]研究发现,下肢机械轴偏移大于3°在导航组中发生率为3.7%,传统组高达50.8%,导航组更具有优势。 (7)股骨假体偏移率:对比2组术后股骨假体偏移>3°,6项研究结果均提示差异有显著性意义[17,20,40,42,49-50],且一致认为导航在股骨假体位置准确安放上更具有优势。 (8)其他:比较2组美国纽约特种外科医院评分、美国膝关节协会评分、西安大略和麦克马斯特大学骨关节炎指数以及膝关节活动度,均提示2组之间差异并无显著性意义(P > 0.05)[17,42,49-50]。 2.5.3 小结 计算机导航辅助技术通过特定的解剖标志点,将下肢整体的力线情况反映在计算机上,这样术者可以实时的观察到自己进行的每一个操作的准确位置以及所产生的结果。在导航辅助下全膝关节置换中,股骨和胫骨的截骨是基于在导航系统中注册相关部位的解剖标志,而不是依靠传统髓内或髓外定位系统。通过对15篇关于计算机导航与传统膝关节置换术的随机对照试验的Meta分析,在术中假体安放的精准度、术后膝关节活动度两方面导航组要优于传统组;在手术时间上,传统组更具有优势;比较术中出血量以及术后并发症发生率2组差异并无显著性意义[48]。此文从已检索文献中归纳总结2种方法的相关评价指标可以得知,股骨侧弓骨关节炎行全膝关节置换术,相比传统方法,计算机导航辅助在术后下肢力线、假体位置安放上更具有优势;术前基线资料年龄、体质量指数差异并无显著性意义,在总失血量上,仅有1篇发现导航组比传统组更少;导航组使用止血带时间更长;2组住院时间差异也并无显著性意义。 "

| [1]Rönn K, Reischl N , Gautier E, et al. Current surgical treatment of knee osteoarthritis. Arthritis. 2011;(5):45-48.[2]Cobb JP. Patient safety after partial and total knee replacement. Lancet. 2014;384(9960):1405-1407.[3]Kim HJ, Lee HJ, Shin JY, et al. Preoperative planning using the picture archiving and communication system technique in high tibial osteotomy. J Orthop Surg. 2017;25(1):1-6.[4]李健.计算机导航技术在全膝关节置换中对下肢力线重建的作用[J]. 医学综述, 2011, 17(20):3108-3110.[5]孙振辉,孙云波,曹建刚,等.人工全膝关节置换术后伤口并发症的原因分析和临床处理[J].中国修复重建外科杂志, 2009,23(6):644-647.[6]Wilson DA, Corkum JP, Teeter MG, et al. Early Failure of a Polyethylene Acetabular Liner Cemented Into a Metal Cup. J Arthroplasty. 2012; 27(5):820. e5-e8.[7]Gharaibeh MA, Solayar GN, Harris IA, et al. Accelerometer-based, portable navigation (kneealign) vs conventional instrumentation for total knee arthroplasty: a prospective randomized comparative trial. J Arthroplasty. 2016; 32(3):777-782.[8]谢军,刘巍,袁凤来.股骨假体旋转角对全膝关节置换后膝关节功能恢复影响的3年随访[J].中国组织工程研究,2017,21(27):4283-4287.[9]吴鹏,郎俊哲,刘扬波,等.全膝关节置换术股骨远端外翻角影响因素探讨[J]. 温州医科大学学报, 2016, 46(12):878-882.[10]黄宁,魏杰,秦德安. 股骨前弓角的临床意义[J]. 实用骨科杂志, 2014, 20(3): 237-239.[11]Tang WM, Chiu KY, Kwan MF, et al. Sagittal bowing of the distal femur in Chinese patients who require total knee arthroplasty. J Orthop Res. 2005; 23(1):41-45.[12]吴博,王岩,张国强,等.两种股骨截骨角度对膝关节置换术中股骨假体冠状位对线的影响[J].中国矫形外科杂志, 2017, 25(9):838-843.[13]Shi X, Li H, Zhou Z, et al. Comparison of postoperative alignment using fixed vs individual valgus correction angle in primary total knee arthroplasty with lateral bowing femur. J Arthroplasty. 2016;31(5): 976-983.[14]Mullaji AB, Marawar SV, Mittal V. A comparison of coronal plane axial femoral relationships in asian patients with varus osteoarthritic knees and healthy knees. J Arthroplasty. 2009; 24(6):861-867.[15]Mullaji A, Shetty GM. Computer-assisted total knee arthroplasty for arthritis with extra-articular deformity. J Arthroplasty. 2009; 24(8): 1164-1169.[16]Yau WP, Chiu KY, Tang WM, et al. Coronal bowing of the femur and tibia in Chinese: its incidence and effects on total knee arthroplasty planning. J Orthop Surg. 2007;15(1):32-36.[17]Huang TW, Peng KT, Huang KC, et al. Differences in component and limb alignment between computer-assisted and conventional surgery total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014; 22(12):2954-2961.[18]Lasam MP, Lee KJ, Chang CB, et al. Femoral lateral bowing and varus condylar orientation are prevalent and affect axial alignment of TKA in Koreans. Clin Orthop Relat Res. 2013;471(5):1472-1483.[19]Kim JM, Hong SH, Kim JM, et al. Femoral shaft bowing in the coronal plane has more significant effect on the coronal alignment of TKA than proximal or distal variations of femoral shape. Knee Surg Sports Traumatol Arthrosc. 2014; 23(7):1936-1942.[20]Huang TW, Hsu WH, Peng KT, et al. Total knee replacement in patients with significant femoral bowing in the coronal plane: a comparison of conventional and computer-assisted surgery in an Asian population. J Bone Joint Surg Br. 2011;93(3):345-350.[21]Abdelaal AH, Yamamoto N, Hayashi K, et al. Radiological assessment of the femoral bowing in Japanese population. SICOT J. 2016; 2:1-7.[22]Mochizuki T , Tanifuji O , Koga Y , et al. Sex differences in femoral deformity determined using three-dimensional assessment for osteoarthritic knees. Knee Surg Sports Traumatol Arthrosc. 2017; 25(2): 468-476.[23]Magnussen RA , Weppe F , Demey G , et al. Residual varus alignment does not compromise results of tkas in patients with preoperative varus. Clin Orthop Relat Res. 2011;469(12):3443-3450.[24]Gothesen O, Espehaug B , Havelin LI , et al. Functional outcome and alignment in computer-assisted and conventionally operated total knee replacements: a multicentre parallel-group randomised controlled trial. Bone Joint J. 2014; 96-B(5):609-618.[25]Bellemans J, Colyn W, Vandenneucker H, et al. The chitranjan ranawat award: is neutral mechanical alignment normal for all patients? the concept of constitutional varus. Clin Orthop Relat Res. 2012;470(1): 45-53.[26]Cho MR , Lee YS , Choi WK. Relationship between lateral femoral bowing and varus knee deformity based on two-dimensional assessment of side-to-side differences. Knee Surg Relat Res. 2018; 30(1):58-63.[27]Abdel MP, Oussedik S, Parratte S, et al. Coronal alignment in total knee replacement. Bone Joint J. 2014; 96-B(7):857-862.[28]Liow MH, Goh GS, Pang HN, et al. Computer-assisted stereotaxic navigation improves the accuracy of mechanical alignment and component positioning in total knee arthroplasty. Arch Orthop Trauma Surg. 2016; 136(8):1173-1180.[29]Lee CY, Huang TW, Peng KT, et al. Variability of distal femoral valgus resection angle in patients with end-stage osteoarthritis and genu varum deformity: radiographic study in an ethnic asian population. Biomed J. 2015;38(4):350-355.[30]谢树峰,柳庆坤,刘晓松,等. 全膝关节置换术中股骨远端外翻截骨角与股骨形态的相关性研究[J]. 西北国防医学杂志, 2018,39(4):224-228.[31]Chow MYM, Tsang WL, Wong MK, et al. Comparison of postoperative alignment of total knee replacement using computer-assisted navigation with conventional guiding system in chinese population with significant coronal femoral bowing. J Orthop Trauma Rehabil. 2015; 19(1):21-24.[32]Tanaka T, Takayama K, Hashimoto S, et al. Radiographic analysis of the lower limbs using the hip-calcaneus line in healthy individuals and in patients with varus knee osteoarthritis. Knee. 2017;24(5):1146-1152.[33]吴伟,郭万首,李传东,等. CT三维重建分析不同体位下股骨侧弓对下肢力线测量的影响[J]. 中国组织工程研究, 2017, 21(11):1764-1769.[34]Nam D, Vajapey S, Haynes JA, et al. Does use of a variable distal femur resection angle improve radiographic alignment in primary total knee arthroplasty? J Arthroplasty. 2016;31(9):91-96.[35]Bardakos N, Cil A, Thompson B, et al. Mechanical axis cannot be restored in total knee arthroplasty with a fixed valgus resection angle: a radiographic study. J Arthroplasty. 2007;22(6 Suppl 2): 85-89.[36]Kharwadkar N, Kent RE, Sharara KH, et al. 5 degrees to 6 degrees of distal femoral cut for uncomplicated primary total knee arthroplasty: is it safe? Knee. 2006;13(1):57-60.[37]Mason JB, Fehring TK, Estok R, et al. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 2007; 22(8):1097-1106.[38]马路遥,郭万首,马金辉,等.全膝关节置换术中固定角度外翻截骨会影响置换后下肢力线吗[J].中国组织工程研究, 2017, 21(11):1658-1663.[39]Ko PS , Tio MK , Ban CM , et al. Radiologic analysis of the tibial intramedullary canal in Chinese varus knees. J Arthroplasty. 2001; 16(2): 212-215.[40]Kobayashi H, Akamatsu Y, Kumagai K, et al. Influence of coronal bowing on the lower alignment and the positioning of component in navigation and conventional total knee arthroplasty. Orthop Traumatol Surg Res. 2017;103(2):251-256.[41]Huang TW, Lee CY, Lin SJ, et al. The influence of alignment on midterm outcome after total knee arthroplasty in patients with marked coronal femoral bowing. J Arthroplasty. 2015;30(9):1531-1536.[42]Huang TW , Chuang PY , Lee CY , et al. Total knee arthroplasty in patients with Ranawat type-II valgus arthritic knee with a marked coronal femoral bowing deformity: comparison between computer-assisted surgery and intra-articular resection. J Orthop Surg Res. 2016;11(1):88.[43]Thippanna RK, Kumar MN. Lateralization of femoral entry point to improve the coronal alignment during total knee arthroplasty in patients with bowed femur. J Arthroplasty. 2016; 31(9):1943-1948.[44]Mullaji AB, Shetty GM, Kanna R, et al. The influence of preoperative deformity on valgus correction angle: an analysis of 503 total knee arthroplasties. J Arthroplasty. 2013; 28(1):20-27.[45]Reed SC, Gollish J. The accuracy of femoral intramedullary guides in total knee arthroplasty. J Arthroplasty. 1997;12(6):677-682.[46]Novotny J, Gonzalez MH, Amirouche FM, et al. Geometric analysis of potential error in using femoral intramedullary guides in total knee arthroplasty. J Arthroplasty. 2001;16(5):641-647.[47]吴伟,郭万首,程立明,等.股骨侧弓角的个体差异对全膝人工关节置换术后下肢力线的影响[J].中华医学杂志, 2017,97(13):1006-1010.[48]王康,石一璠,赵昱,等.计算机导航与传统人工全膝关节置换临床疗效的Meta分析[J].中华关节外科杂志(电子版), 2018,12(2):222-230.[49]Lee CY, Lin SJ, Kuo LT, et al. The benefits of computer-assisted total knee arthroplasty on coronal alignment with marked femoral bowing in Asian patients. J Orthop Surg Res. 2014;9(1):122.[50]Kim CW, Lee CR. Effects of femoral lateral bowing on coronal alignment and component position after total knee arthroplasty: a comparison of conventional and navigation-assisted surgery. Knee Surg Relat Res. 2018;30(1):64-73.[51]Roberts TD, Clatworthy MG, Frampton CM, et al. Does computer assisted navigation improve functional outcomes and implant survivability after total knee arthroplasty. J Arthroplasty. 2015;30(9 Suppl): 59-63. |
| [1] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [2] | Zhao Zhongyi, Li Yongzhen, Chen Feng, Ji Aiyu. Comparison of total knee arthroplasty and unicompartmental knee arthroplasty in treatment of traumatic osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 854-859. |
| [3] | Yuan Jun, Yang Jiafu. Hemostatic effect of topical tranexamic acid infiltration in cementless total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 873-877. |
| [4] | Cao Xuhan, Bai Zixing, Sun Chengyi, Yang Yanjun, Sun Weidong. Mechanism of “Ruxiang-Moyao” herbal pair in the treatment of knee osteoarthritis based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 746-753. |
| [5] | Li Yonghua, Feng Qiang, Tan Renting, Huang Shifu, Qiu Jinlong, Yin Heng. Molecular mechanism of Eucommia ulmoides active ingredients treating synovitis of knee osteoarthritis: an analysis based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 765-771. |
| [6] | Qian Xuankun, Huang Hefei, Wu Chengcong, Liu Keting, Ou Hua, Zhang Jinpeng, Ren Jing, Wan Jianshan. Computer-assisted navigation combined with minimally invasive transforaminal lumbar interbody fusion for lumbar spondylolisthesis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3790-3795. |
| [7] | Yang Wei, Chen Zehua, Yi Zhiyong, Huang Xudong, Han Qingmin, Zhang Ronghua. Effectiveness of intra-articular injection of hyaluronic acid versus placebo in the treatment of early and mid-stage knee osteoarthritis: a Meta-analysis based on randomized, double-blind, controlled, clinical trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(23): 3760-3766. |
| [8] | Mieralimu•Muertizha, Ainiwaerjiang•Damaola, Lin Haishan, Wang Li . Relationship between tibio-femoral mechanical axis deviation on coronal plane and early joint function recovery after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3300-3304. |
| [9] | Zheng Kai, Li Rongqun, Sun Houyi, Zhang Weicheng, Li Ning, Zhou Jun, Zhu Feng, Wang Yijun, Xu Yaozeng. Computer-navigated versus conventional one-stage bilateral total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3305-3312. |
| [10] | Deng Zhibo, Li Zhi, Wu Yahong, Mu Yuan, Mu Yuexi, Yin Liangjun. Local infiltration anesthesia versus femoral nerve block for pain control and safety after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3401-3408. |
| [11] | Zuo Xiuqin, Yin Sasa, Xie Huimin, Jia Zishan, Zhang Lining. Applicability and specifications of platelet-rich plasma in musculoskeletal repair [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(20): 3239-3245. |
| [12] | Huang Chenyu, Tang Cheng, Wei Bo, Li Jiayi, Li Xuxiang, Zhang Huikang, Xu Yan, Yao Qingqiang, Wang Liming. Application of three-dimensional printing guide plate in total knee arthroplasty for patients with varus and valgus deformity [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2789-2793. |
| [13] | Li Shangzhi, Zheng Dezhi, Liu Jun. Early analgesia of cocktail therapy after total knee arthroplasty with enhanced recovery after surgery program [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2794-2798. |
| [14] | Liu Jinlei, Yin Li, Zhang Yi, Wang Haitao, Li Zhuangyan, Xia Peige, Qiao Renqiu. Effects of intravenous tranexamic acid combined with periarticular multipoint injection of tranexamic acid cocktail on blood loss and pain after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2833-2839. |
| [15] | Xu Hui, Kang Bingxin, Gao Chenxin, Zhao Chi, Xu Xirui, Sun Songtao, Xie Jun, Xiao Lianbo, Shi Qi. Effectiveness of Tuina in the treatment of pain after total knee arthroplasty in patients with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2840-2845. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||