Chinese Journal of Tissue Engineering Research ›› 2019, Vol. 23 ›› Issue (8): 1265-1274.doi: 10.3969/j.issn.2095-4344.1050
Previous Articles Next Articles
The influence of different limb positions on clinical outcomes after primary total knee arthroplasty: a meta-analysis of randomized controlled trials
Wang Haiyang1, Lin Yanbin1, Yu Guangshu1, Li Jiehui2, Zhang Shouxiong2, Liu Youying2, Xu Hongbin2
- 1Department of Orthopedics, Fuzhou Second Hospital Affiliated to Xiamen University, Fuzhou 350007, Fujian Province, China; 2Graduate School of Fujian University of Traditional Chinese Medicine, Fuzhou 350122, Fujian Province, China
-
Online:2019-03-18Published:2019-03-18 -
Contact:Lin Yanbin, Chief physician, Professor, Master’s supervisor, Department of Orthopedics, Fuzhou Second Hospital Affiliated to Xiamen University, Fuzhou 350007, Fujian Province, China -
About author:Wang Haiyang, Master candidate, Department of Orthopedics, Fuzhou Second Hospital Affiliated to Xiamen University, Fuzhou 350007, Fujian Province, China -
Supported by:the Young Talent Training Project in Health System of Fujian Province, No. 2014-ZQN-JC-34 (to LYB)
CLC Number:
Cite this article
Wang Haiyang, Lin Yanbin, Yu Guangshu, Li Jiehui, Zhang Shouxiong, Liu Youying, Xu Hongbin. The influence of different limb positions on clinical outcomes after primary total knee arthroplasty: a meta-analysis of randomized controlled trials[J]. Chinese Journal of Tissue Engineering Research, 2019, 23(8): 1265-1274.
share this article

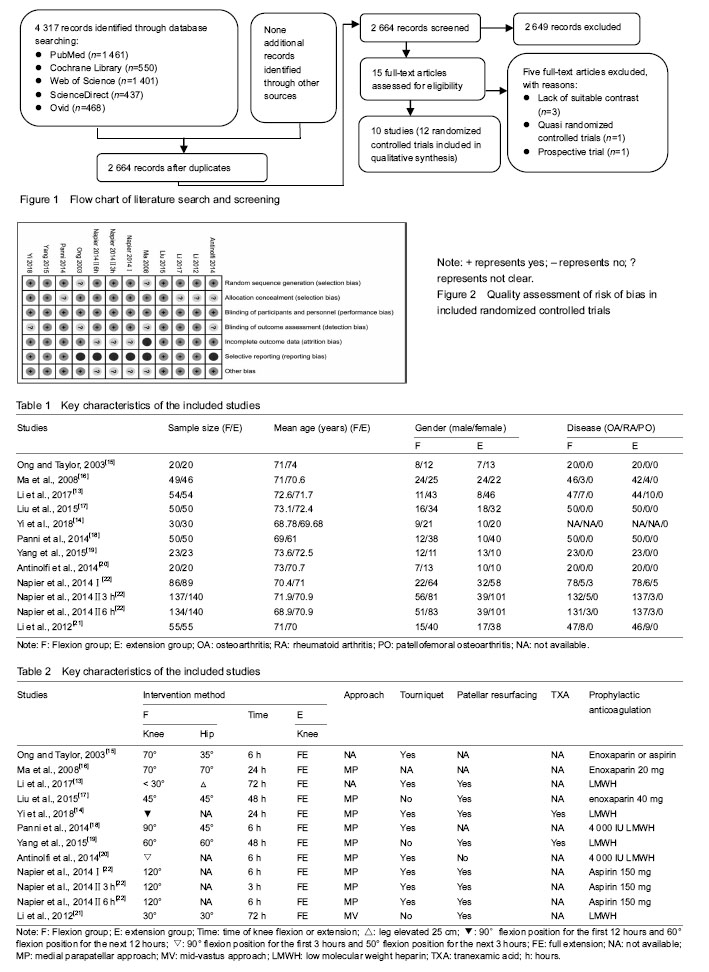
Study selection and characteristics of the included studies A total of 4 317 relevant studies were initially identified. After duplicate studies were removed, 2 664 studies were available for assessing titles and abstracts for eligibility. Of these, 15 articles were then evaluated for full-text articles. We eventually identified 10 articles[13-22] meeting the Inclusive criteria (Figure 1). Among these, the article by Napier et al.[22] had two RCTs and the second RCT had multiple comparisons. All selected studies were in English and were published between 2003 and 2018. Five studies[13-14, 17, 19, 21] were performed in China, two[15, 22] in UK, two[18,20] in Italy, and one[16] in Australia. The key characteristics of these studies are illustrated in Table 1, while study treatment protocol of the included study is shown in Table 2. Quality assessment The methodological quality of all the included RCTs was assessed based on the Cochrane Collaboration recommendations. Although all included RCTs declared randomization, only 10 RCTs mentioned the adequate randomization technique including a random number list[13, 17-21] and a sealed random number envelope[14, 22]. Allocation concealment was mentioned in six trials[14-17, 19, 22] and unclear in four trials[13, 18, 20-21]. Outcome assessors were blinded in six trials[13, 17-19, 21-22], but the blinding in the other four trials was unclear[14-16, 20]. The detailed risk of bias of methodological quality in the eligible RCTs is summarized in Figure 2."

Outcomes of meta-analysis Total blood loss Total blood loss was mentioned in 8 studies[13-14, 17-22], including 1 115 patients (553 patients were in the flexion group and 562 patients in the extension group). Because of the high heterogeneity (P < 0.000 01, I²=88%), a random-effect model was used to pool the data. In pooled analyses, compared with the extension group, there was a significant reduction in the total blood loss in the flexion group (MD=-163.39; 95%CI, -232.74 to -94.04; P < 0.000 01; Figure 3). The subgroup analysis of total blood loss did not emerge any significant differences within all subgroups (Table 3). Hidden blood loss Five studies[13, 17-19, 21] with a total of 464 patients reported the outcome of hidden blood loss. Significant heterogeneity was found, so a random-model was adopted (P < 0.000 01, I²=96%). Pooling results demonstrated that there was an outstanding reduction in the hidden blood loss between flexion and extension groups (MD=-95.24; 95%CI, -153.64 to -36.84; P=0.001; Figure 4). In the subgroup analysis of hidden blood loss, there was no significant difference with subgroups based on the time of knee flexion. Subgroup analysis revealed significant reductions in hidden blood loss when the knee was fixed in the ≤ 60° of knee flexion (MD=-64.70; 95%CI, -121.20 to -8.21; P=0.02) compared with the > 60° of knee flexion (MD=-143.10; 95%CI, -310.68 to 24.47; P=0.09) (Table 3). Blood transfusion requirement Seven studies[13-19] with a total of 549 patients provided the data of blood transfusion requirement. Discovered no significant heterogeneity, a fixed-model was applied (P=0.59, I²=0%). The meta-analysis unmasked that there was a remarkable reduction in the blood transfusion requirement between flexion and extension groups (RR=-0.07; 95%CI, -0.13 to -0.02; P=0.010; Figure 5). The subgroup analysis revealed that blood transfusion requirement can markedly reduce when the knee was fixed in the > 60° of knee flexion (RR=-0.10; 95%CI, -0.17 to -0.03; P=0.007) in comparison with the ≤ 60° of knee flexion subgroup (RR=-0.04; 95%CI, -0.13 to 0.06; P=0.43). It could dramatically diminish when the knee was fixed for 24 hours (RR=-0.09; 95%CI, -0.17 to -0.02; P=0.002) compared with >24 hours (RR=-0.06; 95%CI, -0.14 to 0.03; P=0.21) (Table 3). Range of motion Data from 7 studies[13-14, 16-19, 21] including 883 patients were available for range of motion. Among seven studies, three studies[13, 19, 21] provided the multiple data of range of motion at 7 days, 6 weeks and 6 months postoperatively, which were also involved in pooled analyses. There was remarkable heterogeneity among studies (P=0.006, I²=61%); therefore, a random-model was performed. In pooled analyses, compared with the extension group, there was a significant improvement of range of motion in the flexion group (MD=3.50; 95%CI, 1.31 to 5.69; P=0.002; Figure 6). The subgroup analysis uncovered that range of motion can dramatically improve when the knee was fixed in the ≤ 60° of knee flexion (MD=3.84; 95%CI, 0.86 to 6.82; P=0.01) compared with the > 60° of knee flexion (MD=3.10; 95%CI, -0.28 to 6.48; P=0.07); that it can significantly increase when the knee was fixed for > 24 hours (MD=3.85; 95%CI, 1.88 to 5.82; P=0.000 1) in comparison with ≤ 24 hours (MD=2.21; 95%CI, -3.69 to 8.11; P=0.46); that it could markedly improve at 1 week postoperatively (MD=6.94; 95%CI, 5.06 to 8.81; P=0.000). On the contrary, similar results did not appear at 6 or more than 6 weeks postoperatively (MD=1.89; 95%CI, -0.05 to 3.82; P=0.06) (Table 3)."
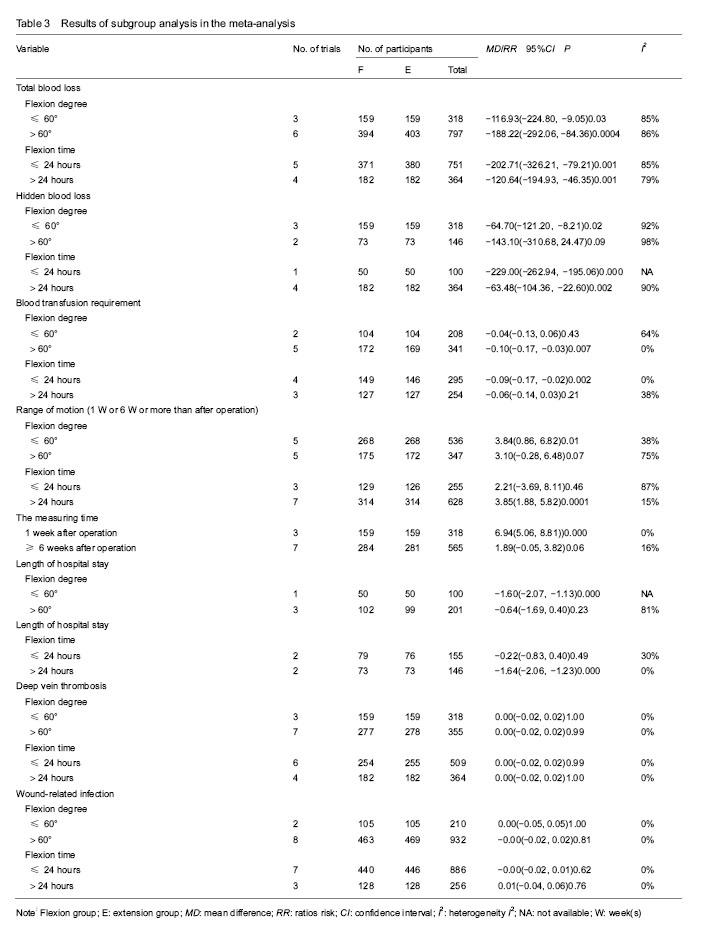

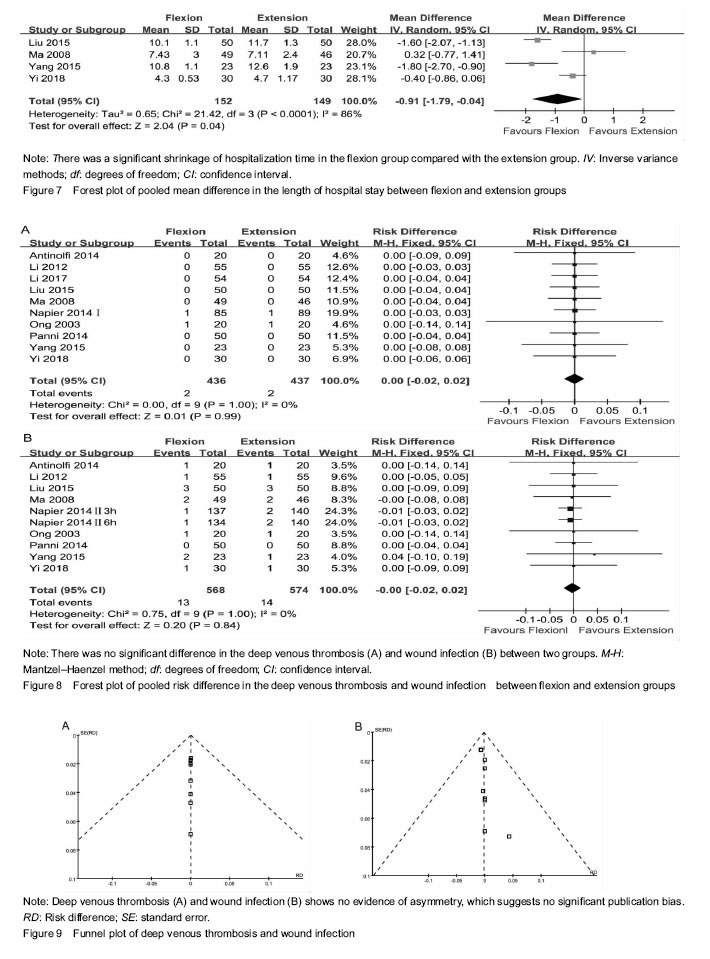
Hospitalization time The hospitalization time was mentioned in 4 studies[14, 16-17, 19], including 301 patients (152 patients were in the flexion group and 149 patients in the extension group). Because of the high heterogeneity (P < 0.000 1, I²=86%), a random-effect model was adopted to pool the data. The meta-analysis uncovered that there was a significant shrinkage of hospitalization time in the flexion group compared with the extension group (MD=-0.91; 95%CI, -1.79 to -0.04; P=0.04; Figure 7). The subgroup analysis unmasked that length of hospitalization time could significantly shorten when the knee was fixed in the ≤ 60° of knee flexion (MD=-1.60; 95%CI, -2.07 to -1.13; P=0.000) compared with the > 60° of knee flexion (MD=-0.64; 95%CI, -1.69 to 0.40; P=0.23); that it can dramatically diminish when the knee was fixed for > 24 hours (MD=-1.64; 95%CI, -2.06 to -1.23; P=0.000) in comparison with the knee fixed time of > 24 hours (MD=-0.22; 95%CI, -0.83 to 0.40; P=0.49) (Table 3). Deep venous thrombosis Data from 10 studies [13-22] including 873 patients was available for deep venous thrombosis. There was no heterogeneity among studies (P=1.00, I²=0%); hence, a fixed-model was adopted. In pooled analyses, there was no significant between-group difference in the deep venous thrombosis (RR=0.00; 95%CI, -0.02 to 0.02; P=0.99; Figure 8A). The subgroup analysis of deep venous thrombosis did not emerge any significant differences among subgroups (Table 3). Wound infection Nine studies[14-22] with a total of 1 142 patients provided the data of wound infection. Detected no significant heterogeneity, a fixed-model was adopted (P=1.00, I²=0%). The meta-analysis unmasked that there was no significant difference in wound infection between flexion and extension groups (RR=-0.00; 95%CI, -0.02 to 0.02; P=0.84; Figure 8B). In the subgroup analysis of wound infection, there was no significant difference among subgroups (Table 3). Publication bias Two funnel plots respectively based on deep venous thrombosis and wound infection were used to assess publication bias. Both figures demonstrated only minimal asymmetry and a few outliers, indicating minimal evidence of publication bias (Figure 9)."
| [1] Lei Y, Xie J, Xu B, et al. The efficacy and safety of multiple-dose intravenous tranexamic acid on blood loss following total knee arthroplasty: a randomized controlled trial. Int Orthop. 2017;41(10):2053-2059. [2] Wu YG, Zeng Y, Yang TM, et al. The efficacy and safety of combination of intravenous and topical tranexamic acid in revision hip arthroplasty: a randomized, controlled trial. J Arthroplasty. 2016;31(11):2548-2553.[3] Yi Z, Bin S, Jing Y, et al. Tranexamic acid administration in primary total hip arthroplasty: a randomized controlled trial of intravenous combined with topical versus single-Dose Intravenous Administration. J Bone Joint Surg Am. 2016; 98(12):983-991. [4] Loftus TJ, Spratling L, Stone BA, et al. A patient blood management program in prosthetic joint arthroplasty decreases blood use and improves outcomes. J Arthroplasty. 2016;31(1):11-14. [5] Ponnusamy KE, Kim TJ, Khanuja HS. Perioperative blood transfusions in orthopaedic surgery. J Bone Joint Surg Am. 2014;96(21):1836-1844. [6] Lee SY, Chong S, Balasubramanian D, et al. What is the ideal route of administration of tranexamic acid in TKA? a randomized controlled trial. Clin Orthop Relat Res. 2017; 475(8):1987-1996.[7] Fu X, Tian P, Li ZJ, et al. Postoperative leg position following total knee arthroplasty influences blood loss and range of motion: a meta-analysis of randomized controlled trials. Curr Med Res Opin. 2016;32(4):771-778. [8] Wu Y, Yang T, Zeng Y, et al. Effect of different postoperative limb positions on blood loss and range of motion in total knee arthroplasty: An updated meta-analysis of randomized controlled trials. Int J Surg. 2017;37:15-23. [9] Faldini C, Traina F, De Fine M, et al. Post-operative limb position can influence blood loss and range of motion after total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):852-859. [10] De Fine M, Traina F, Giavaresi G, et al. Effect of different postoperative flexion regimes on the outcomes of total knee arthroplasty: randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2972-2977.[11] Jiang C, Lou J, Qian W, et al. Impact of flexion versus extension of knee position on outcomes after total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg. 2017;137(2):257-265. [12] Fu X, Tian P, Li ZJ, et al. Postoperative leg position following total knee arthroplasty influences blood loss and range of motion: a meta-analysis of randomized controlled trials. Curr Med Res Opin. 2016;32(4):771-778. [13] Li B, Wang G, Wang Y, et al. Effect of two limb positions on venous hemodynamics and hidden blood loss following total knee arthroplasty. J Knee Surg. 2017;30(1):70-74. [14] Zeng Y, Si H, Li C, et al. Effect of knee flexion position and combined application of tranexamic acid on blood loss following primary total knee arthroplasty: a prospective randomized controlled trial. Int Orthop. 2018;42(3):529-535. [15] Ong SM, Taylor GJ. Can knee position save blood following total knee replacement? Knee. 2003;10(1):81-85.[16] Ma T, Khan RJ, Carey Smith R, et al. Effect of flexion/extension splintage post total knee arthroplasty on blood loss and range of motion -- a randomised controlled trial. Knee. 2008;15(1):15-19. [17] Liu J, Li YM, Cao JG, et al. Effects of knee position on blood loss following total knee arthroplasty: a randomized, controlled study. J Orthop Surg Res. 2015;10:69. [18] Panni AS, Cerciello S, Vasso M, et al. Knee flexion after total knee arthroplasty reduces blood loss. Knee Surg Sports Traumatol Arthrosc. 2014;22(8):1859-1864.[19] Yang Y, Yong-Ming L, Pei-jian D, et al. Leg position influences early blood loss and functional recovery following total knee arthroplasty: A randomized study. Int J Surg. 2015;23(Pt A):82-86.[20] Antinolfi P, Innocenti B, Caraffa A, et al. Post-operative blood loss in total knee arthroplasty: knee flexion versus pharmacological techniques. Knee Surg Sports Traumatol Arthrosc. 2014;22(11):2756-2762.[21] Li B, Wen Y, Liu D, et al. The effect of knee position on blood loss and range of motion following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012; 20(3):594-599. [22] Napier RJ, Bennett D, McConway J, et al. The influence of immediate knee flexion on blood loss and other parameters following total knee replacement. Bone Joint J. 2014; 96-B (2): 201-209. [23] Madarevic T, Tudor A, Sestan B, et al. Postoperative blood loss management in total knee arthroplasty: a comparison of four different methods. Knee Surg Sports Traumatol Arthrosc. 2011;19(6):955-959. [24] Zenios M, Wykes P, Johnson DS, et al. The use of knee splints after total knee replacements. Knee. 2002;9(3): 225-228.[25] Horton TC, Jackson R, Mohan N, et al. Is routine splintage following primary total knee replacement necessary? A prospective randomised trial. Knee. 2002;9(3):229-231. |
| [1] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [2] | Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470. |
| [3] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [4] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [5] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [6] | Li Dadi, Zhu Liang, Zheng Li, Zhao Fengchao. Correlation of total knee arthroplasty efficacy with satisfaction and personality characteristics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1346-1350. |
| [7] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [8] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [9] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [10] | Peng Zhihao, Feng Zongquan, Zou Yonggen, Niu Guoqing, Wu Feng. Relationship of lower limb force line and the progression of lateral compartment arthritis after unicompartmental knee arthroplasty with mobile bearing [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1368-1374. |
| [11] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [12] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [13] | Yuan Jiawei, Zhang Haitao, Jie Ke, Cao Houran, Zeng Yirong. Underlying targets and mechanism of Taohong Siwu Decoction in prosthetic joint infection on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1428-1433. |
| [14] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [15] | Wang Yongsheng, Wu Yang, Li Yanchun. Effect of acute high-intensity exercise on appetite hormones in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1305-1312. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||

