Chinese Journal of Tissue Engineering Research
Previous Articles Next Articles
Characteristics of total hip arthroplasty in patients with end stage renal disease
Zhuang Ze, Li Zhi-yong, Chen Yu-xian, Ren Jian-hua, He Rong-han, Zhao Jia-yao, Wang Kun
- Department of Joint and Traumatic Orthopedics, the Third Affiliated Hospital of Sun Yat-sen University, Guangzhou 510630, Guangdong Province, China
-
Received:2012-11-29Revised:2013-02-16Online:2013-06-25Published:2013-06-25 -
Contact:Wang Kun, M.D., Chief physician, Department of Joint and Taumatic Orthopedics, the Third Affiliated Hospital of Sun Yat-sen University, Guangzhou 510630, Guangdong Province, China dr.wangkun333@yahoo.com.cn -
About author:Zhuang Ze, Department of Joint and Taumatic Orthopedics, the Third Affiliated Hospital of Sun Yat-sen University, Guangzhou 510630, Guangdong Province, China zzbjm@163.com
CLC Number:
Cite this article
Zhuang Ze, Li Zhi-yong, Chen Yu-xian, Ren Jian-hua, He Rong-han, Zhao Jia-yao, Wang Kun. Characteristics of total hip arthroplasty in patients with end stage renal disease[J]. Chinese Journal of Tissue Engineering Research, doi: 10.3969/j.issn.2095-4344.2013.26.002.
share this article
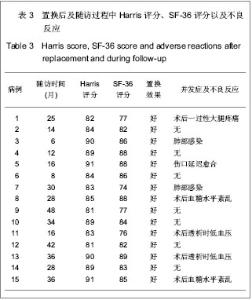
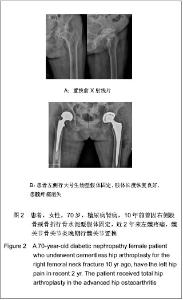
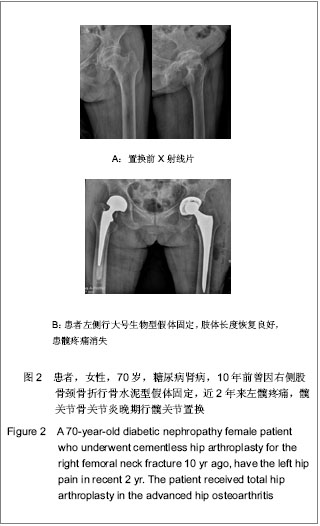
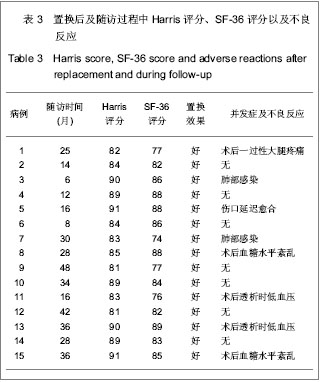
2.3 置换后髋关节活动度 屈曲平均110°,过伸平均10°,内旋平均35°,外旋平均30°,外展平均30°,内收平均20°。 2.4 置换后并发症发生情况 出院前出现5例并发症,2例置换后透析时出现低血压休克,2例肺部感染,1例伤口延迟愈合,经治疗后均恢复。 2.5 置换后随访评分 置换后随访时间为0.5-4年,呈偏态分布,中位数时间为30个月,Harris髋关节功能评分由置换前的(53.0±5.8)分增加至末次随访的(86.0±3.8)分。SF-36评分由置换前的(65.0±2.4)分增加至末次随访的(83.0±4.9)分。 2.6 置换后的不良事件 没有和手术相关的严重并发症,如肺栓塞、下肢深静脉血栓和假体松动等。置换后随访未见假体松动、脱位、假体感染等假体相关并发症。部分糖尿病肾病患者置换后血糖水平紊乱,伤口愈合延迟。围手术期间有2例患者出现肺部感染,予抗感染后痊愈,见表3。"
| [1] Dong HY. Yingguo Yixue Zazhi:Zhongwenban. 2006;9(3):136.董海燕.译后评沦:我囯慢性肾脏病的新数据及其警示[J].英囯医学杂志:中文版,2006,9(3):136.[2] Chinese Society of Blood Purification Administration. Zhongguo Xueye Jinghua. 2010;9(1):47-49.中国医院协会血液净化中心管理分会血液透析登记组.我国面临快速增长的终末期肾病治疗负担[J].中国血液净化,2010,9(1): 47-49.[3] Tang S,Gong ZF,Peng XM,et al. Zhongguo Laonianxue Zazhi. 2009;29(5): 613-614.唐盛,龚智峰,彭小梅,等.老年终末期肾病患者流行病学调查分析[J].中国老年学杂志,2009,29(5): 613-614.[4] Zhang LX,Wang M,Wang HY. Zhonghua Shenzhangbing Zazhi. 2005; 21(7):425-428.张路霞,王梅,王海燕.慢性肾脏病的流行病学研究[J].中华肾脏病杂志,2005, 21(7):425-428.[5] Goosen JH, Kums AJ, Kollen BJ,et al. Porous-coated femoral components with or without hydroxyapatite in primary uncemented total hip arthroplasty: a systematic review of randomized controlled trials.Arch Orthop Trauma Surg. 2009; 129(9):1165-1169.[6] Epinette JA, Manley MT. Uncemented stems in hip replacement--hydroxyapatite or plain porous: does it matter? Based on a prospective study of HA Omnifit stems at 15-years minimum follow-up.Hip Int. 2008;18(2):69-74.[7] Rahmy AI, Gosens T, Blake GM,et al. Periprosthetic bone remodelling of two types of uncemented femoral implant with proximal hydroxyapatite coating: a 3-year follow-up study addressing the influence of prosthesis design and preoperative bone density on periprosthetic bone loss. Osteoporos Int. 2004;15(4):281-289. [8] Nagoya S, Nagao M, Takada J,et al. Efficacy of cementless total hip arthroplasty in patients on long-term hemodialysis. J Arthroplasty. 2005;20(1):66-71.[9] Harris WH.Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737-755.[10] Ware JE Jr, Gandek B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol. 1998;51(11):903-912.[11] Coco M, Rush H. Increased incidence of hip fractures in dialysis patients with low serum parathyroid hormone.Am J Kidney Dis. 2000;36(6):1115-1121.[12] Alem AM, Sherrard DJ, Gillen DL,et al. Increased risk of hip fracture among patients with end-stage renal disease.Kidney Int. 2000;58(1):396-399.[13] Qiu MC. Beijing:People’s Medical Publishing House. 2003: 1075-1098.邱明才.代谢性骨病学[M].北京:人民卫生出版社,2003: 1075- 1098.[14] Qiu WQ. Linchuang Huicui. 2001;16(1):33-34.邱维强.肾性骨病诊断与治疗研究进展[J].临床荟萃,2001,16(1): 33-34.[15] Mataliotakis G, Lykissas MG, Mavrodontidis AN,et al. Femoral neck fractures secondary to renal osteodystrophy. Literature review and treatment algorithm. J Musculoskelet Neuronal Interact. 2009;9(3):130-137.[16] Chen SY,Wu BD,Lian XJ,et al. Linchuang Shenzhangbing Zazhi. 2008;8(1):18-20.陈珊莹,吴彼得,连学坚,等.低分子肝素在连续血液净化中抗凝作用的探讨[J].临床肾脏病杂志,2008,8(1):18-20.[17] Chen JD,Hou SX,Li WF. Zhonghua Quanke Yishi Zazhi. 2007; 6(1):55-56.陈金栋,侯树勋,李文锋.慢性肾功能不全骨科患者的围手术期处理[J].中华全科医师杂志,2007,6(1):55-56.[18] Karaeminogullari O, Demirors H, Sahin O,et al. Analysis of outcomes for surgically treated hip fractures in patients undergoing chronic hemodialysis. J Bone Joint Surg Am. 2007; 89(2):324-331.[19] Kalra S, McBryde CW, Lawrence T. Intracapsular hip fractures in end-stage renal failure. Injury. 2006;37(2):175-184.[20] Lv HS. Beijing:People’s Medical Publishing House. 2007.吕厚山.现代人工关节外科学[M].北京:人民卫生出版社, 2007.[21] Li WC, Shih CH, Ueng SW,et al. Uncemented total hip arthroplasty in chronic hemodialysis patients.Acta Orthop. 2010;81(2):178-182. [22] Nagoya S, Nagao M, Takada J, et al. Efficacy of cementless total hip arthroplasty in patients on long-term hemodialysis. J Arthroplasty. 2005;20(1):66-71.[23] Huang GY,Wei YB,Wu JG. Zhongguo Gu yu Guanjie Shunshang Zazhi. 2010;25(1):60-61.黄钢勇,魏亦兵,吴建国.终末期肾病患者的全髋关节置换[J].中国骨与关节损伤杂志,2010,25(1):60-61.[24] 中华医学会骨科学分会. 中国骨科大手术静脉血栓栓塞症预防指南[J].中华关节外科杂志:电子版,2009,3(3):380-383.[25] Zhang B,Shi W. Zhonghua Shenzhangbing Zazhi. 2004; 20(2):145-146.章斌,史伟.终末期肾病血管钙化机制[J].中华肾脏病杂志,2004, 20(2):145-146.[26] Zhou Y,Zhu N,Yuan WJ. Zhonghua Shenzhangbing Zazhi. 2012; 28(6):495-497.周益,朱楠,袁伟杰.慢性肾脏病患者骨-血管轴调节紊乱的研究现状[J]. 中华肾脏病杂志,2012, 28(6):495-497.[27] London GM, Marty C, Marchais SJ,et al. Arterial calcifications and bone histomorphometry in end-stage renal disease. J Am Soc Nephrol. 2004;15(7):1943-1951.[28] Raggi P, Boulay A, Chasan-Taber S,et al. Cardiac calcification in adult hemodialysis patients. A link between end-stage renal disease and cardiovascular disease. J Am Coll Cardiol. 2002; 39(4):695-701.[29] Latos DL.Chronic dialysis in patients over age 65.J Am Soc Nephrol. 1996;7(5):637-646.[30] Chen XM. Beijing:People’s Military Medical Press. 2006: 45-50, 238-258.陈香美.现代慢性肾衰治疗学[M].北京:人民军医出版社,2006: 45-50,238-258.[31] Ryg J, Rejnmark L, Overgaard S,et al. Hip fracture patients at risk of second hip fracture: a nationwide population-based cohort study of 169,145 cases during 1977-2001.J Bone Miner Res. 2009;24(7):1299-1307.[32] Kaukonen JP, Lüthje P, Nurmi-Lüthje I,et al.Second hip fracture and patients' medication after the first hip fracture: a follow-up of 221 hip fracture patients in Finland. Arch Gerontol Geriatr. 2011;52(2):185-189.[33] Lips P, van Schoor NM.Quality of life in patients with osteoporosis.Osteoporos Int. 2005;16(5):447-455.[34] Alvarez-Nebreda ML, Jiménez AB, Rodríguez P,et al. Epidemiology of hip fracture in the elderly in Spain.Bone. 2008; 42(2):278-285.[35] Abbott KC, Bucci JR, Agodoa LY.Total hip arthroplasty in chronic dialysis patients in the United States. J Nephrol. 2003; 16(1):34-39.[36] Sakai S, David D, Shoji H,et al. Bone injuries due to tetany or convulsions during hemodialysis.Clin Orthop Relat Res. 1976; (118):118-123.[37] Taylor LJ, Grant SC. Bilateral fracture of the femoral neck during a hypocalcaemic convulsion. A case report. J Bone Joint Surg Br. 1985;67(4):536-537.[38] Ye CY,Cao CH,Fu WC. Zhongguo Guzhi Shusong Zazhi. 2004;10(1):87-89.叶朝阳,曹春华,付文成. 鲑鱼降钙素对血透患者肾性骨病的疗效观察[J].中国骨质疏松杂志,2004,10(1):87-89.[39] Tang Y,Zhong YH,Gong SM. Zhonghua Shenzhangbing Zazhi. 2011;27(6):406-410.汤颖,钟一红,龚邵敏.终末期肾病血液透析患者感染死亡事件调查[J].中华肾脏病杂志,2011,27(6):406-410.[40] Sunday JM, Guille JT, Torg JS. Complications of joint arthroplasty in patients with end-stage renal disease on hemodialysis. Clin Orthop Relat Res. 2002;(397):350-355.[41] Sakalkale DP, Hozack WJ, Rothman RH.Total hip arthroplasty in patients on long-term renal dialysis. J Arthroplasty. 1999; 14(5):571-575. |
| [1] | Peng Zhihao, Feng Zongquan, Zou Yonggen, Niu Guoqing, Wu Feng. Relationship of lower limb force line and the progression of lateral compartment arthritis after unicompartmental knee arthroplasty with mobile bearing [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1368-1374. |
| [2] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [3] | Du Xiupeng, Yang Zhaohui. Effect of degree of initial deformity of impacted femoral neck fractures under 65 years of age on femoral neck shortening [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1410-1416. |
| [4] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [5] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [6] | Liu Xiangxiang, Huang Yunmei, Chen Wenlie, Lin Ruhui, Lu Xiaodong, Li Zuanfang, Xu Yaye, Huang Meiya, Li Xihai. Ultrastructural changes of the white zone cells of the meniscus in a rat model of early osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1237-1242. |
| [7] | Liu Xin, Yan Feihua, Hong Kunhao. Delaying cartilage degeneration by regulating the expression of aquaporins in rats with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 668-673. |
| [8] | Ma Zetao, Zeng Hui, Wang Deli, Weng Jian, Feng Song. MicroRNA-138-5p regulates chondrocyte proliferation and autophagy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 674-678. |
| [9] | Cao Xuhan, Bai Zixing, Sun Chengyi, Yang Yanjun, Sun Weidong. Mechanism of “Ruxiang-Moyao” herbal pair in the treatment of knee osteoarthritis based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 746-753. |
| [10] | Li Yonghua, Feng Qiang, Tan Renting, Huang Shifu, Qiu Jinlong, Yin Heng. Molecular mechanism of Eucommia ulmoides active ingredients treating synovitis of knee osteoarthritis: an analysis based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 765-771. |
| [11] | Song Shan, Hu Fangyuan, Qiao Jun, Wang Jia, Zhang Shengxiao, Li Xiaofeng. An insight into biomarkers of osteoarthritis synovium based on bioinformatics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 785-790. |
| [12] | Deng Zhenhan, Huang Yong, Xiao Lulu, Chen Yulin, Zhu Weimin, Lu Wei, Wang Daping. Role and application of bone morphogenetic proteins in articular cartilage regeneration [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 798-806. |
| [13] | Zheng Li, Li Dadi, Hu Weifan, Tang Jinlong, Zhao Fengchao. Risk assessment of contralateral knee arthroplasty after unilateral total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 374-379. |
| [14] | Lü Jiaxing, Bai Leipeng, Yang Zhaoxin, Miao Yuesong, Jin Yu, Li Zhehong, Sun Guangpu, Xu Ying, Zhang Qingzhu. Evaluation of internal fixation with proximal femoral nail antirotation in elderly knee osteoarthritis patients with femoral intertrochanteric fractures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 391-396. |
| [15] | Luo Anyu, Liu Hanlin, Xie Xiaofei, Huang Chen. Effect of antioxidant mixture on structural degeneration of an osteoarthritis rat model [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(23): 3625-3629. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||