Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (8): 1693-1704.doi: 10.12307/2025.242
Previous Articles Next Articles
Effects of wearable electronic device-based interventions on physical activity and sedentary behavior in healthy adolescents: a meta-analysis
Wang Yida1, Liu Jun1, Wang Xiaoling1, Wang Liyan2, Yang Chengru1, Zhang Xuexiao3
- 1School of Sport and Health Sciences, Dalian University of Technology, Dalian 116024, Liaoning Province, China; 2College of Rehabilitation Science, Shanghai University of Medicine and Health Sciences, Shanghai 201318, China; 3Graduate Student Affairs Department, Shenyang Sport University, Shenyang 110102, Liaoning Province, China
-
Received:2023-12-04Accepted:2024-01-23Online:2025-03-18Published:2024-07-06 -
Contact:Liu Jun, Master, Professor, Master’s supervisor, School of Sport and Health Sciences, Dalian University of Technology, Dalian 116024, Liaoning Province, China -
About author:Wang Yida, Master candidate, School of Sport and Health Sciences, Dalian University of Technology, Dalian 116024, Liaoning Province, China -
Supported by:Liaoning Provincial Social Science Planning Fund Project, No. L22BTY002 (to LJ); Liaoning Province Sports Science Society Planning Project, No. 2022LTXH066 (to LJ)
CLC Number:
Cite this article
Wang Yida, Liu Jun, Wang Xiaoling, Wang Liyan, Yang Chengru, Zhang Xuexiao. Effects of wearable electronic device-based interventions on physical activity and sedentary behavior in healthy adolescents: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1693-1704.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
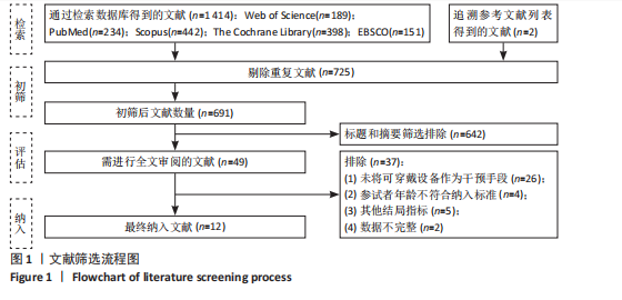
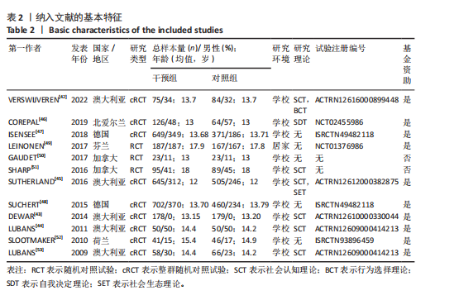
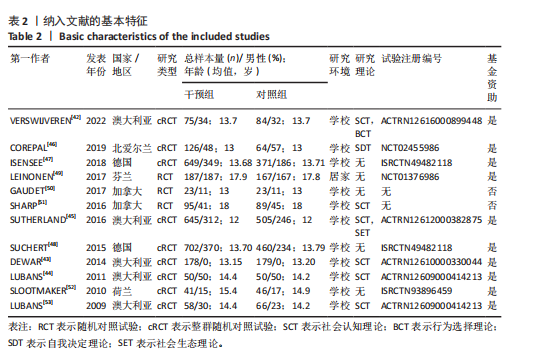
2.1 文献检索结果 经过逐步筛选共纳入12篇文章,包括3项随机对照试验和9项整群随机对照试验。图1概述了所纳入研究的筛选过程。首先使用检索策略对5个数据库进行了初步检索,共检索到1 414篇文章。追溯相关参考文献列表得到2篇文献。使用EndNote 21软件删除了725篇重复文献后,通过审查标题和摘要排除了642篇不相关的文献。最后,通过全文阅读共评估了49篇文章。其中,37篇文章被排除在外,最终纳入12篇文献[42-53]。 2.2 纳入研究的基本特征 纳入的12篇英文文献发表于2009-2022年[42-53],共包含4 933名受试者,每篇文章受试者23-702名,年龄12-18岁,主要国家包括澳大利亚(5篇)[42-45,53]、北爱尔兰(1篇)[46]、德国(2篇)[47-48]、芬兰(1篇)[49]、加拿大(2篇)[50-51]、荷兰(1篇)[52],具体的纳入文献特征见表2,3。 有11篇文献是在学校环境中进行试验[42-48,50-53],而1篇文献在家庭环境中进行试验[49]。有3项研究是随机对照试验[49-51],9项研究是整群随机对照试验[42-48,52-53]。有9项研究使用腰部或臀部佩戴的计步器作为活动追踪器[43-48,51-53],而3项研究使用"
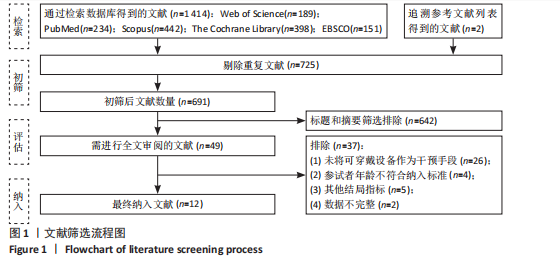

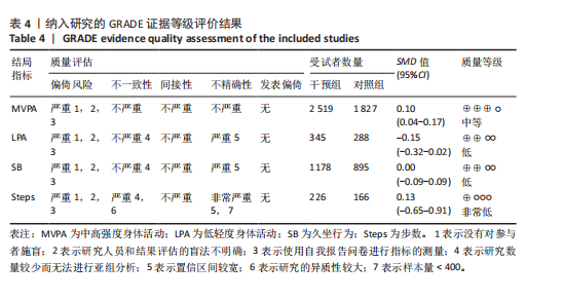
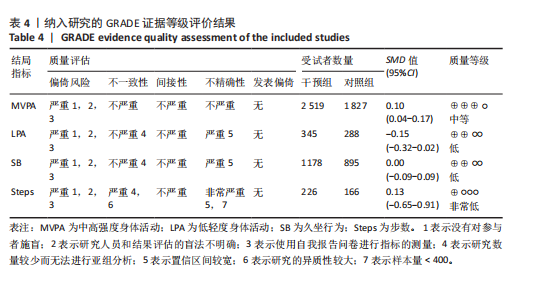
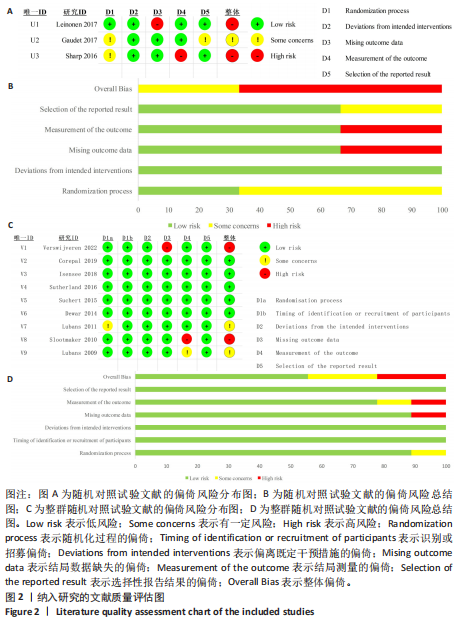
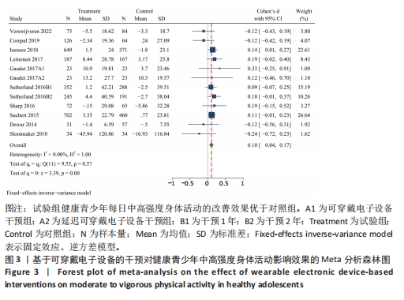
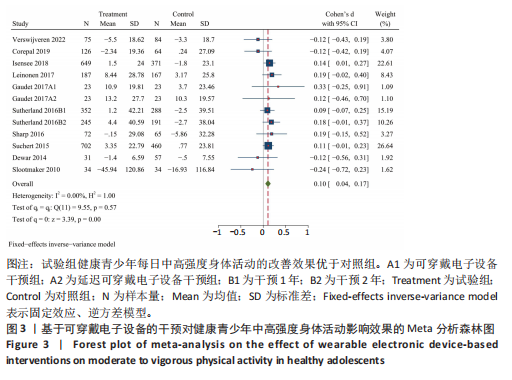
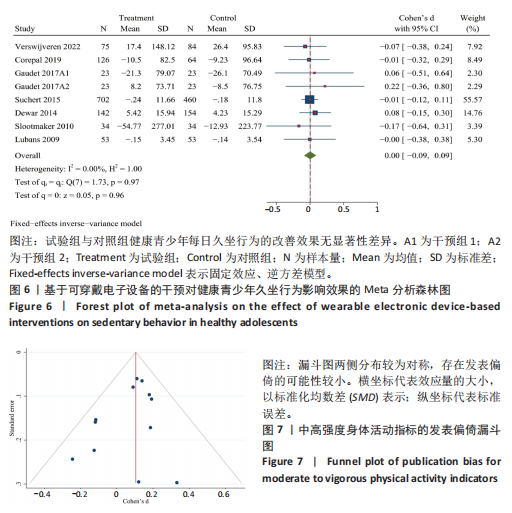
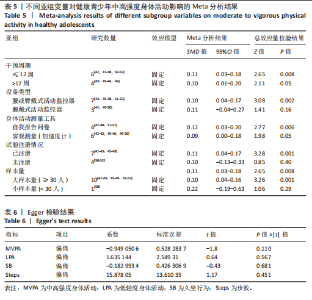
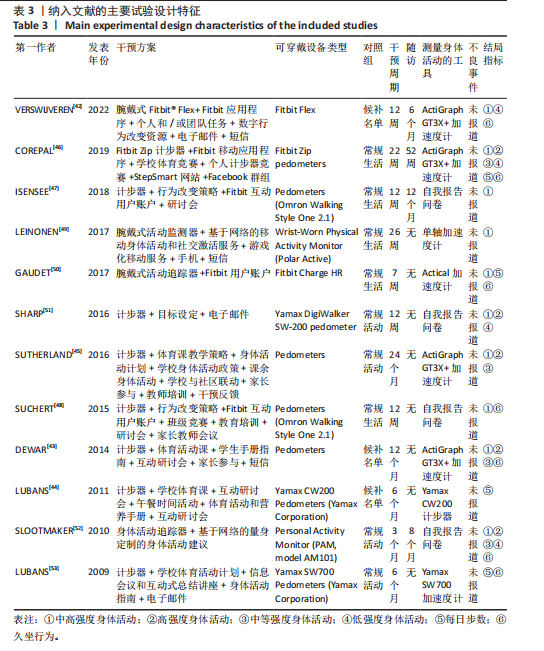
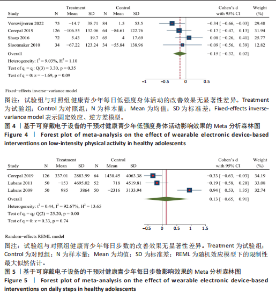
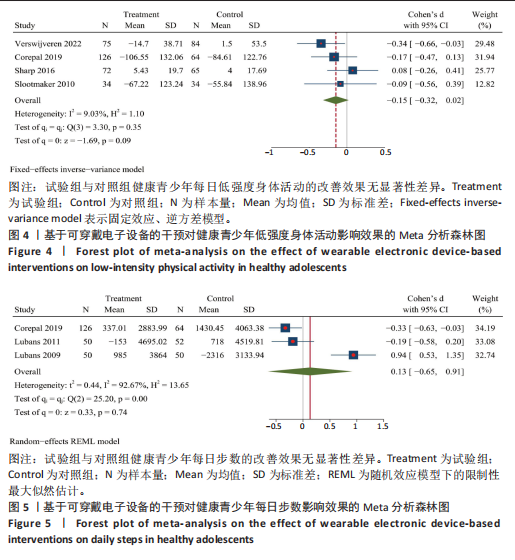
腕带式活动追踪器[42,49-50]。干预周期7-96周,随访期从24-52周。结局指标包括中高强度身体活动、高强度身体活动、中强度身体活动、低强度身体活动、久坐行为和每日步数。8项研究使用客观措施评估身体活动[42-46,49,50,53],而4项研究使用自我报告问卷[47-48,51-52]。有7项研究使用行为改变研究理论,包括社会认知理论[42-46,51,53]、自我决定理论[46]、行为选择理论[42]、社会生态理论[45]。有10项试验已在临床试验注册中心注册[42-49,52-53],而2项试验未注册[50-51]。有10项研究获得了基金资助[42-49,52,53],而2项研究没有获得任何资助[50-51]。在实施干预的方法方面,除了可穿戴身体活动追踪器,还涉及移动应用程序、个人或小组会议、学校体育竞赛、电子邮件、手机、网站、短信、Facebook群组、身体活动和营养手册等。对照组不进行干预,但被要求进行常规活动。 2.3 文献质量评价结果 使用RoB 2工具评估的偏倚风险结果见图2。对于随机对照试验,33.3%为“有一定风险”,66.7%为“高风险”;对于整群随机对照试验,55.6%被评为“低风险”,22.2%为“有一定风险”,22.2%为“高风险”。 表4显示了基于可穿戴电子设备的干预对健康青少年每日中高强度身体活动、低强度身体活动、久坐行为和步数的GRADE证据概况。所有的指标中由于存在不良偏倚风险,如未使用盲法或没有详细说明盲法、使用自我报告的测量方法,因此证据被降一级。轻度身体活动和久坐行为由于存在严重的不精确性问题,如置信区间过宽,因此证据再降一级。每日步数由于存在严重的不一致性和不精确性问题,如异质性较大、置信区间过宽或样本量< 400人等,因此证据再降两级。最终,中高强度身体活动、低强度身体活动、久坐行为和每日步数的证据质量分别为中、低、低和非常低。 2.4 Meta分析结果 2.4.1 两组中高强度身体活动差异的Meta分析结果 基于可穿戴电子设备的干预对健康青少年中高强度身体活动研究共纳入12个研究,如图3所示。异质性检验具有较小的异质性(I2=0%,P > 0.1),故采用固定效应模型进行分析。合并效应量结果显示,与对照组相比,基于可穿戴电子设备的干预措施对中高强度身体活动(SMD=0.10,95%CI:0.04-0.17;Z=3.39;P < 0.05)有较小的有利影响。 2.4.2 两组低强度身体活动差异的Meta分析结果 基于可穿戴电子设备的干预对健康青少年低强度身体活动研究共纳入4个研究,如图4所示。异质性检验具有较小的异质性(I2=9.03%,P > 0.1),故采用固定效应模型进行分析。合并效应量结果显示,与对照组相比,基于可穿戴电子设备的干预措施不能有效改善健康青少年的每日低强度身体活动(SMD=-0.15,95%CI:-0.32-0.02;Z=-1.69;P > 0.05)。 2.4.3 两组每日步数差异的Meta分析结果 基于可穿戴电子设备的干预对健康青少年低强度身体活动研究共纳入3个研究,如图5所示。异质性检验(I2=92.67%,P > 0.1)具有较大的异质性,故采用随机效应模型进行分析。合并效应量结果显示,可穿戴电子设备干预与对照组的每日步数比较差异无显著性意义(SMD=0.13,95%CI:-0.65-0.91;Z=0.33;P > 0.05)。 2.4.4 两组久坐行为差异的Meta分析结果 基于可穿戴电子设备的干预对健康青少年久坐行为研究共纳入8个研究,如图6所示。异质性检验(I2=0%,P > 0.1)具有较小的异质性,故采用固定效应模型进行分析。合并效应量结果显示,可穿戴电子设备干预与对照组的久坐行为比较差异无显著性意义(SMD=0.00,95%CI:-0.09-0.09;Z=0.05;P > 0.05)。 2.4.5 两组中高强度身体活动差异的亚组Meta分析结果 为探讨其他成"
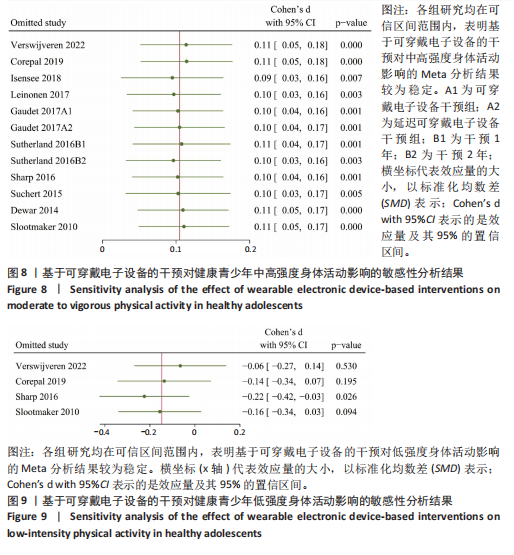
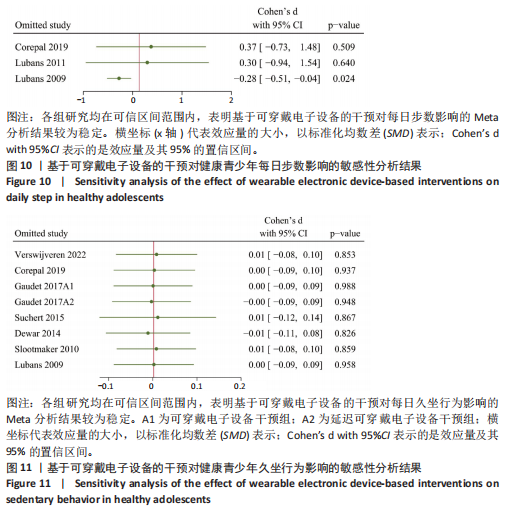
比(SMD=0.10,95%CI:0.01-0.20,P=0.05),≤12周的干预周期对每日中高强度身体活动有更加显著的促进效果(SMD=0.11,95%CI:0.03-0.18,P=0.008)。对于设备类型,与腕戴式活动追踪器相比(SMD=0.11,95%CI:-0.04-0.27,P=0.16),计步器 (佩戴在腰或臀)对每日中高强度身体活动有更加显著的促进效果(SMD=0.10,95%CI:0.04-0.17,P=0.002)。对于身体活动测量工具,与加速度计测量的中高强度身体活动相比(SMD=0.09,95%CI:0.00-0.18,P=0.05),通过问卷测量中高强度身体活动拥有更显著的增加值(SMD=0.12,95%CI:0.03-0.20,P=0.006)。与未进行试验注册相比(SMD=0.10,95%CI:-0.13-0.33,P=0.40),已通过注册的试验具有更显著的改善效果(SMD=0.11,95%CI:0.04-0.17,P=0.001)。最后,大样本量产生的效应量(SMD=0.10,95%CI:0.04-0.16;P=0.001)比小样本量的效应量(SMD=0.22,95%CI:-0.19-0.63,P=0.29)更加显著。 2.4.6 发表偏倚和敏感性分析结果 发表偏倚采用定性和定量的方法进行评估。根据以往经验,绘制漏斗图至少需要10个研究,并且对漏斗图进行非正式的直观检查容易得出错误的结论[54]。因此文章联合使用Egger检验评估纳入研究整体的发表偏倚规模[40],即对中高强度身体活动进行Egger检验和漏斗图分析,低强度身体活动、每日步数和久坐行为则进行Egger检验。结果显示,中高强度身体活动的漏斗图呈现出左右基本对称的形状,见图7,所有指标的发表偏倚漏斗图具有统计学上的显著对称性(P > 0.05),见表6。因此,综合判断纳入的所有文献均不存在发表偏倚。 为评估Meta分析结果的稳健性,文章进行了Leave-One-Out敏感性分析,即通过每次排除一个研究并重新计算整体效应量,来检验任何单一研究对整体结果的影响,结果如图8-11所示。结果显示,中高强度身体活动和久坐行为的整体效应量在排除任何单一研究后均保持了一致性。这表明Meta分析结果对单一研究的影响不敏感,结果较为稳定,即基于"
| [1] CASPERSEN CJ, POWELL KE, CHRISTENSON GM. Physical-activity, exercise, and physical-fitness - definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126-131. [2] PATE RR, O’NEILL JR, LOBELO F. The evolving definition of “sedentary”. Exerc Sport Sci Rev. 2008;36(4):173-178. [3] 郭海霞,饶思瑞.世界各国儿童青少年身体活动指南发展研究[J].中国体育科技, 2021,57(8):61-71. [4] 王军利,张思奇.儿童青少年身体活动指南的国际经验与启示[J].沈阳体育学院学报,2022,41(5):82-88. [5] DONG RB, DOU KY. Changes in physical activity level of adolescents and its relationship with mental health during regular COVID-19 prevention and control. Brain Behav. 2023;13(9):e3116. [6] GUTHOLD R, STEVENS GA, RILEY LM, et al. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1.6 million participants. Lancet Child Adolesc Health. 2020;4(1):23-35. [7] PECHTL SML, KIM LP, JACOBSEN KH. Physical inactivity and sedentariness: languorous behavior adolescents in 80 countries. J Adolesc Health. 2022;70(6):950-960. [8] LIU Y, KE Y, LIANG Y, et al. Results from the China 2022 report card on physical activity for children and adolescents. J Exerc Sci Fit. 2023;21(1):1-5. [9] KRAVITZ AV, O’NEAL TJ, FRIEND DM. Do dopaminergic impairments underlie physical inactivity in people with obesity? Front Hum Neurosci. 2016;10:514. [10] LIPPI G, HENRY BM, SANCHIS-GOMAR F. Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID-19). Eur J Prev Cardiol. 2020; 27(9):906-908. [11] DíAZ-MARTíNEZ X, PETERMANN F, LEIVA AM, et al. No cumplir con las recomendaciones de actividad física se asocia a mayores niveles de obesidad, diabetes, hipertensión y síndrome metabólico en población chilena. Rev Med Chile. 2018;146(5):585-595. [12] POSES-FERRER E, PARISI R, GONZALEZ-VIANA A, et al. Daily sitting time and its association with non-communicable diseases and multimorbidity in Catalonia. Eur J Public Health. 2022;32(1):105-111. [13] KERR NR, BOOTH FW. Contributions of physical inactivity and sedentary behavior to metabolic and endocrine diseases. Trends Endocrinol Metab. 2022;33(12):817-827. [14] PENGPID S, PELTZER K. Associations of loneliness with poor physical health, poor mental health and health risk behaviours among a nationally representative community-dwelling sample of middle-aged and older adults in India. Int J Geriatr Psychiatry. 2021;36(11):1722-1731. [15] KANTOMAA MT, STAMATAKIS E, KANKAANPÄÄ A, et al. Physical activity and obesity mediate the association between childhood motor function and adolescents’ academic achievement. Proc Natl Acad Sci USA. 2013;110(5):1917-1922. [16] LEE IM, SHIROMA EJ, LOBELO F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219-229. [17] THOMPSON WR. Worldwide survey of fitness trends for 2022. Acsms Health Fit J. 2022;26(1):11-20. [18] NATALUCCI V, MARMONDI F, BIRAGHI M, et al. The effectiveness of wearable devices in non-communicable diseases to manage physical activity and nutrition: where We Are? Nutrients. 2023;15(4):913. [19] RIDGERS ND, MCNARRY MA, MACKINTOSH KA. Feasibility and effectiveness of using wearable activity trackers in youth: a systematic review. Jmir Mhealth Uhealth. 2016;4(4):e129. [20] DüKING P, HOLMBERG HC, SPERLICH B. Instant biofeedback provided by wearable sensor technology can help to optimize exercise and prevent injury and overuse. Front Physiol. 2017;8:167. [21] CREASER AV, CLEMES SA, COSTA S, et al. The acceptability, feasibility, and effectiveness of wearable activity trackers for increasing physical activity in children and adolescents: a systematic review. Int J Environ Res Public Health. 2021;18(12):6211. [22] CASADO-ROBLES C, VICIANA J, GUIJARRO-ROMERO S, et al. Effects of Consumer-wearable activity tracker-based programs on objectively measured daily physical activity and sedentary behavior among school-aged children: a systematic review and meta-analysis. Sports Med Open. 2022;8(1):18. [23] TANG MSS, MOORE K, MCGAVIGAN A, et al. Effectiveness of wearable trackers on physical activity in healthy adults: systematic review and meta-analysis of randomized controlled trials. Jmir Mhealth Uhealth. 2020;8(7):e15576. [24] LIU JY, KOR PP, CHAN CP, et al. The effectiveness of a wearable activity tracker (WAT)-based intervention to improve physical activity levels in sedentary older adults: a systematic review and meta-analysis. Arch Gerontol Geriat. 2020;91: 104211. [25] 张丹青,孙建刚,刘雪琦,等.基于可穿戴设备的儿童青少年身体活动干预效果综述[J].上海体育学院学报,2019,43(5): 41-49,98. [26] OCAGLI H, AGARINIS R, AZZOLINA D, et al. Physical activity assessment with wearable devices in rheumatic diseases: a systematic review and meta-analysis. Rheumatology. 2023;62(3):1031-1046. [27] SINGH B, ZOPF E M, HOWDEN E J. Effect and feasibility of wearable physical activity trackers and pedometers for increasing physical activity and improving health outcomes in cancer survivors: a systematic review and meta-analysis. J Sport Health Sci. 2022;11(2):184-193. [28] HAN X, LI P, YANG Y, et al. An exploration of the application of step counter-based physical activity promotion programs in patients with chronic obstructive pulmonary disease: a systematic review. Front Public Health. 2021;9:691554. [29] FRANSSEN WMA, FRANSSEN GHLM, SPAAS J, et al. Can consumer wearable activity tracker-based interventions improve physical activity and cardiometabolic health in patients with chronic diseases? A systematic review and meta-analysis of randomised controlled trials. Int J Behav Nutr Phys Act. 2020;17(1):57. [30] ALAM S, ZHANG M, HARRIS K, et al. The impact of consumer wearable devices on physical activity and adherence to physical activity in patients with cardiovascular disease: a systematic review of systematic reviews and meta-analyses. Telemed J E Health. 2022;29(7):986-1000. [31] WONG SH, TAN ZYA, CHENG LJ, et al. Wearable technology-delivered lifestyle intervention amongst adults with overweight and obese: a systematic review and meta-regression. Int J Nurs Stud. 2022; 127:104163. [32] CAI X, QIU SH, YIN H, et al. Pedometer intervention and weight loss in overweight and obese adults with Type 2 diabetes: a meta-analysis. Diabetic Med. 2016;33(8): 1035-1044. [33] BöHM B, KARWIESE SD, BöHM H, et al. Effects of mobile health including wearable activity trackers to increase physical activity outcomes among healthy children and adolescents: systematic review. Jmir Mhealth Uhealth. 2019;7(4):e8298. [34] PAGE MJ, MCKENZIE JE, BOSSUYT PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [35] STOVOLD E, BEECHER D, FOXLEE R, et al. Study flow diagrams in Cochrane systematic review updates: an adapted PRISMA flow diagram. Syst Rev-London. 2014;3(1):54. [36] AGUAYO-ALBASINI JL, FLORES-PASTOR B, SORIA-ALEDO V. GRADE system: Classification of quality of evidence and strength of recommendation. Cir Espan. 2014;92(2):82-88. [37] GUYATT GH, OXMAN AD, SCHüNEMANN HJ, et al. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64(4):380-382. [38] STERNE JAC, SAVOVIĆ J, PAGE MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [39] CHAPUT JP, WILLUMSEN J, BULL F, et al. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: summary of the evidence. Int J Behav Nutr Phys Act. 2020;17(1):141. [40] EGGER M, SMITH GD, SCHNEIDER M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109): 629-634. [41] WAN X, WANG W, LIU J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. [42] VERSWIJVEREN SJJM, ABBOTT G, LAI S K, et al. Mediators of effects on physical activity and sedentary time in an activity tracker and behavior change intervention for adolescents: secondary analysis of a cluster randomized controlled trial. Jmir Mhealth Uhealth. 2022;10(8):e35261. [43] DEWAR DL, MORGAN PJ, PLOTNIKOFF RC, et al. Exploring changes in physical activity, sedentary behaviors and hypothesized mediators in the NEAT girls group randomized controlled trial. J Sci Med Sport. 2014;17(1):39-46. [44] LUBANS DR, MORGAN PJ, AGUIAR EJ, et al. Randomized controlled trial of the Physical Activity Leaders (PALs) program for adolescent boys from disadvantaged secondary schools. Prev Med. 2011;52(3): 239-246.
[45] SUTHERLAND R, CAMPBELL E, LUBANS DR, et al. ‘Physical Activity 4 Everyone’ school-based intervention to prevent decline in adolescent physical activity levels: 12 month (mid-intervention) report on a cluster randomised trial. Br J Sports Med. 2016;50(8):488-495. [46] COREPAL R, BEST P, O’NEILL R, et al. A feasibility study of ‘The StepSmart Challenge’ to promote physical activity in adolescents. Pilot Feasibility St. 2019; 5(1):132. [47] ISENSEE B, SUCHERT V, HANSEN J, et al. Effects of a school-based pedometer intervention in adolescents: 1-year follow-up of a cluster-randomized controlled trial. J Sch Health. 2018;88(10):717-724. [48] SUCHERT V, ISENSEE B, SARGENT J, et al. Prospective effects of pedometer use and class competitions on physical activity in youth: a cluster-randomized controlled trial. Prev Med. 2015;81:399-404. [49] LEINONEN AM, PYKY R, AHOLA R, et al. Feasibility of gamified mobile service aimed at physical activation in young men: population-based randomized controlled study (MOPO). Jmir Mhealth Uhealth. 2017;5(10):e146. [50] GAUDET J, GALLANT F, BéLANGER M. A bit of fit: minimalist intervention in adolescents based on a physical activity tracker. Jmir Mhealth Uhealth. 2017;5(7):e92. [51] SHARP P, CAPERCHIONE C. The effects of a pedometer-based intervention on first-year university students: a randomized control trial. J Am Coll Health. 2016;64(8):630-638. [52] SLOOTMAKER SM, CHINAPAW MJM, SEIDELL JC, et al. Accelerometers and Internet for physical activity promotion in youth? Feasibility and effectiveness of a minimal intervention [ISRCTN93896459]. Prev Med. 2010;51(1):31-36. [53] LUBANS DR, MORGAN PJ, CALLISTER R, et al. Effects of integrating pedometers, parental materials, and e-mail support within an extracurricular school sport intervention. J Adolesc Health. 2009;44(2):176-183. [54] KOSSMEIER M, TRAN US, VORACEK M. Visual inference for the funnel plot in meta-analysis. Z Psychol. 2019;227(1):83-89. [55] WANG W, CHENG J, SONG W, et al. The effectiveness of wearable devices as physical activity interventions for preventing and treating obesity in children and adolescents: systematic review and meta-analysis. Jmir Mhealth Uhealth. 2022;10(4):e32435. [56] BRICKWOOD KJ, WATSON G, O’BRIEN J, et al. Consumer-based wearable activity trackers increase physical activity participation: systematic review and meta-analysis. Jmir Mhealth Uhealth. 2019;7(4):e11819. [57] METCALF B, HENLEY W, WILKIN T. Effectiveness of intervention on physical activity of children: systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54). BMJ. 2012;345:e5888. [58] YEN HY, HUANG HY. Comparisons of physical activity and sedentary behavior between owners and non-owners of commercial wearable devices. Perspect Public Health. 2021;141(2):89-96. [59] RUPP MA, MICHAELIS JR, MCCONNELL DS, et al. The role of individual differences on perceptions of wearable fitness device trust, usability, and motivational impact. Appl Ergon. 2018;70:77-87. [60] GHAHFAROKHI AD, VOSADI E, BARZEGAR H, et al. The effect of wearable and smartphone applications on physical activity, quality of life, and cardiovascular health outcomes in overweight/obese adults: a systematic review and meta-analysis of randomized controlled trials. Biol Res Nurs. 2022;24(4):503-518. [61] KIRK M A, AMIRI M, PIRBAGLOU M, et al. Wearable technology and physical activity behavior change in adults with chronic cardiometabolic disease: a systematic review and meta-analysis. Am J Health Promot. 2019;33(5):778-791. [62] BROWN JC, GILMORE LA. Physical activity reduces the risk of recurrence and mortality in cancer patients. Exerc Sport Sci Rev. 2020;48(2):67-73. [63] MUNSIE C, EBERT J, JOSKE D, et al. The benefit of physical activity in adolescent and young adult cancer patients during and after treatment: a systematic review. J Adolesc Young Adul. 2019;8(5):512-524. [64] BAILLOT A, CHENAIL S, BARROS POLITA N, et al. Physical activity motives, barriers, and preferences in people with obesity: a systematic review. PLoS One. 2021;16(6):e0253114. [65] HUSSIEN J, BRUNET J, ROMAIN AJM, et al. Living with severe obesity: adults’ physical activity preferences, self-efficacy to overcome barriers and motives. Disabil Rehabil. 2022;44(4):590-599. [66] CHEVANCE G, BARETTA D, GOLASZEWSKI N, et al. Goal setting and achievement for walking: a series of n-of-1 digital interventions. Health Psychol. 2021;40(1): 30-39. [67] ANSON D, MADRAS D. Do low step count goals inhibit walking behavior: a randomized controlled study. Clin Rehabil. 2015;30(7):676-685. [68] MILLER BG, LIVINGSTON CP, ZERGER HM, et al. Evaluating public posting, goal setting, and rewards to increase physical activity in children. Behav Int. 2023;38(1):105-117. [69] GONZALEZ-CUTRE D, ROMERO-ELIAS M, JIMENEZ-LOAISA A, et al. Testing the need for novelty as a candidate need in basic psychological needs theory. Motiv Emotion. 2020;44(2):295-314. [70] STEEL RP. The longitudinal associations between wearable technology, physical activity and self-determined motivation. Int J Sport Exerc Psychol. 2023;1-18. [71] SCHAEFER SE, CHING CC, BREEN H, et al. Wearing, thinking, and moving: testing the feasibility of fitness tracking with urban youth. Am J Health Educ. 2016;47(1):8-16. [72] CHONG KPL, GUO JZ, DENG X, et al. Consumer perceptions of wearable technology devices: retrospective review and analysis. Jmir Mhealth Uhealth. 2020; 8(4):e17544. [73] HAGSTROMER M, AINSWORTH B E, OJA P, et al. Comparison of a subjective and an objective measure of physical activity in a population sample. J Phys Act Health. 2010;7(4):541-550. [74] SMITH SM, DWORKIN RH. Prospective clinical trial registration: not sufficient, but always necessary. Anaesthesia. 2018; 73(5):538-541. [75] CAJITA MI, KLINE CE, BURKE LE, et al. Feasible but not yet efficacious: a scoping review of wearable activity monitors in interventions targeting physical activity, sedentary behavior, and sleep. Curr Epidemiol Rep. 2020;7(1):25-38. [76] HANNAN AL, HARDERS MP, HING WY, et al. Impact of wearable physical activity monitoring devices with exercise prescription or advice in the maintenance phase of cardiac rehabilitation: systematic review and meta-analysis. Bmc Sports Sci Med Rehabil. 2019;11:14. [77] SLOAN RA, KIM Y, SAHASRANAMAN A, et al. The influence of a consumer-wearable activity tracker on sedentary time and prolonged sedentary bouts: secondary analysis of a randomized controlled trial. BMC Res Notes. 2018;11(1):189. [78] COMMISSARIS DA, HUYSMANS MA, MATHIASSEN SE, et al. Interventions to reduce sedentary behavior and increase physical activity during productive work: a systematic review. Scand J Work Environ Health. 2016;(3):181-191. [79] COLL F, CAVALHERI V, GUCCIARDI DF, et al. Quantifying the effect of monitor wear time and monitor type on the estimate of sedentary time in people with COPD: systematic review and meta-analysis. J Clin Med. 2022;11(7):1980. |
| [1] | Li Hanyue, Li Yini, Xiang Linmei, Li Sen. Effects of resistance exercise therapy on pain and function in patients with cervical spondylotic radiculopathy: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 987-996. |
| [2] | Sun Jiahe, Shi Jipeng, Zhu Tianrui, Quan Helong, Xu Hongqi. Effect of exercise intervention in elderly individuals with sarcopenia and its comorbidities: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 997-1007. |
| [3] | Sun Yundi, Cheng Lulu, Wan Haili, Chang Ying, Xiong Wenjuan, Xia Yuan. Effect of neuromuscular exercise for knee osteoarthritis pain and function: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1945-1952. |
| [4] | Wang Juan, Wang Guanglan, Zuo Huiwu. Efficacy of exercise therapy in the treatment of anterior cruciate ligament reconstruction patients: #br# a network meta-analysis #br# [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1714-1726. |
| [5] | Zheng Huakun, Yin Mingyue, Liu Qian. Effects of interval and continuous training on the quality of life in physically inactive adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1727-1740. |
| [6] | Wang Feng, Cao Chunfeng, He Chao, Zhang Tao, Zhou Zixian, Zhu Fengchen. All-inside versus traditional techniques of anterior cruciate ligament reconstruction: meta-analysis of therapeutic efficacy and radiological outcomes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7629-7638. |
| [7] | Liu Liguo, Qiu Mingwang, Huang Yanling, Fan Zhiyong, Wu Shan, Guo Rusong. Reporting quality of randomized controlled trials on acupuncture and manipulation for greater occipital neuralgia evaluated using the CONSORT statement and STRICTA checklist [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6566-6573. |
| [8] | Yu Bingbing, Wang Tingting, Fang Junlin, Guo Yun, Huang Yingru. Acupuncture for treatment of postmenopausal osteoporosis: meta-analysis, systematic evaluation and trial sequential analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6305-6316. |
| [9] | Wang Jinfu, Yang Guan. Meta-analysis of wearable device interventions to promote physical activity in older adults [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(28): 6146-6160. |
| [10] | Deng Yiran, Wang Xianliang, Li Dandan. Meta-analysis of exercise intervention on cardiopulmonary function in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5203-5211. |
| [11] | Huang Renjun, Yang Jingyan, Ma She, Wang Chaoyi, Zhao Yuyang, Yu Dong. Causal relationship between sedentary and physical activity levels in the Oswestry disability index score and intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(2): 322-330. |
| [12] | Hong Jintao, Wang Jingjing, Li Yansong, Wang Chen, Mi Shouling. Sedentary behavior and lower-limb muscle strength in community-dwelling older adults: the mediating and moderating effects of fear of falling and age [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(17): 3566-3571. |
| [13] | Yin Mingyue, Liu Qian, Xu Xiongzhuang, Ma Zhiying, Deng Shengji, Deng Jianfeng, Li Yongming. Acute effects and moderators of sedentary interruption on vascular function in adults: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(17): 3684-3696. |
| [14] | Li Xiupeng, Su Yuying, Wang Yuetong, Peng Liang, Wang Yida, Jing Wen. Effect of low-volume high-intensity interval training on cardiovascular risk factor in obese or overweight populations: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(12): 2590-2604. |
| [15] | Zhong Jun, Wang Wen. Network meta-analysis of different anatomical repair strategies to improve chronic lateral ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1470-1476. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||