Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (33): 7241-7249.doi: 10.12307/2025.910
Previous Articles Next Articles
Complications of intra-prosthetic dissociation after hip arthroplasty
Liao Qiyu, Ru Jiangying
- Department of Orthopedics, Affiliated Qingyuan Hospital, Guangzhou Medical University, Qingyuan People’s Hospital, Qingyuan 511518, Guangdong Province, China
-
Received:2024-09-12Accepted:2024-11-19Online:2025-11-28Published:2025-04-15 -
Contact:Ru Jiangying, MD, Associate professor, Chief physician, Master’s supervisor, Department of Orthopedics, Affiliated Qingyuan Hospital, Guangzhou Medical University, Qingyuan People’s Hospital, Qingyuan 511518, Guangdong Province, China -
About author:Liao Qiyu, Master candidate, Department of Orthopedics, Affiliated Qingyuan Hospital, Guangzhou Medical University, Qingyuan People’s Hospital, Qingyuan 511518, Guangdong Province, China
CLC Number:
Cite this article
Liao Qiyu, Ru Jiangying. Complications of intra-prosthetic dissociation after hip arthroplasty[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7241-7249.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
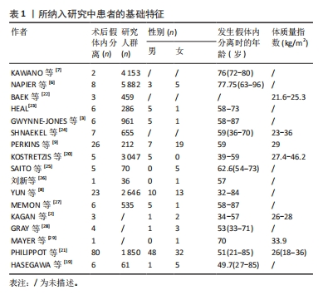
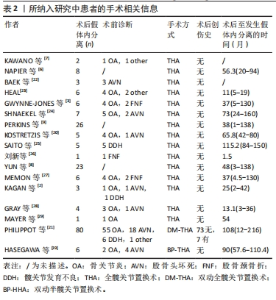
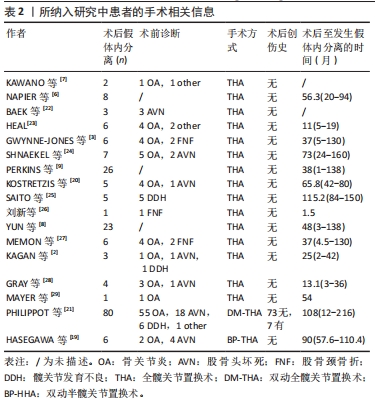
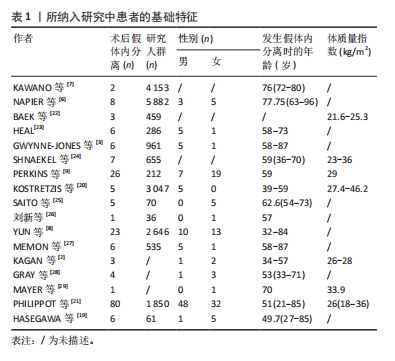
2.1 假体内分离的流行病学特点 假体内分离是髋关节置换术后发生的一种相对少见的并发症,据报道其发生概率为0.03%-12.26%[9,16]。有研究表明,假体内分离的发生风险可能与患者年龄或术后活动量有一定相关性;HASEGAWA等[19]研究报道,髋关节置换术后发生的6例假体内分离患者中,有3例患者年龄均未超过50岁,且其术后活动水平相对较高。在假体内分离患者性别方面,研究结果并不一致;KOSTRETZIS等[20]研究结果显示,髋关节置换术后发生的26例假体内分离患者中,女性患者的占比高达73%;而PHILIPPOT等[21]研究报道,男性患者占髋关节置换术后假体内分离发生总患者数的60%。假体内分离的发生风险还可能与患者体质量指数具有相关性;KOSTRETZIS等[20]研究表明,髋关节置换术后发生假体内分离的所有患者均为超重状态(体质量指数≥27 kg/m2)。此外,患者不同的术前诊断,可能对髋关节置换术后假体内分离并发症的发生风险产生一定的影响;在PHILIPPOT等[21]的一项临床研究中,对髋关节置换术后发生的80例假体内分离患者的术前诊断进行了详尽分析,其中包括骨关节炎55例(占69%)、股骨头坏死18例(占22%)、髋关节发育不良6例(占7%),其余疾病仅占2%。值得注意的是,PERKINS等[9]研究发现,髋关节置换术后早期发生衬垫分离并发症的概率较高,尤其对于初次行髋关节置换术的超重患者,术后36个月内发生衬垫分离尤为显著。经查阅文献,目前绝大多数假体内分离患者在髋关节置换术后并无明显创伤史,仅有4.8%的患者有创伤史记录[12],从患者自身因素来讲,假体内分离并发症发生的风险影响因素可因不同个体差异而定,但总体而言,对于术后活动量较大的中年患者、超重或术前诊断为骨关节炎的患者,其髋关节置换术后早期可能发生假体内分离并发症的风险更高,这可能与患髋解剖结构的破坏和肌肉的失衡有关。见表1,2。"
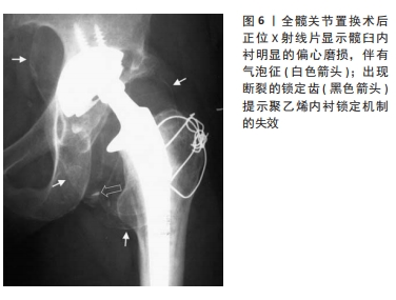
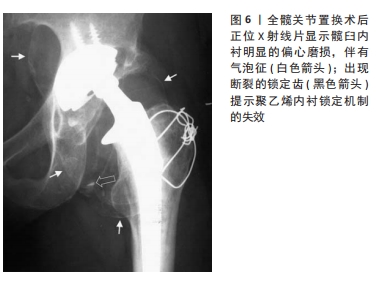
2.2 假体内分离的影像学特点 对于行髋关节置换术的患者而言,假体内分离并发症的发生可能会导致灾难性后果。因此,对该并发症的早期诊断显得尤为重要。尽管询问病史和体格检查能为临床医生提供诊断参考,但影像学评估仍是诊断假体内分离的有力基石。有趣的是,对于内衬未完全脱落的假体内分离,由于股骨头此时仍可能位于髋臼假体的中央,且能保持一定的活动性,在X射线片下可显示关节假体匹配良好的假象,仅有的异常征象是分离的假体在活动时可能会产生“吱吱声”[4,9,30],故对其诊断尤为困难。有研究报道,X射线片中特定的影像学征象,如股骨头呈偏心位置、“新月征”(股骨颈内侧见到的新月形透亮区)或“气泡征”(假体周围软组织或关节腔内出现泡沫状的异常影像,通常提示金属中毒或金属颗粒沉积引起的炎症反应)[31],以及超声下的“有轨迹征”(股骨颈前内侧的曲线形双高回声线)等[24],这些征象都有助于辨别聚乙烯衬垫相对于髋臼金属杯是否发生了错位或分离,并位移至周围软组织中[4,32-33],见图6。但由于技术员和放射科医生的经验受限,这些征象对于诊断内衬分离的敏感性和可靠性还有待进一步研究。另有研究报道,MRI和CT在准确定位聚乙烯衬垫方面显示出较高的有效性[32],尤其是CT双重对比关节造影以及金属伪影消减序列MRI成像,在诊断聚乙烯衬垫分离方面被认为更具有指导价值[34]。此外,相较于CT,MRI还具有检测软组织损伤的优势。"
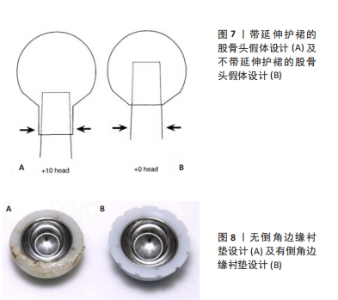
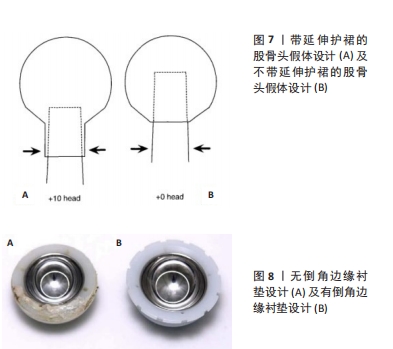
2.3 假体内分离发生的原因分析 2.3.1 假体内撞击 全髋关节置换术后金属股骨颈假体与髋臼杯凸出的金属边缘或聚乙烯衬垫等部件之间的撞击,在假体失稳中扮演着关键角色,其撞击发生的概率为39%-60% [35-37],可能是假体内分离发生的主要风险因素。在相互撞击下,假体间会产生离心负荷,导致聚乙烯磨损并产生微小颗粒,这些颗粒可导致假体锁定机制的松动和骨溶解,最终导致内衬变形以及假体内分离的发生[6,28,38-41]。 有研究表明,与全髋关节假体相比,双动头半髋假体可能存在更多的撞击因素,并产生更多的聚乙烯碎屑[40]。撞击因素主要包括髋臼杯位置过度偏移、股骨柄和髋臼杯之间的联合前倾角不足等[42-43]。此外,假体设计上存在缺陷,如带延伸护裙的股骨头、无倒角边缘的衬垫或大直径锥度股骨颈等,也是双动头半髋假体发生撞击的重要因素[41,44],见图7,8。加高边缘的髋臼衬垫设计相比中性衬垫,提高髋关节的稳定性的同时,可将假体内分离并发症的风险降低1.7倍[45]。然而,边缘加高的内衬搭配加长股骨颈被认为是发生撞击的最糟糕组合[36]。BARRACK等[11]发现,有50%发生假体内分离的髋关节置换患者使用了加长颈的股骨头,作者认为这种设计增加了颈部的厚度,并减小了髋关节的运动范围,在运动过程中更易发生碰撞,从而加速假体内部件锁定机制的失效[28]。"
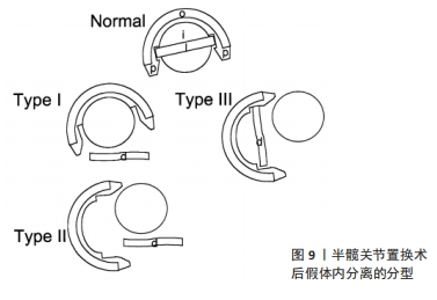
此外,有研究报道,髋关节发育不良、有酗酒史或腰椎融合手术史的患者,也被视为更易发生假体内撞击的高风险群体[2,46]。即使假体的设计和位置安放良好,由于骨盆倾斜变化或运动范围超出平均水平,也会导致撞击[44]。 因此,假体的设计需要高精度、高轻度的特性,以应对异常的生物力学负荷。 有研究表明,股骨头颈比与髋臼组件间的撞击率呈负相关关系[41],头颈比大于2.0和更大的股骨偏心距可以提高髋臼的稳定性,并降低撞击风险[35,44]。更大的股骨头假体通过增加两个关键优势来减少分离的风险:一是增加股骨颈与髋臼接触前的活动范围;二是增加股骨头与髋臼杯脱离前的跳跃距离,从而提供更多的“安全缓冲”[47]。同时,MALIK等[44]的病例报告中将撞击的原因归咎于假体设计和髋关节生物力学不匹配,并提出在选择股骨头的尺寸时需要考虑假体的使用材料,如在金属与高交联聚乙烯假体中,直径32 mm的股骨头可能是最佳选择;而对于钴铬合金与高交联聚乙烯或钴铬合金与陶瓷假体系统中,直径36 mm的股骨头可能更优[48]。值得一提的是,过大的股骨头也可能会带来一些问题,如内衬磨损、锥柄腐蚀和腹股沟疼痛[47],并增加股骨头与内衬间的吸附力和关节旋转扭矩[22]。在同一个髋臼杯中,股骨头直径增大会增加聚乙烯衬垫的接触面积,并降低了相对厚度,同时增加运动过程中股骨头假体的滑动距离和速度,这对聚乙烯衬垫的锁定机制造成了显著的应力负荷[24],进而增加假体内分离发生的风险。有研究指出,外径大于56 mm的髋臼组件由于提供了更多的潜在撞击区域,致使其发生撞击的概率明显增加[36]。因此,当股骨头直径增大到一定程度后,提高股骨偏心距会比单纯增加股骨头直径更有效地改善髋关节的活动范围[47]。 撞击往往是在髋关节屈曲基础上,联合内收和内旋或外展和外旋动作的结果[36]。有研究表明,髋关节屈曲可能与假体内分离之间存在关联,且在假体内分离发生之前,超过半数的患者有主观感觉的不稳定[4]。NAPIER等[6]报告中指出,8例出现假体内分离的患者中,有5例是在蹲姿站起时发生的。MAYER等[29]研究也报道假体内分离患者在发生衬垫分离前经历了多次重复下蹲的动作。尽管撞击可以增加脱位、磨损和假体断裂的风险,但撞击和假体内分离之间的直接关联性还需要进一步的研究来明确[44]。 2.3.2 假体自身因素 全髋关节置换术中,假体材料和制造工艺对于内衬的稳定性起着决定性作用。经过优化处理的传统非交联超高分子量聚乙烯衬垫替代物——高交联聚乙烯衬垫,是目前全髋关节置换术中最常用的髋臼内衬材料,其卓越的耐磨性广受临床欢迎[49-50],其线性磨损率为0.003-0.066 mm/年,远低于引起骨溶解的阈值0.1 mm/年[47,49,51-52],这种耐磨性主要通过伽马射线辐照和随后的重熔或退火等热稳定处理来实现。通过辐照可以促使聚乙烯分子间形成交联,显著提高了耐磨性能及抗张强度,同时减少了假体使用过程中磨损颗粒的释放[49];然而,过高剂量的辐照(达到或超过100 kGy)会导致过度交联,这不仅会降低材料的疲劳强度、抗裂纹扩展能力[29],还可能增加内衬断裂及发生假体内分离的风险[8,53]。此外,辐照过程产生的自由基有可能加速材料的氧化和降解[24],因此,随后采用恰当的热处理工艺来消除这些自由基是保证材料长期性能的关键。有研究指出,热稳定化处理能有效提升衬垫氧化稳定性,其中重熔过程在降低自由基和氧化指数方面比退火过程更为有效[49]。然而,不恰当的处理参数可能导致材料性能不均匀,影响最终的抗张强度,并增加锁定齿断裂的风险[29]。 金属臼杯与内衬间锁定机制的设计也是发生假体内分离的一个关键因素。对于Zimmer第1代和第2代以及Harris-Galante髋臼组件,由于锁定齿的脆弱和髋臼杯-内衬间的不匹配,故具有发生假体内分离的高风险性。因此,对于DePuy第2代 Duraloc髋臼组件,采用髋臼杯边缘的锁定环来防止衬垫脱落;其第3代Pinnacle髋臼组件则引入了内衬锥形锁定机制及锁定齿,以维持旋转稳定性[2]。虽然这种机制提供了能够适配金属、陶瓷和聚乙烯内衬的灵活性,但力学研究结果显示,Pinnacle髋臼组件分离所需的拔除力为144 N,且以6.6 N/年的速度递减[9];相比于上一代产品,其拔除力和杠杆翘出强度有所减弱[2],这可能是导致假体内分离发生的一个重要原因。因此,假体更新换代对衬垫分离的影响仍是一个令人关切的问题[29]。 假体设计中聚乙烯材料的厚度对假体性能也有重要影响。特别是在双动头半髋关节组件中,由于无需对髋臼侧进行骨刮除处理,使用股骨双动头假体的尺寸通常较小,这导致聚乙烯内衬的厚度趋于最小化;而随着聚乙烯厚度降低,其内部的剪切应力会增加,导致磨损加速。SAITO等[25]认为,假体内分离并非由锁定机制失效引起,而是由于内衬较薄以及假体设计不当的缘故,使内衬和金属壳之间出现间隙所导致的。因此,GEORGIOU等[30]认为,为了保证聚乙烯内衬足够的耐磨性和内部剪切应力最小化,聚乙烯内衬的最小厚度应该是6或8 mm,并使用直径为22 mm的股骨头。值得注意的是,与聚乙烯内衬相比,金属衬垫的发生假体内分离的概率较低[23]。但也有研究指出,假体内分离与假体内衬的类型或材料、组件的定位准确度无关[4,54-55]。 此外,URU?等[56]报道了3例双动半髋关节置换术后发生假体内分离患者,X射线片检查显示双动头假体呈过度内翻位。作者认为,假体的设计缺陷会导致双动头股骨假体组件之间的中心位置发生偏移,尤其在外翻位置插入并固定股骨假体时或者髋臼外上缘因骨关节炎存在大量骨赘时,股骨大头假体常呈过度内翻位,此时,聚乙烯衬垫的外上侧会承受过度应力,且股骨颈与聚乙烯内衬的下部之间易发生撞击,最终由于锁定机制损坏而导致假体内分离的发生[14,56]。HASEGAWA等[19]将半髋关节假体分离分为3种类型:Ⅰ型,锁定环脱离至股骨颈处,但金属股骨小头未脱离;Ⅱ型,锁定环脱离至股骨颈处,金属股骨小头与大头脱离,股骨大头在髋臼内呈过度内翻位;Ⅲ型,锁定环未脱位,股骨大头在髋臼内呈过度内翻位,股骨小头与大头脱离,见图9。因此,为了克服这个问题,双动头股骨假体自定心系统应运而生,这种设计的优点在于:一是极点偏移,即通过在运动时产生一种自中心的扭矩,改变股骨小头的中心点,使其自动校正至股骨大头中心的位置,从而防止股骨大头过度内翻[57];二是自动校正力,即通过在活动和承载负荷时产生的扭矩,以维持双动关节组件之间的精准匹配,防止中心位置发生过度偏移[56];三是减轻载荷,这种设计减轻了股骨头假体对软骨以及假体界面之间的负荷,从而延长假体使用寿命,并降低假体内分离发生的风险[19]。BARMADA等[58]、M?LLERS等[57]报道,应用自中心双极半髋假体术后发生概率均显著降低。总之,产品的设计优化、材质的改进以及制造过程的精准控制都是确保假体长期稳定的关键。"

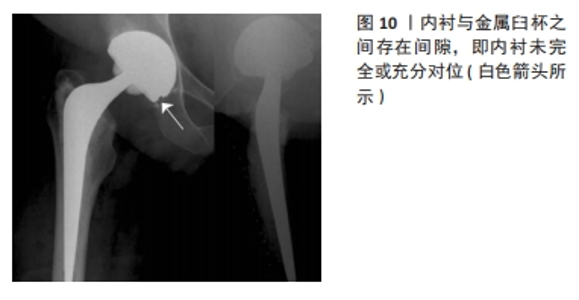
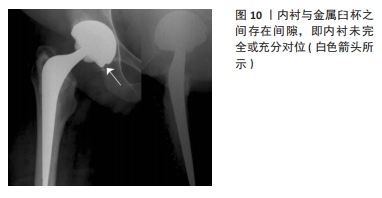
2.3.3 假体位置安装不当 髋关节置换手术的成功与否,很大程度上取决于外科医生技术的精良和假体安装的精确性。如在手术过程中未能正确安装髋臼组件,可能引发一系列问题,如撞击、内衬边缘过载及断裂,进而致使假体内分离的发生[4,8,51]。假体位置安装不当的情况包括两方面:①一方面是指未按照解剖学或生物力学的理想角度安放假体,造成髋臼组件的过度倾斜或旋转等。在髋关节置换术后发生假体内分离的患者中,有超过50%的病例存在假体位置安装不当致使过度外展的情况[6,28]。而WANG等[59]的研究显示,理想的髋白杯外展角和前倾角为40°-50°和10°-25°。②另一方面是指内衬未完全或充分对位,即衬垫没有被正确或充分安置到其对应的金属臼杯内部,见图10。术中如有软组织、骨碎片以及骨水泥碎片等因素的干扰,可能会导致假体组件间不充分对位及匹配[23]。有报道指出,约16.4%的假体内分离是由于衬垫未完全对位造成的[60]。因此,确保在放置内衬时充分可视化髋臼是至关重要的[24]。此外,术中操作失误的缘由,如内衬示模意外留在髋臼杯内,或假体组件型号不匹配等,也有可能导致假体内分离的发生[11,61]。BAEK等[22]认为假体位置安装不当导致假体内分离发生的原因,主要与金属杯的锁定机制失效和内衬未充分着位有关。钛制髋臼杯在打压置入过程中可能会产生可测量的形变,除对锁定装置造成一定的损伤外,还可能导致内衬安装不牢靠,甚至破裂[20,24]。"

髋臼杯缘锁定齿的完整性和臼杯-内衬间的完全匹配吻合是锁定机制成功起效的关键,一旦破损或丧失可能会增加假体内分离发生的风险[23,62]。GEORGIOU等[30]研究表明,对于髋关节置换患者,选择不恰当的假体型号、假体组件间对位不匹配和髋臼杯的长期侵蚀,进而造成锁定机制的失效和假体内分离并发症的发生。有报道,1例全髋关节置换患者在术后1年发现有髋臼金属杯缘锁定齿断裂的现象,术后6年发生了假体内分离并发症[25]。SINGLETON等[23]报告的4例假体内分离中,位于髋臼杯上方的3个锁定齿发生了断裂。总之,保持髋臼杯锁定装置的完整性和假体组件间的精准对位,是确保假体组件锁定机制发挥长期、安全有效作用的重要保障[4]。 2.3.4 医源性分离 对于双动半髋关节置换术后的患者,医源性假体内分离是一个常见的并发症。当双动头半髋假体整体发生脱位时,常被弹性固定于髋臼后壁。如进行闭合复位操作,髋臼杯的卡环将受到强大的扭转力[30],在髋臼后缘充当支点的作用下,使得双极杯发生翻转,同时出现聚乙烯锁定环断裂,从而导致假体内分离的发生。此时,金属股骨大头假体仍滞留在髋臼外,而金属股骨小头假体复位至髋臼中[56,63],这也被称作“开瓶器效应”,见图11。此并发症通常在双动半髋关节置换术后几周至几个月出现。URU?等[56]和BIAN等[64]分别报道,双动半髋关节置换术后分别有40%和75%发生假体内分离的患者属于医源性分离。同样,也有其他文献对双动半髋关节置换术后发生医源性假体内分离并发症进行了相应报道[1,30]。此外,有研究报道,对55例发生早期假体脱位的患者进行手法复位过程中,有7例(13%)发生了双动头假体内分离,其中6例假体为单一聚乙烯锁定环的锁定机制设计。作者认为,双动半髋关节置换术后出现医源性假体内分离的并发症,与使用单一聚乙烯锁定环有关,因此不推荐使用此种锁定机制的假体[65]。"

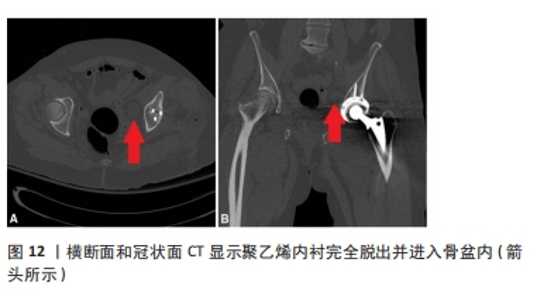
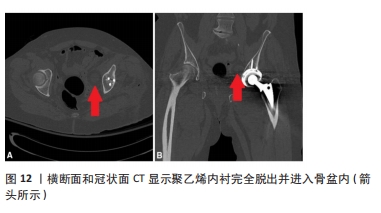
2.4 假体内分离的治疗策略 对于全髋关节置换术后发生假体内分离的患者,考虑到假体组件固定的稳定性和是否撞击等情况,应采取个体化治疗原则[66]。正如GONZáLEZ DELLA VALLE等[61]研究报道,采取多种方法,如更换壳体、更换衬垫、将替换的衬垫用水泥固定至金属臼杯内以及使用骨水泥固定全聚乙烯杯等,治疗18例全髋关节置换术后发生假体内分离的患者,均取得令人满意的疗效。SAITO等[25]和LAPORTE等[67]认为,当金属臼杯假体锁定机制出现故障、术中发现金属臼杯错位或衬垫尺寸不匹配时,可更换比金属臼杯直径小4 mm的聚乙烯内衬,并用骨水泥将衬垫黏合到完好的金属髋臼假体中。有生物力学研究表明,骨水泥黏合内衬足以承受髋关节模拟器施加的载荷,比一些锁定机制固定假体组件更稳定、更可靠[34]。在CIOLLI等[4]的研究中,仅有39.5%的髋臼杯假体和8.8%的股骨柄假体需要进行翻修;然而,即使金属臼杯锁定机制未受损,在更换聚乙烯内衬后,固定内衬的稳定性也会减弱25%[25]。因此,有作者建议需要对多孔涂层髋臼组件进行整体翻修,以降低假体内分离再次发生的可能性[4]。也有作者认为,早期假体内分离可行单纯聚乙烯内衬或金属股骨头假体更换,而晚期假体内分离则需要进行金属臼杯的翻修[26]。同时,在翻修时应充分重视对髋臼骨量缺失的问题的解决[68]。此外,如遇到聚乙烯内衬脱出并进入骨盆内的罕见情况时,治疗上应在修复髋臼并矫正其不稳定性的同时,评估骨盆内聚乙烯衬垫取留的风险性,充分权衡利弊后再进行下一步处理[15],见图12。"
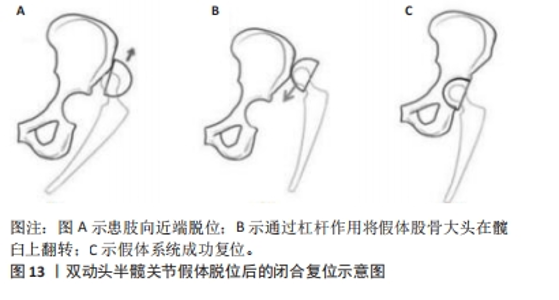
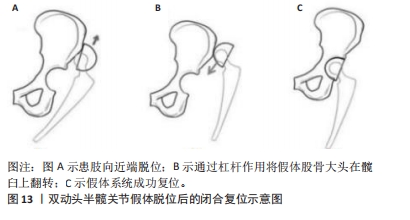
对于双动半髋关节置换术后发生假体内分离的患者,目前临床上的处理包括单纯的更换内衬和全部髋关节假体更换。PERKINS等[9]认为,单纯的内衬更换后易再次复发,原因在于:假体组件不匹配、锁定机制已破坏等因素可直接导致假体磨损加速及假体内分离的再次发生。因此,建议更换全部髋关节假体更为合适。而SAINI等[1]则指出,对于模块化双动头假体,允许单纯的部分组件更换。而对于一体式非模块化双动头假体,由于其特有的锁定机制,则需要全部组件的整体更换。需要强调的是,在假体翻修过程中,应特别注意对组件间的精确匹配,保持假体的稳定性及髂腰肌和短外旋肌的完整性,以确保假体水平和垂直偏心距的完美恢复。 对于双动半髋关节置换术后假体脱位的闭合复位,BARRACK等[11]建议使用局部麻醉或全身麻醉而不是静脉镇静,由于其可减少复位所需要的牵拉力量,从而可能会避免发生医源性假体内分离。此外,BIAN等[64]建议在X射线透视下对双动头半髋关节假体进行闭合复位,首先将患侧肢体向近端移动,同时进行内旋和内收,利用杠杆作用将金属股骨大头假体翻转至髋臼上方,使得其凸面而非边缘部与髋骨接触,以提高双动头假体复位的成功率,并降低医源性假体内分离的发生概率,见图13。"
| [1] SAINI MK, REDDY NR, REDDY PJ. Disassembly of components of a monoblock bipolar hip prosthesis following Dislocation: a case report and review on “bottle opener effect”. J Orthop Case Rep. 2020;10(9): 90-93. [2] KAGAN R, ANDERSON MB, PETERS C, et al. Pinnacle polyethylene liner dissociation: a report of 3 cases. Arthroplast Today. 2018;4(4):441-446. [3] GWYNNE-JONES DP, MEMON A. Acetabular liner dissociation: a comparative study of two contemporary uncemented acetabular components. Arthroplast Today. 2020;6(3):354-359. [4] CIOLLI G, SILVA R, GIOVANNETTI DSE, et al. Liner dissociation in total hip arthroplasty: a systematic review. Eur Rev Med Pharmacol Sci. 2022;26(1 Suppl):138-150. [5] WASEEM S, FONG D, ONSA M, et al. Dual mobility total hip replacements in young patients- a systematic review. Indian J Orthop. 2023;57(2):203-210. [6] NAPIER RJ, DIAMOND O, O’NEILL C, et al. The incidence of dissociated liners in 4,751 consecutive total hip arthroplasties using Pinnacle polyethylene acetabular liners. Hip Int. 2017;27(6):537-545. [7] KAWANO S, SONOHATA M, KITAJIMA M, et al. Highly cross-linked polyethylene liner dissociation from a cement-less modular acetabular shell: two Case Reports. Open Orthop J. 2016;10:732-740. [8] YUN A, KOLI EN, MORELAND J, et al. Polyethylene liner dissociation is a complication of the depuy pinnacle Cup: a report of 23 Cases. Clin Orthop Relat Res. 2016;474(2):441-446. [9] PERKINS TJ, KOP AM, WHITEWOOD C, et al. Dissociation of polyethylene liners with the depuy pinnacle cup: a report of 26 cases. Hip Int. 2023;33(1):28-33. [10] CIRIELLO V, LA CHINA R, CHIRILLO DF, et al. Is modular dual mobility superior to standard bearings for reducing dislocation risk after primary total hip arthroplasty? A retrospective comparative multicenter study. J Clin Med. 2023;12(13):4200. [11] BARRACK RL, BURKE DW, COOK SD, et al. Complications related to modularity of total hip components. J Bone Joint Surg Br. 1993;75(5): 688-692. [12] LI L, REN J, LIU J, et al. What are the risk factors for dislocation of Hip bipolar hemiarthroplasty through the anterolateral approach? A nested case-control study. Clin Orthop Relat Res. 2016;474(12):2622-2629. [13] ELLANTI P, BAHARI S, MCCARTHY T. Significantly displaced femoral head component in a dissociated bipolar hip hemiarthroplasty. Orthop Surg. 2012;4(3):194-196. [14] SEVINÇ HF. Dissociation of bipolar components following bipolar hemiarthroplasty: a report of two different cases and review of the literature. Ulus Travma Acil Cerrahi Derg. 2021;27(5):600-603. [15] FEHRING KA, BERRY DJ. Dissociation and intrapelvic entrapment of a dual-mobility polyethylene component. Clin Orthop Relat Res. 2016;474(4):1072-1076. [16] JAMESON SS, BAKER PN, MASON J, et al. Independent predictors of failure up to 7.5 years after 35 386 single-brand cementless total hip replacements: a retrospective cohort study using national joint registry data. Bone Joint J. 2013;95-B(6):747-757. [17] YANG Y, FU G, LI Q, et al. Multivariable analysis of risk factors affecting dislocation after bipolar hemiarthroplasty in patients with femoral neck fracture. Ther Clin Risk Manag. 2022;18:101-111. [18] 郑昱新, 汤荣光. 全髋置换术后聚乙烯内衬与金属壳分离[J]. 临床骨科杂志,2001(1):77-78. [19] HASEGAWA M, SUDO A, UCHIDA A. Disassembly of bipolar cup with self-centering system: a report of seven cases Clin Orthop Relat Res. 2004;(425):163-167. [20] KOSTRETZIS L, MARTINOV S, LAVIGNE M, et al. Liner dissociation in a large-diameter ceramic-bearing acetabular component: a report of five cases. BMC Musculoskelet Disord. 2022;23(1):136. [21] PHILIPPOT R, BOYER B, FARIZON F. Intraprosthetic dislocation: a specific complication of the dual-mobility system. Clin Orthop Relat Res. 2013; 471(3):965-970. [22] BAEK SH, KIM JY, HAN JW, et al. Potential risk of AMC ceramic liner for dissociation after square seating. J Orthop Sci. 2018;23(3):600-603. [23] NEAL S. Polyethylene liner dissociation with the depuy pinnacle cup: a report of 6 cases. Orthop Res Online. 2018;3:293. [24] SHNAEKEL AW, MAYES WH, STAMBOUGH JB, et al. dissociation of acetabular polyethylene liners with a morse taper design. J Arthroplasty. 2020;35(12):3754-3757. [25] SAITO S, RYU J, SEKI M, et al. Analysis and results of dissociation of the polyethylene liner in the harris-galante I acetabular component. J Arthroplasty. 2008;23(4):522-526. [26] 刘新, 李卫国. 人工髋关节置换术后脱位及内衬分离的原因和防治[J]. 中国骨与关节损伤杂志,2008,23(2):107-109. [27] MEMON AR, GWYNNE-JONES D. Polyethylene liner dissociation with the Pinnacle acetabular component: should we be concerned? Arthroplast Today. 2020;6(1):5-8. [28] GRAY CF, MOORE RE, LEE GC. Spontaneous dissociation of offset, face-changing polyethylene liners from the acetabular shell: a report of four cases. J Bone Joint Surg Am. 2012;94(9):841-845. [29] MAYER SW, WELLMAN SS, BOLOGNESI MP, et al. Late liner disassociation of a Pinnacle system acetabular component. Orthopedics. 2012;35(4):e561-e565. [30] GEORGIOU G, SIAPKARA A, DIMITRAKOPOULOU A, et al. Dissociation of bipolar hemiarthroplasty of the hip after dislocation. A report of five different cases and review of literature. Injury. 2006;37(2):162-168. [31] SU EP, CALLANDER PW, SALVATI EA. The bubble sign: a new radiographic sign in total hip arthroplasty. J Arthroplasty. 2003;18(1):110-112. [32] ENDO Y, GEANNETTE C, CHANG WT. Imaging evaluation of polyethylene liner dissociation in total hip arthroplasty. Skeletal Radiol. 2019;48(12):1933-1939. [33] BEDARD NA, TETREAULT MW, HANSSEN AD, et al. Intermediate to long-term follow-up of cementing liners into well-fixed acetabular components. J Bone Joint Surg Am. 2020;102(16):1397-1404. [34] CHAUHAN A, FITZPATRICK S, SCIULLI RL, et al. Using double-contrast CT arthrography to confirm suspected dissociation of a cemented polyethylene liner in the setting of revision total hip arthroplasty: a case report. JBJS Case Connect. 2017;7(2):e34. [35] USREY MM, NOBLE PC, RUDNER LJ, et al. Does neck/liner impingement increase wear of ultrahigh-molecular-weight polyethylene liners? J Arthroplasty. 2006;21(6 Suppl 2):65-71. [36] SHON WY, BALDINI T, PETERSON MG, et al. Impingement in total hip arthroplasty a study of retrieved acetabular components. J Arthroplasty. 2005;20(4):427-435. [37] ISAAC GH, WROBLEWSKI BM, ATKINSON JR, et al. A tribological study of retrieved hip prostheses. Clin Orthop Relat Res. 1992;(276):115-125. [38] 张海林, 翁文杰, 袁涛, 等. Harris-Galante Ⅱ型髋臼假体与聚乙烯内衬分离1例报告[J]. 中国矫形外科杂志,2009,17(3):236-237. [39] 黄野, 张洪, 周乙雄. Harris-GalanteⅡ组配型髋臼的内衬脱落二例报告[J]. 中华骨科杂志,2003(4):62-63. [40] ITO H, MATSUNO T, KANEDA K. Bipolar hemiarthroplasty for osteonecrosis of the femoral head. A 7- to 18-year followup. Clin Orthop Relat Res. 2000;(374):201-211. [41] YAMAGUCHI M, AKISUE T, BAUER TW, et al. The spatial location of impingement in total hip arthroplasty. J Arthroplasty. 2000;15(3):305-313. [42] HABE Y, HAMADA H, UEMURA K, et al. Cup safe zone and optimal stem anteversion in total hip arthroplasty for patients with highly required range of motion. J Orthop Res. 2024;42(6):1283-1291. [43] 郭卓涛, 张凯, 查国春, 等. 腰椎融合对全髋关节置换后中期疗效影响的匹配对照试验[J]. 中国组织工程研究,2023,27(36):5801-5805. [44] MALIK A, DORR LD, LONG WT. Impingement as a mechanism of dissociation of a metasul metal-on-metal liner. J Arthroplasty. 2009; 24(2):313-323. [45] HEMMILÄ M, KARVONEN M, LAAKSONEN I, et al. Survival of 11,390 continuum cups in primary total hip arthroplasty based on data from the Finnish Arthroplasty Register. Acta Orthopaedica. 2019;90(4): 312-317. [46] AYORA A, GONZALEZ G, FERNANDEZ C. A polyethylene liner dissociation case report in depuy pinnacle cup. An impingement problem? Arch Clin Exp Surg (ACES). 2019:1. [47] TSIKANDYLAKIS G, OVERGAARD S, ZAGRA L, et al. Global diversity in bearings in primary THA. EFORT Open Rev. 2020;5(10):763-775. [48] TSIKANDYLAKIS G, MOHADDES M, CNUDDE P, et al. Head size in primary total hip arthroplasty. EFORT Open Rev. 2018;3(5):225-231. [49] JALALI O, SCUDDAY T, FICKENSCHER MC, et al. Third-Generation medium cross-linked polyethylene demonstrates very low wear in total hip arthroplasty. Arthroplast Today. 2020;6(3):316-321. [50] PAGANO S, PLATE JF, KAPPENSCHNEIDER T, et al. Polyethylene liner dissociation in total hip arthroplasty: a retrospective case-control study on a single implant design. J Orthop Traumatol. 2024;25(1):38. [51] GOYAL P, HOWARD JL, YUAN X, et al. Effect of Acetabular Position on polyethylene liner wear measured using simultaneous biplanar acquisition. J Arthroplasty. 2017;32(5):1670-1674. [52] FRANSEN BL, BENGOA FJ, NEUFELD ME, et al. Thin highly cross-linked polyethylene liners combined with large femoral heads in primary total hip arthroplasty show excellent survival and low wear rates at a mean follow-up of 12.8 years. Bone Joint J. 2023;105-B(1):29-34. [53] YEE MA, O’KEEFE TJ, WINTER S. Incarcerated fracture fragments of longevity polyethylene liners after total hip arthroplasty. Arthroplasty Today. 2016;2(1):6-10. [54] SARACCO M, PASSIATORE M, CAZZATO G, et al. Use of ceramic bearings in hip arthroplasty: correct implantation and review of clinical and radiographic results. J Biol Regul Homeost Agents. 2020;34(4 Suppl. 3): 237-242. [55] LEWINNEK GE, LEWIS JL, TARR R, et al. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217-220. [56] URUÇ V, ÖZDEN R, DUMAN IG, et al. Five cases of early dissociation between the bipolar hip endoprosthesis cup components; either spontaneously or during reduction maneuvers. Acta Orthop Traumatol Turc. 2017;51(2):172-176. [57] MÖLLERS M, STEDTFELD HW, PAECHTNER S, et al. Hemi-arthroplasty of the hip joint: concentric or positive eccentric (self-centering) dual head prosthesis? A retrospective comparison. Unfallchirurg. 1992;95(5): 224-229. [58] BARMADA R, MESS D. Bateman hemiarthroplasty component disassembly. A report of three cases of high-density polyethylene failure. Clin Orthop Relat Res. 1987;(224):147-149. [59] WANG XD, LAN H, HU ZX, et al. SuperPATH minimally invasive approach to total hip arthroplasty of femoral neck fractures in the elderly: preliminary clinical results. Orthop Surg. 2020;12(1):74-85. [60] LANGDOWN AJ, PICKARD RJ, HOBBS CM, et al. Incomplete seating of the liner with the trident acetabular system: a cause for concern? J Bone Joint Surg Br. 2007;89(3):291-295. [61] GONZÁLEZ DELLA VALLE A, RUZO PS, LI S, et al. Dislodgment of polyethylene liners in first and second-generation harris-galante acetabular components. A report of eighteen cases. J Bone Joint Surg Am. 2001;83(4):553-559. [62] HAN CD, CHOE WS, YOO JH. Late dissociation of the polyethylene liner from a modular acetabular metal shell after primary total hip arthroplasty--a report of five cases. Yonsei Med J. 1998;39(3):277-282. [63] VASILEIOS A, SPYRIDON P. Dissociation of bipolar hemiarthroplasty of the Hip and review of literature. Arthroplast Today. 2022;16:119-123. [64] BIAN YY, WANG LC, XIAO K, et al. Hip dislocation and femoral component disassembly after bipolar hemiarthroplasty: a report of four cases and introduction of new reduction maneuvers. Chin Med J (Engl). 2019;132(3):370-372. [65] SIM SB, SON SW, SHIM BJ. Be aware of the “O” sign in the bipolar cup dissociation during closed reduction of bipolar dislocation: a case report. Medicine (Baltimore). 2023;102(37):e35234. [66] 王上增, 王禛, 游明灿, 等.人工股骨头置换后的髋臼磨损:原因和处理[J]. 中国组织工程研究,2023,27(13):2028-2032. [67] LAPORTE DM, MONT MA, PIERRE-JACQUES H, et al. Technique for acetabular liner revision in a nonmodular metal-backed component. J Arthroplasty. 1998;13(3):348-350. [68] WERLE J, GOODMAN S, SCHURMAN D, et al. Polyethylene liner dissociation in harris-galante acetabular components: a report of 7 cases. J Arthroplasty. 2002;17(1):78-81. |
| [1] | Wang Lei, Li Chengsong, Zhang Shenshen, Wang Qing. Finite element analysis of biomechanical characteristics of three internal fixation methods in treatment of inferior patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7048-7054. |
| [2] | Wang Rongqiang, Yang Liu, Wu Xiangkun, Shang Lilin. Analysis of factors associated with prognosis of osteoporosis patients after hip arthroplasty and construction of Nomogram prediction model [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7137-7142. |
| [3] | Abuduainijiang·Abulimiti, Alimu·Mamuti, Li Simi. Artificial femoral head replacement for femoral neck fracture in the elderly: validation of a risk prediction model for hip dysfunction [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7143-7149. |
| [4] | Yang Wanzhong, Ma Rong, Guo Wei, Wang Zhiqiang, Yang Wei, Chen Zhen, Wang Zemin, Zhang Honglai, Ge Zhaohui. One-stage posterior hemivertebra resection and pedicle screw fixation in treatment of congenital scoliosis: a 2-year follow-up of correction effect [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7173-7180. |
| [5] | Jiang Zehua, Du Wenjun, Ren Zhishuai, Cui Haojun, Zhu Rusen. Percutaneous vertebroplasty via Kambin's triangle for treatment of osteoporotic compression fractures: evaluation of safety and effectiveness [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7181-7188. |
| [6] | Yan Jinlian, Xu Zhengquan, Wei Renjie, Wang Yehua. Hip joint function recovery and prediction model construction after proximal femoral nail antirotation for intertrochanteric fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7189-7195. |
| [7] | Cao Yong, Li Xin, Chen Zhigang, Gu Honglin, Lyu Shujun. Compensatory alignment changes of cervical and thoracic spine after correction of lumbar degenerative scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7196-7202. |
| [8] | Liang Jiachang, Guan Hua, Feng Enhui, Chen Pu, Huang Weiming, He Jianbo, Xie Jiewei. Ilizarov technique for treatment of congenital brachymetatarsia of the fourth: subgroup analysis of prolongation ratio [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7217-7222. |
| [9] | Pan Hongyu, Li Hongtao, Xiao Changming, Li Sen. Biomechanical analysis on treatment of different types of osteoporotic vertebral compression fractures with individualized precise puncture vertebral augmentation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5773-5784. |
| [10] | Chen Zhen, Chen Xi, Li Xiaoting, Chen Daxin, Hong Weiwu. Comparison of medial-lateral and lateral-only fixation for pediatric supracondylar humeral fractures: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5924-5932. |
| [11] | Wang Yijun, Zheng Kai, Zhang Lianfang, Zhu Feng, Zhang Weicheng, Li Rongqun, Zhou Jun, Xu Yaozeng. Navigation-assisted total knee arthroplasty using functional alignment restores constitutional alignment and joint line obliquity [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5810-5818. |
| [12] | Tu Zesong, Xu Daxing, Luo Hongbin, Wang Yusheng, Feng Xinglun, Peng Zhonghua, Du Shaolong. Construction of a risk prediction model for failure of proximal femoral nail antirotation fixation in intertrochanteric fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5845-5853. |
| [13] |
Wang Qianliang, Zhang Qianzhongyi, Peng Yujian, Yan Jun.
Effects of unilateral biportal endoscopic transforaminal lumbar interbody fusion on paraspinal muscles
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5862-5868.
|
| [14] | Pan Xian, Zhang Yuanjin, Zhang Guofu, Li Jun, Liu Bingxia, Zhou Dingkang, Sun Farui. Debridement, antibiotics, and implant retention combined with replacement of assembled components in treatment of acute prosthetic joint infection after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4499-4505. |
| [15] | Lyu Xiaodong, Gu Jinrui, Gao Jingyu, Ge Jianzhong. Total hip arthroplasty after failure of internal fixation for intertrochanteric fractures: model prediction of occult blood loss [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4506-4513. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||