Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (27): 5924-5932.doi: 10.12307/2025.826
Previous Articles Next Articles
Comparison of medial-lateral and lateral-only fixation for pediatric supracondylar humeral fractures: a systematic review and meta-analysis
Chen Zhen1, Chen Xi1, Li Xiaoting2, Chen Daxin1, Hong Weiwu1
- 1Department of Orthopedics of Traditional Chinese Medicine, 2Department of Acupuncture, Shantou Central Hospital, Shantou 515000, Guangdong Province, China
-
Received:2024-05-13Accepted:2024-07-26Online:2025-09-28Published:2025-03-07 -
Contact:Chen Zhen, MS, Attending physician, Department of Orthopedics of Traditional Chinese Medicine, Shantou Central Hospital, Shantou 515000, Guangdong Province, China -
About author:Chen Zhen, MS, Attending physician, Department of Orthopedics of Traditional Chinese Medicine, Shantou Central Hospital, Shantou 515000, Guangdong Province, China -
Supported by:Science and Technology Plan Medical and Health Category Project, No. 191220175263010 (to CZ)
CLC Number:
Cite this article
Chen Zhen, Chen Xi, Li Xiaoting, Chen Daxin, Hong Weiwu. Comparison of medial-lateral and lateral-only fixation for pediatric supracondylar humeral fractures: a systematic review and meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5924-5932.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

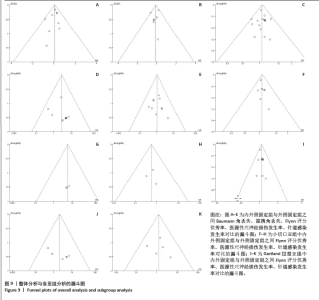
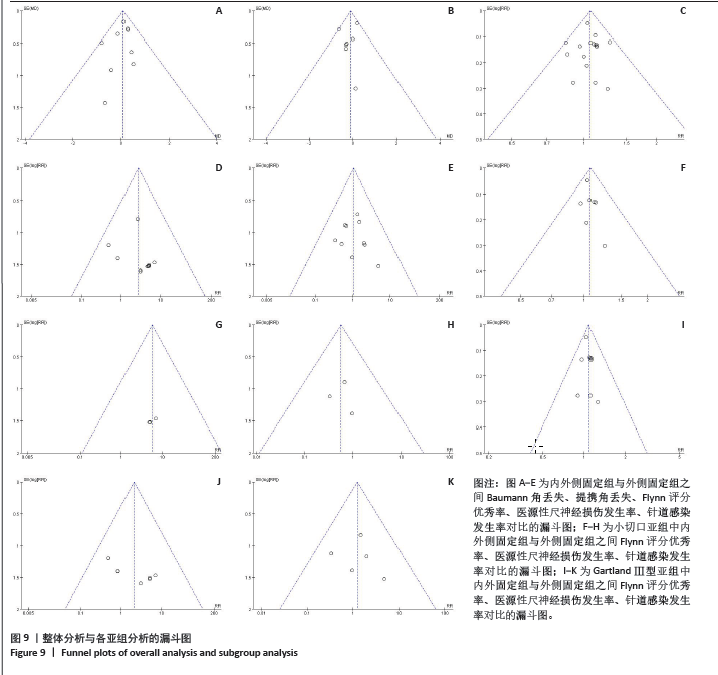
2.4 影像学检查的Meta分析结果 共有9项研究中报道了手术Baumann角丢失的情况[18-21,23-25,30-31],外侧固定组与内外侧固定组Baumann角丢失之间的差异无显著性意义(P=0.47),见图3。共有7项研究中报道了手术提携角丢失的情况[18-19,21,23-25,31],外侧固定组与内外侧固定组提携角丢失之间差异同样无显著性意义(P=0.47),见图4。 2.5 肘关节功能的Meta分析结果 共有16项研究根据Flynn评分标准对肘关节功能进行了评估[19-25,27-35]。在内外侧固定组中,74.9%(402/537)的患者报告了优秀的结果,这与外侧固定组的70.7%(389/550)结果类似,RR=1.06,95%CI:0.99-1.14,P=0.12,如图5所示。结果表明,在使用Flynn标准进行评估时,内外侧固定组与外侧固定组之间的肘关节功能恢复没有显著差异。"
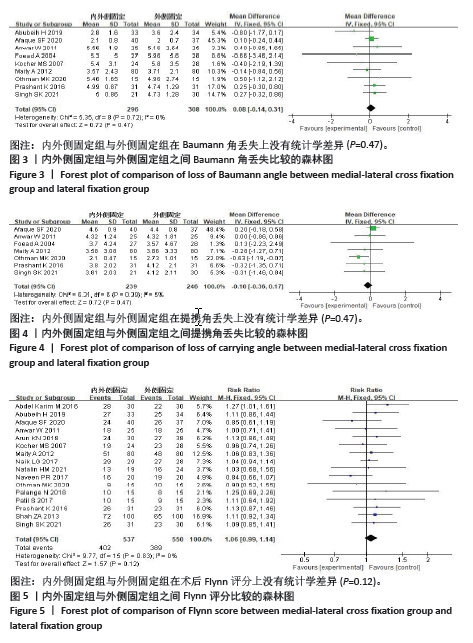
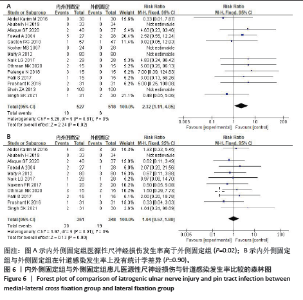
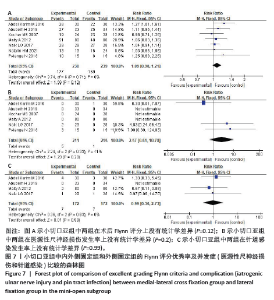
2.6 并发症的Meta分析结果 有14项研究中报道了医源性尺神经损伤的发生率[18,20-26,29-31,33-35],其中4项研究报告术中、术后并没有发生尺神经损伤[20,30-31,35]。在接受内外侧克氏针固定治疗的患者中,527例骨折中有19例出现尺神经损伤,发生率为3.6%;相比之下,518例外侧固定的患儿中只有6例发生了尺神经损伤,发生率为1.2%。内外侧固定组患儿医源性尺神经损伤发生率更高(P=0.02),如图6A所示。 此外,文章还分析了两组针道感染发生率的差异。在内外侧固定组中,针道感染发生率为5.7%(20/351),与外侧固定组的针道感染发生率5.5%(19/348)相比差异无显著性意义(RR=1.04,95%CI:0.57-1.89,P=0.90),如图6B所示。"

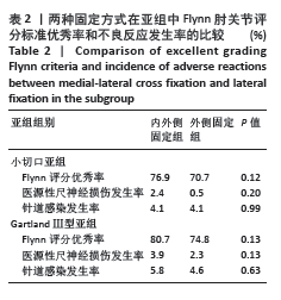
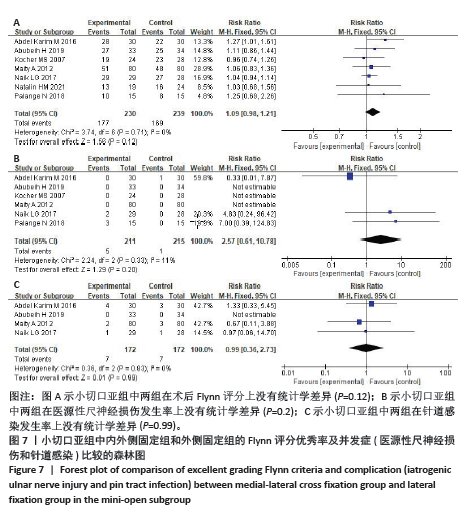
2.7 小切口亚组分析 文献报道采用术中小切口有可能降低手术不良反应的发生风险,因此进行了关于小切口技术的亚组分析,分析两种手术方式在功能恢复与不良反应发生率方面的差异,具体详见表2。 在使用小切口技术的两组固定方法中,内外侧固定组中76.9% (177/230)的患者报告了优秀的结果,略高于外侧固定组70.7%(169/239),但两组间差异无显著性意义(P=0.12),见图7A。 小切口亚组中,内外侧固定组中有2.4%(5/211)的患者发生了尺神经损伤,而外侧固定组为0.5%(1/215),但两组对比差异无显著性意义(P=0.2),见图7B。 内外侧固定组与外侧固定组的患儿针道感染发生率一致,均为4.1%,差异同样无显著性意义(P=0.99),见图7C。"
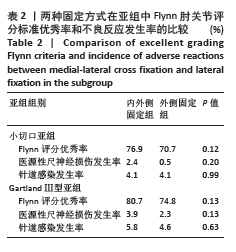
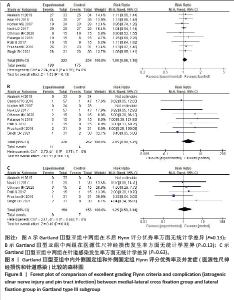
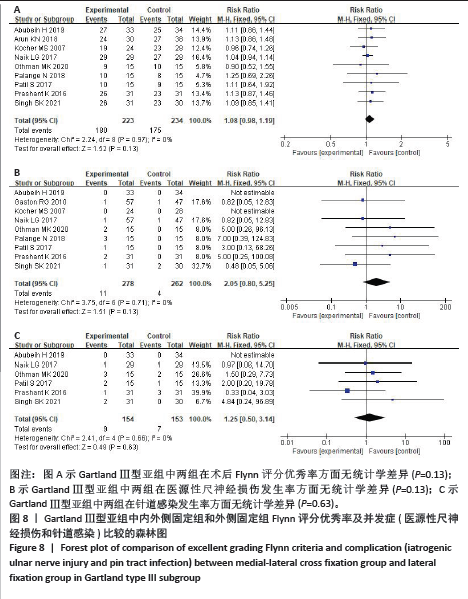
2.8 Gartland Ⅲ型的亚组分析 如表2所示,在只纳入Gartland Ⅲ型骨折的研究中,内外侧固定组80.7%(180/223)的患者报告了Flynn评分优秀的结果,高于外侧固定组的74.8%(175/234),但两组间差异无显著性意义(P=0.13),见图8A。 Gartland Ⅲ型亚组中,内外侧固定组中有3.9%(11/278)的患者发生了尺神经损伤,高于外侧固定组的2.3%(4/262),但两组对比差异无显著性意义(P=0.13),见图8B。内外侧固定组患儿针道感染发生率为5.8%(9/154),高于外侧固定组的4.6%(7/153),两组对比差异无显著性意义(P=0.63),见图8C。"
| [1] KHOSHBIN A, LEROUX T, WASSERSTEIN D, et al. The epidemiology of paediatric supracondylar fracture fixation: a population-based study. Injury. 2014;45(4): 701-708. [2] LI Y, WEI S, CANAVESE F, et al. Treatment and Outcome of Supracondylar Humeral Fractures in Children Over 10 Years of Age at the Time of Injury: A Review of 60 Cases. J Pediatr Orthop. 2024;44(7):e580-e587. [3] WANG Y, CHONG Q, ZHANG S, et al. Analysis of risk factors for failed closed reduction in pediatric Gartland Type III supracondylar humerus fracture. J Shoulder Elbow Surg. 2024;33(10):2279-2289. [4] SCHULTZ RJ, AMARAL JZ, BRIDGES CS, et al. Gartland classification concordance of supracondylar fractures among pediatric emergency medicine physicians, radiologists, and orthopedic surgeons. Pediatr Radiol. 2024;54(7):1180-1186. [5] FARROW L, ABLETT AD, MILLS L, et al. Early versus delayed surgery for paediatric supracondylar humeral fractures in the absence of vascular compromise: a systematic review and meta-analysis. Bone Joint J. 2018;100-B(12):1535-1541. [6] DE L, DURÁN D, DE L, et al. Supracondylar fractures of the humerus in children. Clin Orthop Relat Res. 2005;19(3):57-64. [7] ZHAO JG, WANG J, ZHANG P. Is Lateral Pin Fixation for Displaced Supracondylar Fractures of the Humerus Better Than Crossed Pins in Children? Clin Orthop Relat Res. 2013;471(9):2942-2953. [8] WORATANARAT P, ANGSANUNTSUKH C, RATTANASIRI S, et al. Meta-analysis of pinning in supracondylar fracture of the humerus in children. J Orthop Trauma. 2012;26(1):48-53. [9] NA Y, BAI R, ZHAO Z, et al. Comparison of lateral entry with crossed entry pinning for pediatric supracondylar humeral fractures: a meta-analysis. J Orthop Surg Res. 2018; 13(1):68. [10] DEKKER AE, KRIJNEN P, SCHIPPER IB. Results of crossed versus lateral entry K-wire fixation of displaced pediatric supracondylar humeral fractures: A systematic review and meta-analysis. Injury. 2016;47(11): 2391-2398. [11] OMID R, CHOI PD, SKAGGS DL. Supracondylar Humeral Fractures in Children. JBJS. 2008;90(5):1121-1132. [12] LEE KM, CHUNG CY, GWON DK, et al. Medial and lateral crossed pinning versus lateral pinning for supracondylar fractures of the humerus in children: decision analysis. J Pediatr Orthop. 2012;32(2): 131-138. [13] FREDJ AB, RBAI H, CHATBOURI F, et al. Clinical and radiographic outcomes after paediatric supracondylar humeral fractures treated with combined intramedullary and lateral wire fixation: our experience in fifty-one cases. Int Orthop. 2023;47(12):2901-2906. [14] MCINNES MDF, MOHER D, THOMBS BD, et al. Preferred Reporting Items for a Systematic Review and Meta-analysis of Diagnostic Test Accuracy Studies: The PRISMA-DTA Statement. JAMA. 2018; 319(4):388-396. [15] CALOGERO V, AULISA AG, CARERI S, et al. Evaluation of Gartland Classification, Baumann Angle and Anterior Humeral Line in Paediatrics Supracondylar Fractures: An Inter and Intra-Observer Reliability Study. J Clin Med. 2023;13(1):167. [16] FLYNN JC, MATTHEWS JG, BENOIT RL. Blind pinning of displaced supracon-dylar fractures of the humerus in children. Sixteen years’experience withlong-term follow-up, J Bone Jt Surg Am. 1974;56:263-272. [17] HIGGINS JP, ALTMAN DG, GØTZSCHE PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [18] FOEAD A, PENAFORT R, SAW A, et al. Comparison of two methods of percutaneous pin fixation in displaced supracondylar fractures of the humerus in children. J Orthop Surg (Hong Kong). 2004; 12(1):76-82. [19] ANWAR W, RAHMAN N, IQBAL MJ, et al. Comparison of the two methods of percutaneous k - wire fixation in displaced supracondylar fracture of humerus in children. J Postgrad Med Institute. 2011; 25(4):356-361. [20] ABUBEIH H, ADLY W, GAAFARY K, et al. Percutaneous cross-pinning versus two lateral entry pinning in Gartland type III pediatric supracondylar humerus fractures. Egypt Orthop J. 2019;54:52-61. [21] PRASHANT K, LAKHOTIA D, BHATTACHARYYA TD, et al. A comparative study of two percutaneous pinning techniques (lateral vs medial-lateral) for Gartland type III pediatric supracondylar fracture of the humerus. J Orthop Traumatol. 2016;17(3):223-229. [22] PATIL S, GAONKAR N, PANDEY P, et al. A comparative study of two percutaneous pinning techniques (Cross K wire vs Lateral K wire) for Gartland type III pediatric supracondylar fracture of the humerus. Med J. 2017;3(4):665-668. [23] OTHMAN MK HS. Percutanous crossed pinning versus twolateral pinning for treating supracondylar humeral fracture in children: comparative study. J Kirkuk Med Coll. 2020;8:64-77. [24] SK S, P S, SP G, et al. A comparative study ofcross pinning versus lateral pinning technique in the management ofcompletely displaced type-lll supra condylar humerus fracture in therural India children: a prospective study. J Orthop Traumatol Rehabil. 2021;13:122-128. [25] AFAQUE SF, SINGH A, MAHARJAN R, et al. Comparison of clinic-radiological outcome of cross pinning versus lateral pinning for displaced supracondylar fracture of humerus in children: A randomized controlled trial. J Clin Orthop Trauma. 2020; 11(2):259-263. [26] GASTON RG, CATES TB, DEVITO D, et al. Medial and lateral pin versus lateral-entry pin fixation for Type 3 supracondylar fractures in children: a prospective, surgeon-randomized study. J Pediatr Orthop. 2010; 30(8):799-806. [27] KN A, RAMACHANDRA K, VEERABHADRA J, et al. A prospective study of crossed versus lateral pinning for displaced extension-type supracondylar fractures of humerus. AkiNik Publications. 2018;4(4):737-740 [28] NAVEEN PR, CHAITANYA PR. A prospective study of crossed versus lateral only pinning in the treatment of displaced supracondylar fractures of the humerus in children. Med J. 2017;3(3):400-404. [29] ABDEL KARIM M, HOSNY A, NASEF ABDELATIF NM, et al. Crossed Wires Versus 2 Lateral Wires in Management of Supracondylar Fracture of the Humerus in Children in the Hands of Junior Trainees. J Orthop Trauma. 2016;30(4):e123-e128. [30] KOCHER MS, KASSER JR, WATERS PM, et al. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. A randomized clinical trial. J Bone Jt Surg Am. 2007;89:706-712. [31] MAITY A, SAHA D, ROY DS. A prospective randomised, controlled clinical trial comparing medial and lateral entry pinning with lateral entry pinning for percutaneous fixation of displaced extension type supracondylar fractures of the humerus in children. J Orthop Surg Res. 2012;7:6. [32] NATALIN HM, SILVA J, VOLPON JB. Comparison of two methods of fixation of supracondylar fractures of the humerus in children. Acta Ortop Bras. 2021;29(5): 263-267. [33] PALANGE ND, GS P, MANE A, et al. A comparison between percutaneous cross k wire vs lateral k wires fixation in management of Type III Gartland paediatric supracondylar fractures. Med J. 2019;5(2): 119-122. [34] NAIK LG, SHARMA GM, BADGIRE KS, et al. Cross pinning versus lateral pinning in the management of type III supracondylar humerus fractures in children. J Clin Diagn Res. 2017;11:RC01-3. [35] ZA S, U A. Displaced supracondylar humeral fractures; treatment among children: crossed versus lateral pinning. Prof Med J. 2013;20:818-824. [36] BABAL JC, MEHLMAN CT, KLEIN G. Nerve injuries associated with pediatric supracondylar humeral fractures: a meta-analysis. Journal of Pediatric Orthopaedics. 2010;30(3):253-263. [37] PAVONE V, VESCIO A, RICCIOLI M, et al. Is Supine Position Superior to Prone Position in the Surgical Pinning of Supracondylar Humerus Fracture in Children? J Funct Morphol Kinesiol. 2020;5(3):57. [38] GONG HS, CHUNG MS, OH JH, et al. Oblique closing wedge osteotomy and lateral plating for cubitus varus in adults. Clin Orthop Relat Res. 2008;466(4):899-906. [39] REES AB, SCHULTZ JD, WOLLENMAN LC, et al. A Mini-Open Approach to Medial Pinning in Pediatric Supracondylar Humeral Fractures May Be Safer Than Previously Thought. J Bone Joint Surg Am. 2022;104(1):33-40. [40] PATRIOTA GSQA, ASSUNÇÃO FILHO CA, ASSUNÇÃO CA. What is the best fixation technique for the treatment of supracondylar humerus fractures in children? Rev Bras Ortop. 2017;52(4): 428-434. [41] KWOK SM, CLAYWORTH C, NARA N. Lateral versus cross pinning in paediatric supracondylar humerus fractures: a meta analysis of randomized control trials. ANZ J Surg. 2021;91(5):980-985. [42] CHEN C, ZHANG Y, CHEN H, et al. The effects of postoperative malrotation alignment on outcomes of Gartland type III/IV paediatric supracondylar humeral fractures treated by close reduction and percutaneous K-wire fixation. J Orthop Surg Res. 2024;19(1):26. [43] GREVE F, BIBERTHALER P, CASTELLANI C, et al. Beneficial Perioperative Aspects Favor the Use of Percutaneous Crossed Pinning over Antegrade Nailing in Pediatric Supracondylar Fractures-A Retrospective Comparative Study. Children (Basel). 2023; 10(5):830. |
| [1] | Zhang Xinxin, Gao Ke, Xie Shidong, Tuo Haowen, Jing Feiyue, Liu Weiguo. Network meta-analysis of non-surgical treatments for foot and ankle ability and dynamic balance in patients with chronic ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1931-1944. |
| [2] | Sun Yundi, Cheng Lulu, Wan Haili, Chang Ying, Xiong Wenjuan, Xia Yuan. Effect of neuromuscular exercise for knee osteoarthritis pain and function: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1945-1952. |
| [3] | Wang Yida, Liu Jun, Wang Xiaoling, Wang Liyan, Yang Chengru, Zhang Xuexiao. Effects of wearable electronic device-based interventions on physical activity and sedentary behavior in healthy adolescents: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1693-1704. |
| [4] | Zhang Zixian, Xu Youliang, Wu Shaokui, Wang Xiangying. Effects of blood flow restriction training combined with resistance training on muscle indicators in college athletes: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1705-1713. |
| [5] | Wang Juan, Wang Guanglan, Zuo Huiwu. Efficacy of exercise therapy in the treatment of anterior cruciate ligament reconstruction patients: #br# a network meta-analysis #br# [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1714-1726. |
| [6] | Zheng Huakun, Yin Mingyue, Liu Qian. Effects of interval and continuous training on the quality of life in physically inactive adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1727-1740. |
| [7] | Li Zhe, Li Ping, Zhang Chao, Guo Guangling. A network meta-analysis of efficacy of mesenchymal stem cells from different sources in treatment of premature ovarian failure animal models [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7898-7908. |
| [8] | Wang Kaigang, Hao Dongsheng, Ma Pei, Zhou Shuo, Li Ruimin. Comparison of efficacy of different biological scaffolds for pulp regeneration therapy in immature permanent teeth: a Bayesian network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7447-7460. |
| [9] | Wang He, Yu Shaohong, . Meta-analysis of transcranial direct current stimulation in improving lower limb motor dysfunction in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6556-6565. |
| [10] | Wang Jianlei, He Peiliang, Sun Yongjian. A meta-analysis of clinical efficacy and safety of intravenous glucocorticoids before lower limb joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 599-607. |
| [11] | Li Jia, Liu Qianru, Xing Mengnan, Chen Bo, Jiao Wei, Meng Zhaoxiang. A network meta-analysis on therapeutic effect of different types of exercise on knee osteoarthritis patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 609-616. |
| [12] | Zhou Yanjie, Cao Chunfeng, Zhang Zhongzu, Niu Xiong, Wang Xin, Yang Zaihai, Zhou Liang, Li Bo. Meta-analysis of anterior cervical decompression and fusion ROI-CTM self-locking system in treatment of degenerative cervical spondylosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 617-627. |
| [13] | Jiang Siqi, Huang Huanhuan, Yu Xinyu, Peng Ying, Zhou Wei, Zhao Qinghua. Meta-analysis of dose-effect of exercise on improving muscle health in community-dwelling older adults with sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6295-6304. |
| [14] | Yu Bingbing, Wang Tingting, Fang Junlin, Guo Yun, Huang Yingru. Acupuncture for treatment of postmenopausal osteoporosis: meta-analysis, systematic evaluation and trial sequential analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6305-6316. |
| [15] | Wang Jinfu, Yang Guan. Meta-analysis of wearable device interventions to promote physical activity in older adults [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(28): 6146-6160. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||