Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (27): 5862-5868.doi: 10.12307/2025.831
Previous Articles Next Articles
Effects of unilateral biportal endoscopic transforaminal lumbar interbody fusion on paraspinal muscles
Wang Qianliang, Zhang Qianzhongyi, Peng Yujian, Yan Jun
- Department of Orthopedics, Second Affiliated Hospital of Soochow University, Suzhou 215004, Jiangsu Province, China
-
Received:2024-05-28Accepted:2024-08-21Online:2025-09-28Published:2025-03-06 -
Contact:Yan Jun, MD, Chief physician, Department of Orthopedics, Second Affiliated Hospital of Soochow University, Suzhou 215004, Jiangsu Province, China -
About author:Wang Qianliang, MS, Attending physician, Department of Orthopedics, Second Affiliated Hospital of Soochow University, Suzhou 215004, Jiangsu Province, China -
Supported by:National Natural Science Foundation of China, No. 81971036 (to YJ)
CLC Number:
Cite this article
Wang Qianliang, Zhang Qianzhongyi, Peng Yujian, Yan Jun.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
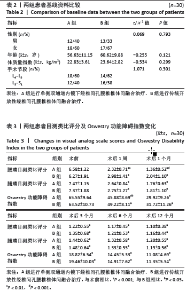
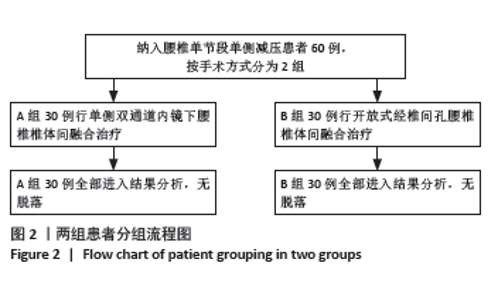
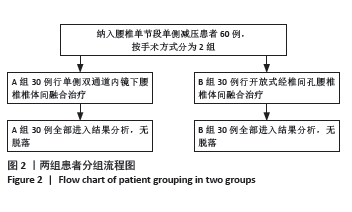
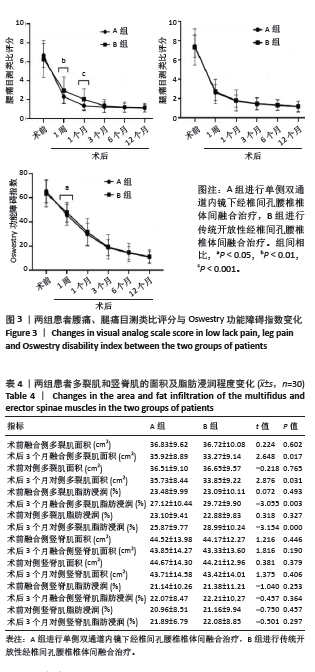
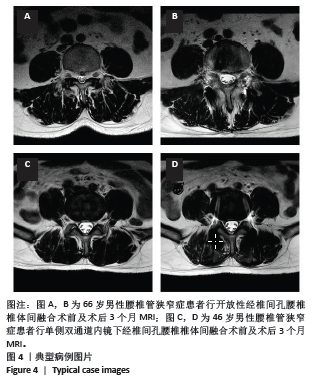
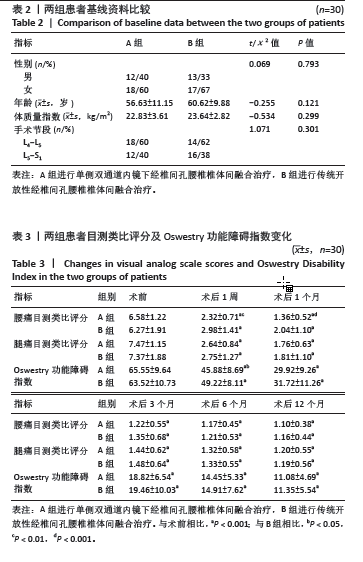
2.3 基线资料比较 两组患者性别分布、年龄、体质量指数及手术节段相比,差异均无显著性意义(P > 0.05),具有可比性,见表2。 2.4 效果或结局分析 2.4.1 目测类比评分及Oswestry 功能障碍指数 见表3。 两组术后各时间点腰部目测类比评分较术前均明显下降(P < 0.001,P < 0.001)。术前腰部目测类比评分无明显组间差异(P=0.895),术后1周及术后1个月,A组患者腰部目测类比评分低于B组(P < 0.01,P < 0.001),而术后3,6,12个月随访中两组患者腰部目测类比评分均无明显差异(P=0.465,0.563,0.587),见图3a。 两组术后各时间点腿部目测类比评分均较术前明显下降(PA组 < 0.001,PB组 < 0.001),腿部目测类比评分在术前及术后各随访时间段均无明显组间差异(P=0.865,0.785,0.587,0.755,0.763,0.745),见图3b。 两组术后各时间点Oswestry功能障碍指数均较术前明显下降(PA组 < 0.001,PB组 < 0.001)。术前Oswestry功能障碍指数无明显组间差异(P=0.796),术后1周A组Oswestry功能障碍指数低于B组(P < 0.05);而在术后1,3,6,12个月随访中,Oswestry功能障碍指数均未显示出组间差异(P=0.587,0.755,0.763,0.745),见图3c。"
| [1] MOBBS RJ, PHAN K, MALHAM G, et al. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1(1):2-18. [2] KONG F, ZHOU Q, QIAO Y, et al. [Comparison of unilateral biportal endoscopic transforaminal lumbar interbody fusion versus minimally invasive tubular transforaminal lumbar interbody fusion for lumbar degenerative disease]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2022;36(5):592-599. [3] DING Q, TANG X, ZHANG R, et al. Do Radiographic Results of Transforaminal Lumbar Interbody Fusion Vary with Cage Position in Patients with Degenerative Lumbar Diseases? Orthop Surg. 2022; 14(4):730-741. [4] KANG MS, HEO DH, KIM HB, et al. Biportal Endoscopic Technique for Transforaminal Lumbar Interbody Fusion: Review of Current Research. Int J Spine Surg. 2021;15(suppl 3):S84-S92. [5] KIM JE, YOO HS, CHOI DJ, et al. Comparison of Minimal Invasive Versus Biportal Endoscopic Transforaminal Lumbar Interbody Fusion for Single-level Lumbar Disease. Clin Spine Surg. 2021;34(2):E64-E71. [6] SONG KS, LEE CW, MOON JG. Biportal Endoscopic Spinal Surgery for Bilateral Lumbar Foraminal Decompression by Switching Surgeon’s Position and Primary 2 Portals: A Report of 2 Cases With Technical Note. Neurospine. 2019;16(1):138-147. [7] HEO DH, SON SK, EUM JH, et al. Fully endoscopic lumbar interbody fusion using a percutaneous unilateral biportal endoscopic technique: technical note and preliminary clinical results. Neurosurg Focus. 2017;43(2):E8. [8] GUO W, YE J, LI T, et al. Evaluation of the learning curve and complications in unilateral biportal endoscopic transforaminal lumbar interbody fusion: cumulative sum analysis and risk-adjusted cumulative sum analysis. J Orthop Surg Res. 2024;19(1):194. [9] TIAN D, LIU J, ZHU B, et al. Unilateral biportal endoscopic extreme transforaminal lumbar interbody fusion with large cage combined with endoscopic unilateral pedicle screw fixation for lumbar degenerative diseases: a technical note and preliminary effects. Acta Neurochir (Wien). 2023;165(1):117-123. [10] HEO DH, KIM JS, PARK CW, et al. Contralateral Sublaminar Endoscopic Approach for Removal of Lumbar Juxtafacet Cysts Using Percutaneous Biportal Endoscopic Surgery: Technical Report and Preliminary Results. World Neurosurg. 2019;122:474-479. [11] PARK JH, JUN SG, JUNG JT, et al. Posterior Percutaneous Endoscopic Cervical Foraminotomy and Diskectomy With Unilateral Biportal Endoscopy. Orthopedics. 2017;40(5):e779-e783. [12] HEO DH, EUM JH, JO JY, et al. Modified far lateral endoscopic transforaminal lumbar interbody fusion using a biportal endoscopic approach: technical report and preliminary results. Acta Neurochir (Wien). 2021;163(4):1205-1209. [13] YOU X, ZHAO B, ZHANG T, et al. Clinical Efficacy of Unilateral Dual-channel Endoscopic Lumbar Interbody Fusion for Lumbar Spondylolisthesis with Spinal Scoliosis. Orthop Surg. 2024;16(5):1134-1142. [14] FU H, HU Y, YANG D, et al. [Comparison of effectiveness between unilateral biportal endoscopic decompression and unilateral biportal endoscopic lumbar interbody fusion for degree Idegenerative lumbar spondylolisthesis]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2024; 38(2):169-175. [15] KIM JE, CHOI DJ. Biportal Endoscopic Transforaminal Lumbar Interbody Fusion with Arthroscopy. Clin Orthop Surg. 2018;10(2): 248-252. [16] GATAM AR, GATAM L, MAHADHIPTA H, et al. Unilateral Biportal Endoscopic Lumbar Interbody Fusion: A Technical Note and an Outcome Comparison with the Conventional Minimally Invasive Fusion. Orthop Res Rev. 2021;13:229-239. [17] SIHVONEN T, HERNO A, PALJARVI L, et al. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine (Phila Pa 1976). 1993;18(5):575-581. [18] HAN G, JIANG Y, ZHANG B, et al. Imaging Evaluation of Fat Infiltration in Paraspinal Muscles on MRI: A Systematic Review with a Focus on Methodology. Orthop Surg. 2021;13(4):1141-1148. [19] LIN GX, HUANG P, KOTHEERANURAK V, et al. A Systematic Review of Unilateral Biportal Endoscopic Spinal Surgery: Preliminary Clinical Results and Complications. World Neurosurg. 2019;125:425-432. [20] KIM N, JUNG SB. Biportal endoscopic spine surgery in the treatment of multi-level spontaneous lumbar epidural hematoma: Case report. J Orthop Sci. 2022;27(1):288-291. [21] HIRA K, NAGATA K, HASHIZUME H, et al. Relationship of sagittal spinal alignment with low back pain and physical performance in the general population. Sci Rep. 2021;11(1):20604. [22] HIYAMA A, KATOH H, SAKAI D, et al. The correlation analysis between sagittal alignment and cross-sectional area of paraspinal muscle in patients with lumbar spinal stenosis and degenerative spondylolisthesis. BMC Musculoskelet Disord. 2019;20(1):352. [23] MUELLNER M, HAFFER H, MOSER M, et al. Paraspinal musculature impairment is associated with spinopelvic and spinal malalignment in patients undergoing lumbar fusion surgery. Spine J. 2022;22(12): 2006-2016. [24] LV Y, CHEN M, WANG SL, et al. Endo-TLIF versus MIS-TLIF in 1-segment lumbar spondylolisthesis: A prospective randomized pilot study. Clin Neurol Neurosurg. 2022;212:107082. [25] LIN GX, YAO ZK, ZHANG X, et al. Evaluation of the Outcomes of Biportal Endoscopic Lumbar Interbody Fusion Compared with Conventional Fusion Operations: A Systematic Review and Meta-Analysis. World Neurosurg. 2022;160:55-66. [26] CHOI DJ, CHOI CM, JUNG JT, et al. Learning Curve Associated with Complications in Biportal Endoscopic Spinal Surgery: Challenges and Strategies. Asian Spine J. 2016;10(4):624-629. [27] KIM JE, YOO HS, CHOI DJ, et al. Learning Curve and Clinical Outcome of Biportal Endoscopic-Assisted Lumbar Interbody Fusion. Biomed Res Int. 2020;2020:8815432. [28] KIM SK, KANG SS, HONG YH, et al. Clinical comparison of unilateral biportal endoscopic technique versus open microdiscectomy for single-level lumbar discectomy: a multicenter, retrospective analysis. J Orthop Surg Res. 2018;13(1):22. [29] PANG D, YANG J, HAI Y, et al. Changes in paraspinal muscles and facet joints after percutaneous endoscopic transforaminal lumbar interbody fusion for the treatment of lumbar spinal stenosis: A 3-year follow-up. Front Surg. 2022;9:1041105. [30] KAWAGUCHI Y, MATSUI H, TSUJI H. Back muscle injury after posterior lumbar spine surgery. Part 2: Histologic and histochemical analyses in humans. Spine (Phila Pa 1976). 1994;19(22):2598-2602. |
| [1] | Zhang Chunlin, Hou Zhaohua, Yan Xu, Jiang Yan, Fu Su, Ning Yongming, Li Dongzhe, Dong Chao, Liu Xiaokang, Wang Yongkui, Cao Zhengming, Yang Tengyue. Decompression mechanism of symmetrically adduction of lumbar decompression induced resorption of herniated nucleus pulpous [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1810-1819. |
| [2] | Lu Qi, Sun Maji, Wang Xuezhi, Song Ting, Ma Yiming, Yuan Feng, Chen Hongliang. Two visual arthroplasty techniques for L5-S1 disc herniation: a half-year follow-up evaluation of clinical outcomes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1841-1847. |
| [3] | Feng Zhimeng, Sun Ning, Sun Zhaozhong, Li Yuefei, Liu Changzhen, Li Sa. Three-dimensional image reconstruction can safely assist one-hole split endoscope in treatment of #br# L5/S1 far lateral lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1876-1882. |
| [4] | Sun Yundi, Cheng Lulu, Wan Haili, Chang Ying, Xiong Wenjuan, Xia Yuan. Effect of neuromuscular exercise for knee osteoarthritis pain and function: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1945-1952. |
| [5] | Zhi Fang, Zhu Manhua, Xiong Wei, Lin Xingzhen. Analgesic effect of acupuncture in a rat model of lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 936-941. |
| [6] | Luo Dan, Ge Zhilin, Hou Yonghui, Wang Wanshun, Zhan Jiheng, Hou Yu, Lin Dingkun, Chen Shudong. Extraction and subculture of neural stem cells from mouse embryonic spinal cord: comparison and analysis on advantages and disadvantages of three commonly used digestive enzymes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6609-6615. |
| [7] | Zheng Xiang, Zhang Mingxing, Huang Ya, Shan Sharui. Improvement of lower limb walking function in patients with chronic non-specific low back pain by biofeedback assisted electrical stimulation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 547-553. |
| [8] | Wang Jianlei, He Peiliang, Sun Yongjian. A meta-analysis of clinical efficacy and safety of intravenous glucocorticoids before lower limb joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 599-607. |
| [9] | Li Jia, Liu Qianru, Xing Mengnan, Chen Bo, Jiao Wei, Meng Zhaoxiang. A network meta-analysis on therapeutic effect of different types of exercise on knee osteoarthritis patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 609-616. |
| [10] | Zhang Ziyu, Chen Longhao, Sheng Wei, Lyu Hanzhe, Shen Ying, Wang Binghao, Lyu Zhizhen, Lyu Lijiang. Application of artificial intelligence in the diagnosis and treatment of lumbar disc herniation: evolution towards standardization, efficiency, and precision of diagnosis and treatment methods [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6269-6276. |
| [11] | Bai Liang, Fu Su, Yan Xu, Zhang Chunlin, Li Ying . Measurement of intervertebral disc height and analysis of strength after induced resorption of herniated nucleus pulpous [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5785-5794. |
| [12] | Sun Yingjin, Liu Ning, Huang Long, Feng Shuo, Chen Xiangyang. Effect of patellar morphology on functional recovery and patellofemoral joint alignment after unicompartmental knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5826-5832. |
| [13] | Wang Jun, Zhang Hui, Li Zhengyuan, Hao Lin, Chen Shenghong, Yin Zongsheng. Assessment on initial effectiveness of a novel local infiltration anesthesia in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5839-5844. |
| [14] | Liu Jiashun, Xie Hongru, Sun Yunkai, Li Shujin, Mao Tengfei, An Yaoyao, Zhang Qin. Correlation and mechanism between lumbar disc degeneration and paraspinal muscle changes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5897-5906. |
| [15] | Fang Jun, Wei Wei, Xue Yating, Cui Chenlong, Wei Jiasheng, Shi Xiao, Yang Lijuan, Yang Baozhong. M2 macrophage-derived exosomes promote microglia M2-type polarization [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(25): 5320-5327. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||