Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (27): 5785-5794.doi: 10.12307/2025.834
Previous Articles Next Articles
Measurement of intervertebral disc height and analysis of strength after induced resorption of herniated nucleus pulpous
Bai Liang, Fu Su, Yan Xu, Zhang Chunlin, Li Ying
- Department of Orthopedics, First Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, Henan Province, China
-
Received:2024-03-20Accepted:2024-06-15Online:2025-09-28Published:2025-03-05 -
Contact:Zhang Chunlin, MD, Chief physician, Professor, Master’s supervisor, Department of Orthopedics, First Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, Henan Province, China Li Ying, Chief nurse, Department of Orthopedics, First Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, Henan Province, China -
About author:Bai Liang, Master candidate, Department of Orthopedics, First Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, Henan Province, China -
Supported by:intervertebral disc| lumbar disc herniation| cervical disc herniation| centroid| magnetic resonance image| artificial intelligence| biomechanics
CLC Number:
Cite this article
Bai Liang, Fu Su, Yan Xu, Zhang Chunlin, Li Ying . Measurement of intervertebral disc height and analysis of strength after induced resorption of herniated nucleus pulpous[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5785-5794.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
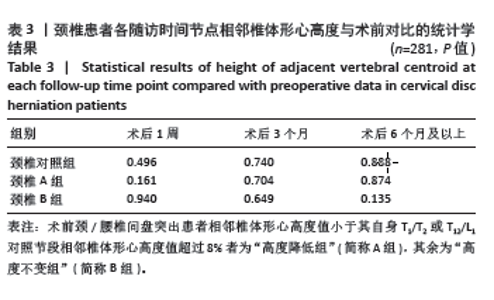
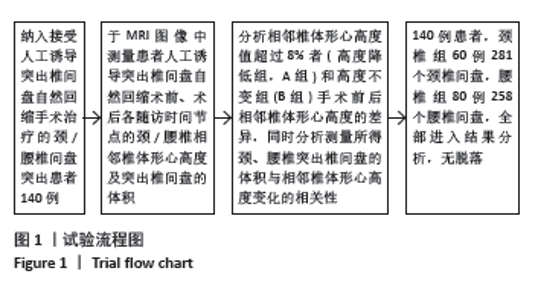
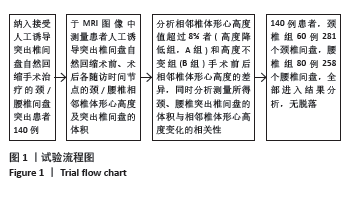
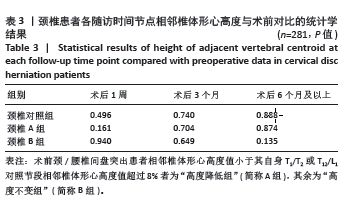
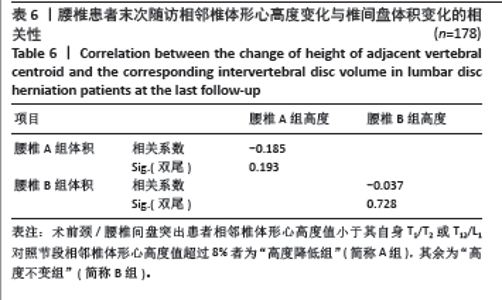
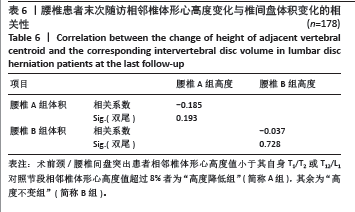
2.3 颈椎结果 2.3.1 相邻椎体形心高度变化情况 共观察颈椎间盘281个:①对照组60个,术前与术后末次随访相邻椎体形心高度平均值分别为20.46 mm[标准误为0.28,四分位水平为20.26(18.99,21.69)]及20.17 mm[标准误为0.71,四分位水平为19.60(18.72,20.78)],差异无显著性意义(P > 0.05);②A组162个,术前与术后末次随访相邻椎体形心高度平均值分别为 16.65 mm[标准误为0.28,四分位水平为16.50(15.34,18.05) mm]及15.92 mm[标准误为0.71,四分位水平为15.46(14.09,17.19) mm],各时间点相邻椎体形心高度变化差异无显著性意义(P > 0.05);③B组59个,术前与术后末次随访相邻椎体形心高度平均值分别为20.15 mm[标准误为0.33,四分位水平为19.89(18.34,21.50) mm]及19.09 mm[标准误为0.41,四分位水平为19.11(17.91,19.97) mm],各时间点相邻椎体形心高度变化差异无显著性意义(P > 0.05),见图2及表3。"
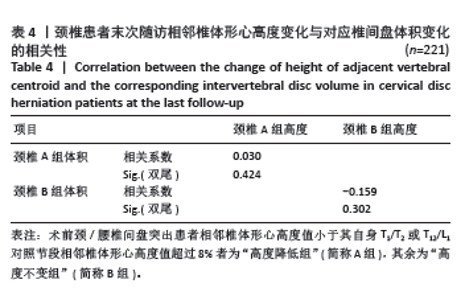
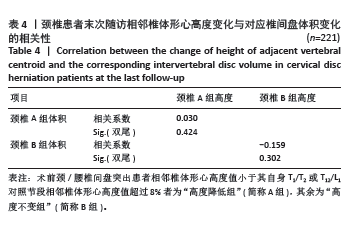
2.3.2 颈椎突出椎间盘体积 60例患者221个手术节段中 186个发生iRHNP,吸收比为84.2%(186/221),最大吸收率为91.67%,其中吸收率分级为轻度、中度、显著、完全吸收的节段在发生iRHNP现象节段中的占比分别为41.40%,37.63%,15.59%及5.38%(图3)。A组术前与术后颈椎突出椎间盘体积平均值分别是510.28 mm3和364.76 mm3,较术前平均缩小28.52%;B组术前与术后颈椎突出椎间盘体积平均值分别是466.16 mm3和307.33 mm3,较术前平均缩小34.07%。将其中iRHNP患者术前与术后末次随访的变化差值,与对应时间节点的突出椎间盘体积变化差值进行spearman相关性分析,根据检验结果可知(表4),二者之间无相关性(P > 0.05)。"
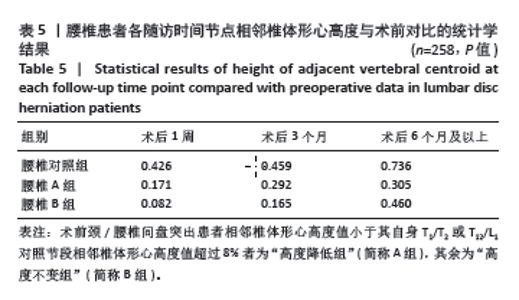
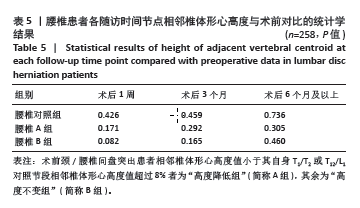
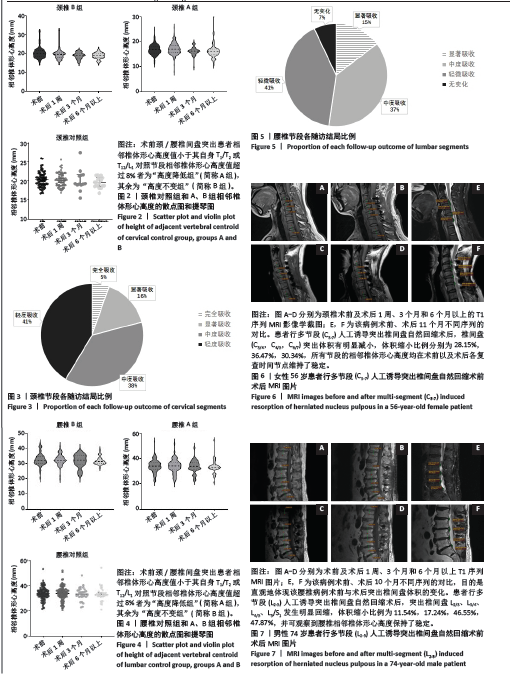
2.4 腰椎结果 2.4.1 相邻椎体形心高度变化情况 观察腰椎间盘共258个,其中:①对照组80个,术前与术后末次随访相邻椎体形心高度平均值约为33.03 mm[标准误为0.46,四分位水平为32.56(30.55,34.95)]和32.40 mm[标准误为0.57,四分位水平为31.38(30.41,33.50)],差异无显著性意义(P > 0.05);②A组59个,术前与术后末次随访相邻椎体形心高度平均值分别为30.08 mm[标准误为0.52,四分位水平为30.87(27.14,32.43) mm]和31.67 mm[标准误为0.61,四分位水平为32.02(27.39,34.89) mm],各时间点相邻椎体形心高度变化差异无显著性意义(P > 0.05);③B组119个,术前与术后末次随访相邻椎体形心高度平均值分别为35.91 mm[标准误为0.41,四分位水平为35.26(33.32,37.42) mm]和34.12 mm[标准误为0.69,四分位水平为33.86(32.10,36.58) mm],各时间点相邻椎体形心高度变化差异无显著性意义(P > 0.05),见图4及表5。"
2.4.2 腰椎突出椎间盘体积 80例腰椎间盘突出患者178个手术节段中有157个发生iRHNP,吸收比为88.20%(157/178)。最大吸收率为86.55%,其中吸收率分级为轻度、中度、显著、完全吸收的节段在全部研究节段中的占比分别为45.60%,36.00%及9.60% (图5)。A组术前与术后腰椎突出椎间盘体积平均值分别是690.51 mm3和496.58 mm3,较术前平均缩小28.09%;B组术前与术后腰椎突出椎间盘体积平均值分别是698.70 mm3和535.99 mm3,较术前平均缩小23.29%。 与颈椎组处理相同,将其中iRHNP患者术前与术后末次随访的变化差值,与对应时间节点的突出椎间盘体积变化差值进行spearman相关性分析,根据表6检验结果可知,二者之间无相关性(P > 0.05)。"
2.5 典型病例 2.5.1 典型病例1 如图6所示,女性患者,56岁,诉双手麻木、双足行走踩棉花感1年,双侧Hoffmann征阳性,双下肢肌张力增高,双下肢肌力Ⅳ级,经3个月保守治疗后疗效欠佳,症状有加重趋势,强烈要求予以手术治疗。行多节段(C3-7)iRHNP术后,突出颈椎间盘C3/4,C4/5,C6/7的体积于分别由术前274,104,96 mm3减至术后的197,66,67 mm3,吸收率分别为28.10%,36.54%,30.21%。图6A-D分别为颈椎术前及术后1周、3个月和6个月以上的T1序列MRI影像学截图,其中对照节段(T1/2)在上述4个时间节点的相邻椎体形心高度测量值分别为18.59,17.72,18.01,18.27 mm;C3/4为13.32,13.67,13.29,13.59 mm;C4/5为13.91,14.93,14.52,14.27 mm;C5/6为13.77,14.91,13.27,14.08 mm。 2.5.2 典型病例2 如图7所示,男性患者,74岁,诉腰部疼痛40余年,双侧下肢疼痛、麻木,行走时症状有加重3年,手术治疗意愿强烈。行L2-5节段iRHNP术后, L2/3、L3/4、L4/5、L5/S1椎间盘突出的体积分别由术前435,870,870,940 mm3减至术后末次随访体积的390,720,465,490 mm3,吸收率分别为10.34%,17.24%,46.55%,47.87%。图7A-D分别为术前及术后1周、3个月和6个月以上T1序列MRI图片,其中对照节段(T12/L1)在4个时间节点的相邻椎体形心高度测量值分别是29.05,28.63,28.84,28.97 mm;L2/3为31.62,32.21,31.22,32.46 mm;L3/4为30.85,30.42,30.69,30.47 mm;L4/5为30.74,31.89,31.89,31.82 mm;L5/S1为28.47,28.60,28.72,29.18 mm。"
| [1] HASHIMOTO K, AIZAWA T, KANNO H, et al. Adjacent segment degeneration after fusion spinal surgery—a systematic review. Int Orthop. 2018;43(4):987-993. [2] KANG T, PARK SY, KANG CH, et al. Is biportal technique/endoscopic spinal surgery satisfactory for lumbar spinal stenosis patients? Medicine. 2019;98(18):e15451. [3] MAZAS S, BENZAKOUR A, CASTELAIN JE, et al. Cervical disc herniation: which surgery? Int Orthop. 2018;43(4):761-766. [4] HOUTEN JK, WEINSTEIN GR, COLLINS M. Long-term fate of C3-7 arthrodesis: 4-level ACDF versus Cervical Laminectomy and Fusion. J Neurosurg Sci. 2021;65(4):402-407. [5] ALPERT JN. Review of the Diagnosis and Management of Lumbar Spinal Stenosis. JAMA. 2022;328(8):779-780. [6] FU S, ZHANG C, YAN X, et al. Volumetric Changes in Cervical Disc Herniation. Spine. 2022;47(7):E296-E303. [7] ZHANG C, FU S, YAN X, et al. Cervical microendoscopic laminoplasty-induced clinical resolution of disc herniation in patients with single- to three-level myelopathy. Sci Rep. 2022;12(1):18854. [8] CANALE ST, BEATY JH. Campbell’s Operative Orthopaedics. 11th ed. Philadephia: Mosby, 2011. [9] TEICHTAHL AJ, URQUHART DM, WANG Y, et al. A Dose–response relationship between severity of disc degeneration and intervertebral disc height in the lumbosacral spine. Arthritis Res Ther. 2015;17:297. [10] ABDOLLAH V, PARENT EC, SU A, et al. The effects of axial loading on the morphometric and T2 characteristics of lumbar discs in relation to disc degeneration. Clin Biomech. 2021;83:105291. [11] HUSSAIN M, NATARAJAN RN, AN HS, et al. Patterns of height changes in anterior and posterior cervical disc regions affects the contact loading at posterior facets during moderate and severe disc degeneration: a poroelastic C5-C6 finite element model study. Spine (Phila Pa 1976). 2010;35(18):E873-E881. [12] MAQUER G, SCHWIEDRZIK J, HUBER G, et al. Compressive strength of elderly vertebrae is reduced by disc degeneration and additional flexion. J Mech Behav Biomed Mater. 2015;42:54-66. [13] LUOMA K, VEHMAS T, RIIHIMÄKI H, et al. Disc Height and Signal Intensity of the Nucleus Pulposus on Magnetic Resonance Imaging as Indicators of Lumbar Disc Degeneration. Spine. 2001;26(6):680-686. [14] BROOKS M, DOWER A, ABDUL JALIL MF, et al. Radiological predictors of recurrent lumbar disc herniation: a systematic review and meta-analysis. J Neurosurg Spine. 2021;34(3):481-491. [15] O’CONNELL GD, JOHANNESSEN W, VRESILOVIC EJ, et al. Human internal disc strains in axial compression measured noninvasively using magnetic resonance imaging. Spine (Phila Pa 1976). 2007;32(25): 2860-2868. [16] DOLAN P, ADAMS MA. Recent advances in lumbar spinal mechanics and their significance for modelling. Clin Biomech. 2001;16:S8-S16. [17] TAO Y, GALBUSERA F, NIEMEYER F, et al. The impact of age, sex, disc height loss and T1 slope on the upper and lower cervical lordosis: a large-scale radiologic study. Eur Spine J. 2021;30(9):2434-2442. [18] DALY CD, GHOSH P, BADAL T, et al. A Comparison of Two Ovine Lumbar Intervertebral Disc Injury Models for the Evaluation and Development of Novel Regenerative Therapies. Global Spine J. 2018;8(8):847-859. [19] SUZUKI A, DAUBS MD, HAYASHI T, et al. Patterns of Cervical Disc Degeneration: Analysis of Magnetic Resonance Imaging of Over 1000 Symptomatic Subjects. Global Spine J. 2018;8(3):254-259. [20] 蒋欣, MORISHITA Y, HENRY H, 等. 腰痛患者MRI上各节段腰椎间盘退变形式与年龄的相关性分析[J]. 中国脊柱脊髓杂志,2009, 19(11):845-849. [21] ZHANG C, LI D, WANG C, et al. Cervical Endoscopic Laminoplasty for Cervical Myelopathy. Spine (Phila Pa 1976). 2016;41 Suppl 19:B44-B51. [22] 牛策号, 张春霖, 严旭, 等. 椎体后方结构及对突出椎间盘体积测量的影响[J]. 中国组织工程研究,2023,27(18):2897-2902. [23] YANG B, O’CONNELL GD. Intervertebral disc swelling maintains strain homeostasis throughout the annulus fibrosus: A finite element analysis of healthy and degenerated discs. Acta Biomater. 2019;100:61-74. [24] JEONG JG, KANG S, JUNG GH, et al. Biomechanical Effect of Disc Height on the Components of the Lumbar Column at the Same Axial Load: A Finite-Element Study. J Healthc Eng. 2022;2022(23):1-13. [25] ZHANG F, ZHANG K, TIAN HJ, et al. Correlation between lumbar intervertebral disc height and lumbar spine sagittal alignment among asymptomatic Asian young adults. J Orthop Surg Res. 2018;13(1):34. [26] 龚克, 胡学昱, 凃志鹏, 等. 影像学正常人群腰椎椎间高度指数、椎间角度及腰椎前凸角度的研究分析[J]. 生物骨科材料与临床研究,2018,15(2):19-24. [27] MCDONALD CL, ALSOOF D, GLUECK J, et al. Adjacent Segment Disease After Spinal Fusion. JBJS Rev. 2023;11(6). doi: 10.2106/JBJS.RVW.23.00028. [28] AHLGREN BD, LUI W, HERKOWITZ HN, et al. Effect of Anular Repair on the Healing Strength of the Intervertebral Disc. Spine. 2000;25(17): 2165-2170. [29] TANAKA N, AN HS, LIM TH, et al. The relationship between disc degeneration and flexibility of the lumbar spine. Spine J. 2001;1(1): 47-56. [30] O’CONNELL GD, SEN S, ELLIOTT DM. Human annulus fibrosus material properties from biaxial testing and constitutive modeling are altered with degeneration. Biomech Model Mechanobiol. 2011;11(3-4): 493-503. [31] YANG H, JEKIR MG, DAVIS MW, et al. Effective modulus of the human intervertebral disc and its effect on vertebral bone stress. J Biomech. 2016;49(7):1134-1140. [32] ALLEN MJ, SCHOONMAKER JE, BAUER TW, et al. Preclinical Evaluation of a Poly (Vinyl Alcohol) Hydrogel Implant as a Replacement for the Nucleus Pulposus. Spine. 2004;29(5):515-523. [33] KIRNAZ S, CAPADONA C, WONG T, et al. Fundamentals of Intervertebral Disc Degeneration. World Neurosurg. 2022;157(2):264-273. [34] LIU ZS, FANG M, YANG L, et al. Correlation between the height reduced and the degeneration of lumbar intervertebral disc. Chin J Med Imaging Technol. 2011;27(2):388-391. [35] MACKI M, HERNANDEZ-HERMANN M, BYDON M, et al. Spontaneous regression of sequestrated lumbar disc herniations: Literature review. Clin Neurol Neurosurg. 2014;120:136-141. [36] KIRKALDY-WILLIS WH, WEDGE JH, YONG-HING K, et al. Pathology and Pathogenesis of Lumbar Spondylosis and Stenosis. Spine. 1978; 3(4):319-328. [37] JIANFA Z, SHANGLI L, SHIZHEN Z. Experimental study on stiffness and strength of lumbar intervertebral disc. J Appl Biomech. 1996;(3): 160-162+189. [38] STOUSTRUP P, RESNICK CM, ABRAMOWICZ S, et al. Management of Orofacial Manifestations of Juvenile Idiopathic Arthritis: Interdisciplinary Consensus‐Based Recommendations. Arthritis Rheumatol. 2022;75(1):4-14. [39] POOTHERI S, ELLAM D, GRÜBL T, et al. A Two-Stage Automatic Color Thresholding Technique. Sensors (Basel). 2023;23(6):3361. [40] 刘盼. 关于DR测距误差的分析[J]. 中国辐射卫生,2020,29(2): 153-156. [41] Н.И.МУСХЕЛИШВИЛИ. Курсаналитической теометрии. 2016. [42] GUELLIL N, ARGAWAL N, KRIEGHOFF M, et al. Novel Methods to Measure Height and Volume in Healthy and Degenerated Lumbar Discs in MRIs: A Reliability Assessment Study. Diagnostics. 2022;12(6):1437. |
| [1] | Zhang Chunlin, Hou Zhaohua, Yan Xu, Jiang Yan, Fu Su, Ning Yongming, Li Dongzhe, Dong Chao, Liu Xiaokang, Wang Yongkui, Cao Zhengming, Yang Tengyue. Decompression mechanism of symmetrically adduction of lumbar decompression induced resorption of herniated nucleus pulpous [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1810-1819. |
| [2] | Lu Qi, Sun Maji, Wang Xuezhi, Song Ting, Ma Yiming, Yuan Feng, Chen Hongliang. Two visual arthroplasty techniques for L5-S1 disc herniation: a half-year follow-up evaluation of clinical outcomes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1841-1847. |
| [3] | Feng Zhimeng, Sun Ning, Sun Zhaozhong, Li Yuefei, Liu Changzhen, Li Sa. Three-dimensional image reconstruction can safely assist one-hole split endoscope in treatment of #br# L5/S1 far lateral lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1876-1882. |
| [4] | Zhi Fang, Zhu Manhua, Xiong Wei, Lin Xingzhen. Analgesic effect of acupuncture in a rat model of lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 936-941. |
| [5] | Yang Bin, Tao Guangyi, Yang Shun, Xu Junjie, Huang Junqing . Visualization analysis of research hotspots of artificial intelligence in field of spinal cord nerve injury and repair [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 761-770. |
| [6] | Song Haoran, Zhang Yuqiang, Gu Na, Zhi Xiaodong, Wang Wei. Visualization analysis of artificial intelligence in bone trauma research based on Citespace [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 493-502. |
| [7] | Zhao Yuxin, Liang Liang, Jin Feng, Xu Yangyang, Kang Zhijie, Fang Yuan, He Yujie, Wang Xing, Wang Haiyan, Li Xiaohe. Establishment and stress analysis of a finite element model for adolescent cervical disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 448-454. |
| [8] | Zhang Ziyu, Chen Longhao, Sheng Wei, Lyu Hanzhe, Shen Ying, Wang Binghao, Lyu Zhizhen, Lyu Lijiang. Application of artificial intelligence in the diagnosis and treatment of lumbar disc herniation: evolution towards standardization, efficiency, and precision of diagnosis and treatment methods [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6269-6276. |
| [9] |
Wang Qianliang, Zhang Qianzhongyi, Peng Yujian, Yan Jun.
Effects of unilateral biportal endoscopic transforaminal lumbar interbody fusion on paraspinal muscles
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5862-5868.
|
| [10] | Zhang Ruofan, Guan Huanhuan, He Zhuoqun, Zhang Yunfeng, Jin Feng, Wang Zhiqiang, Wang Jianzhong, Li Xiaohe, Zhu Yong, Wang Haiyan, Zhang Kai. Effect of minimally invasive interbody fusion device height on lumbar biomechanics in patients with adolescent lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4421-4429. |
| [11] | Gu Jiangpeng, Chen Xujing, Liu Yikang, Guo Wei, Liu Xiaomin, Wang Fei, Feng Wei. Short-term effect of manipulation therapy for lumbar disc herniation quantitatively evaluated by three-dimensional scoliosis angle [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4552-4559. |
| [12] | Wang Qianliang, Chen Jianpeng, Wang Yuanbin, Yan Jun. Mechanism of circ05188 targeting miR-199a-5p involved in nociceptive hypersensitivity in a rat model of lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(20): 4230-4238. |
| [13] | Wei Mengli, Zhong Yaping, Gui Huixian, Zhou Yiwen, Guan Yeming, Yu Shaohua. Sports injury prediction model based on machine learning [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(2): 409-418. |
| [14] | Bai Xue, Wang Xing, Hong Guoping, Jia Rushuo, Han Qi, Guo Huaiyu, Niu Hongkai, Zhang Shaojie, Chao Lumen. A three-dimensional virtual simulation platform for Mongolian medical brain vibration therapy constructed based on the three-dimensional motion capture technology [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(18): 3826-3832. |
| [15] | Bu Nan, Yang Yicheng, , Song Beibei, Bai Kaixiang, Du Yunyun, . Evaluating the compensatory function of intelligent assistive devices for the blind in China based on the International Classification of Functioning, Disability and Health [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(17): 3650-3656. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||