Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (27): 5773-5784.doi: 10.12307/2025.832
Previous Articles Next Articles
Biomechanical analysis on treatment of different types of osteoporotic vertebral compression fractures with individualized precise puncture vertebral augmentation
Pan Hongyu1, Li Hongtao1, Xiao Changming1, Li Sen2
- 1Department of Spine Surgery, Hospital of Traditional Chinese Medicine Affiliated to Southwest Medical University, Luzhou 646000, Sichuan Province, China; 2Department of Spine Surgery, Nanjing Drum Tower Hospital, Nanjing 210008, Jiangsu Province, China
-
Received:2024-05-31Accepted:2024-08-12Online:2025-09-28Published:2025-03-05 -
Contact:Li Sen, MD, Chief physician, Department of Spine Surgery, Nanjing Drum Tower Hospital, Nanjing 210008, Jiangsu Province, China -
About author:Pan Hongyu, Master candidate, Department of Spine Surgery, Hospital of Traditional Chinese Medicine Affiliated to Southwest Medical University, Luzhou 646000, Sichuan Province, China Li Hongtao, Master candidate, Department of Spine Surgery, Hospital of Traditional Chinese Medicine Affiliated to Southwest Medical University, Luzhou 646000, Sichuan Province, China Xiao Changming, MS, Attending physician, Department of Spine Surgery, Hospital of Traditional Chinese Medicine Affiliated to Southwest Medical University, Luzhou 646000, Sichuan Province, China Pan Hongyu, Li Hongtao, and Xiao Changming contributed equally to this article.
CLC Number:
Cite this article
Pan Hongyu, Li Hongtao, Xiao Changming, Li Sen. Biomechanical analysis on treatment of different types of osteoporotic vertebral compression fractures with individualized precise puncture vertebral augmentation[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5773-5784.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

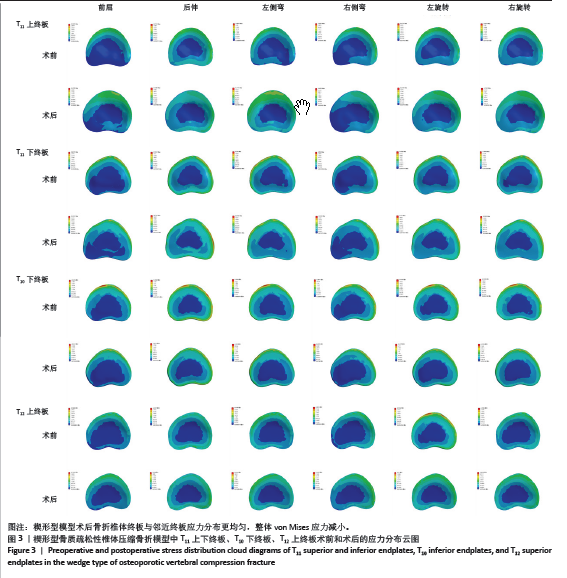
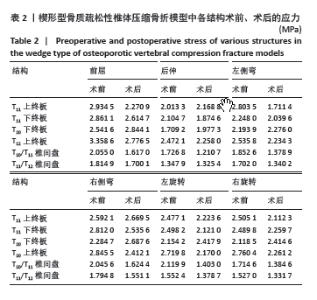
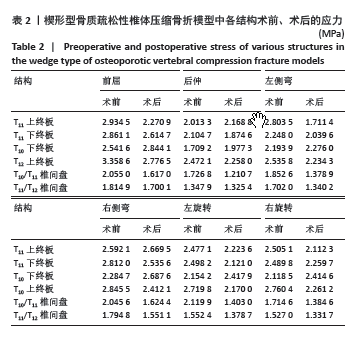
在6种椎体生理运动状态下(前屈、后伸、左右侧弯、左右旋转),术前T11上终板最大von Mises应力值分别为2.934 5,2.013 3,2.803 5,2.592 1,2.477 1,2.505 1 MPa;而术后T11上终板最大von Mises应力值分别2.270 9,2.168 8,1.711 4,2.669 5,2.223 6,2.112 3 MPa。相比术前,T11上终板的应力除了后伸状态和右侧弯状态,其余运动状态下的应力都有明显的降低,前屈减少22.61%,后伸增加7.72%,左侧弯减少38.59%,右侧弯增加7.74%,左旋转减少10.23%,右旋转减少15.56%。在6种椎体生理运动状态下,术前T11下终板最大von Mises应力值分别为2.861 1,2.104 7,2.248 0,2.812 0,2.498 2,2.489 8 MPa;术后T11下终板最大von Mises应力值分别为2.614 7,1.874 6、2.039 6,2.535 6,2.121 0,2.259 7 MPa,相比于术前,T11下终板的应力整体下降,前屈减少8.61%,后伸减少23.01%,左侧弯减少9.27%,右侧弯减少9.83%,左旋转减少15.1%,右旋转减少9.24%(图4)。 在6种椎体生理运动状态下,术前T10下终板的最大von Mises应力值分别为2.541 6,1.709 2,2.193 9,2.284 7,2.154 2,2.118 5 MPa;术后分别为2.844 1,1.977 3,2.276,2.687 6,2.417 9,2.414 6 MPa,相比术前,T10下终板的应力均有增加,前屈增加11.9%,后伸增加13.75%,左侧弯增加3.74%,右侧弯增加17.63%,左旋转增加12.24%,仅有右旋转减少13.98%。在6种椎体生理运动状态下,T12上终板术前的最大von Miese应力值分别为3.358 6,2.472 1,2.535 8,2.845 5,2.719 8,2.760 4 MPa;而术后最大von Miese应力值分别为2.776 5,2.258,2.234 3,2.412 1,2.17,2.261 2 MPa,经过个体化精准穿刺椎体强化术治疗后的T12上终板的应力均明显下降,前屈减少17.33%,后伸减少8.66%,左侧弯减少11.89%,右侧弯减少15.23%,左旋转减少20.21%,右旋转减少18.18%(图4)。 2.1.2 椎间盘应力的变化 在楔形型模型中,其椎间盘的应力分布云图和应力数据见图5及表2。在6种椎体生理运动状态下,T10/T11椎间盘术前的最大von Mises应力值分别为2.055 0,1.726 8,1.852 6,2.045 6,2.119 9,1.714 6 MPa;术后T10/T11椎间盘最大von Mises应力值分别为1.617,1.210 7,1.378 9,1.624 4,1.403,1.384 6 MPa,术后T10/T11椎间盘的应力相比术前下均有显著降低,其中前屈减少21.31%,后伸减少29.89%,左侧弯减少25.57%,右侧弯减少20.59%,左旋转减少33.82%,右旋转减少19.25%。在6种椎体生理运动状态下,术前T11/T12椎间盘的最大von Mises应力值分别为1.814 9,1.347 9,1.702 0,1.794 8,1.552 4,1.527 0 MPa;术后则分别为1.700 1,1.325 4,1.340 2,1.551 1,1.378 7,1.331 7 MPa,术后T11/T12椎间盘的应力较术前相比,均显著降低,其中前屈减少6.33%,后伸减少1.67%,左侧弯减少21.26%,右侧弯减少13.58%,左旋转减少11.19%,右旋转减少12.79%(图4)。"
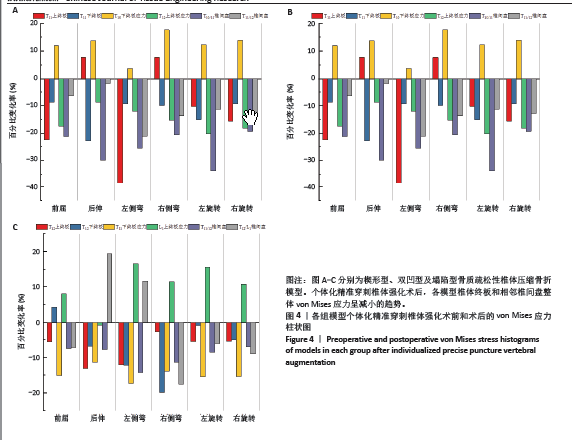

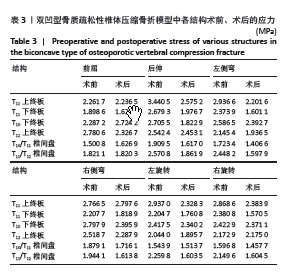
2.2 双凹型模型结果 2.2.1 骨折椎体终板以及邻近终板的应力变化 在双凹型模型中,其骨折椎体终板以及邻近终板的应力分布云图和应力数据见图6及表3。 在6种椎体生理运动状态下,T11上终板术前的最大von Mises应力值分别为2.261 7,3.440 5,2.936 6,2.766 5,2.937 0, 2.868 6 MPa;术后的最大von Mises应力值为2.236 5,2.575 2,2.201 6,2.797 6,2.328 3,2.383 9 MPa,相比于术前,T11上终板的应力除右侧弯时有轻微增高,其余运动状态下的应力都明显降低,分别为前屈减少1.11%,后伸减少25.15%,左侧弯减少14.81%,右侧弯增加1.11%,左旋转减少20.73%,右旋转减少5.89%。在6种椎体生理运动状态下,T11下终板术前的von Mises应力值分别为1.898 6,2.679 3,2.373 9,2.207 7,2.204 7,2.380 8 MPa;术后,T11下终板von Mises应力值分别为1.621 0,1.976 7,1.601 1,1.818 0,1.760 8,1.570 5 MPa,与术前相比,T11下终板的应力在6种椎体生理运动状态下均明显降低,分别为前屈减少14.62%,后伸减少26.22%,左侧弯减少35.55%,右侧弯减少17.65%,左旋转减少20.13%,右旋转减少34.03%(图4)。 在6种椎体生理运动状态下,T10下终板术前的最大von Mises应力值分别为2.287 2,2.705 5,2.586 5,2.797 9,2.417 5,2.422 9 MPa;术后最大von Mises应力值分别为2.724 2,1.822 9,2.392 7,2.395 9,2.340 2,2.371 1 MPa,T10下终板的应力相比术前,除前屈增加19.11%,其余动作的应力均降低,后伸减少32.62%,左侧弯减少7.49%,右侧弯减少14.37%,左旋转减少3.2%,右旋转减少2.14%。在6种椎体生理运动状态下,术前T12上终板的最大von Mises应力值分别为2.780 6,2.542 4,2.145 4,2.518 7,2.044,2.1729 MPa;而术后T12上终板的最大von Mises应力值分别为2.326 7,2.453 1,1.936 5,2.287 9,1.895 7,2.175 MPa,经过个体化精准穿刺椎体强化治疗后T12上终板的应力整体表现为下降的趋势,前屈减少16.32%,后伸减少3.51%,左侧弯减少9.74%,右侧弯减少9.16%,左旋转减少7.26%,右旋转增加0.1%(图4)。 2.2.2 椎间盘应力的变化 在双凹型模型中,其椎间盘应力分布云图和应力数据见图5及表3。在6种椎体生理运动状态下,T10/T11椎间盘术前的最大von Mises应力值为1.500 8,1.909 5,1.723 4,1.879 1,1.543 9,1.596 8 MPa;术后T10/T11椎间盘最大von Mises应力值分别为1.626 9,1.617,1.406 6,1.716 1,1.513 7,1.457 7 MPa,术后的T10/T11椎间盘的应力相较于术前,除前屈动作增加8.4%,其余生理运动状态下的应力均降低,后伸减少15.32%,左侧弯减少18.38%,右侧弯减少8.67%,左旋转减少1.96%,右旋转减少8.71%。在6种椎体生理运动状态下,T11/T12椎间盘术前的最大von Miese应力值分别为1.821 1,2.570 8,2.448 2,1.944 1,2.259 8,2.149 6 MPa;术后T11/T12椎间盘最大von Miese应力值分别为1.820 3,1.861 9,1.597 9,1.613 8,1.603 5,1.604 5 MPa,术后的T11/T12椎间盘的应力显著降低,前屈减少0.04%,后伸减少27.58%,左侧弯减少34.73%,右侧弯减少16.99%,左旋转减少29.04%,右旋转减少25.36%(图4)。 "


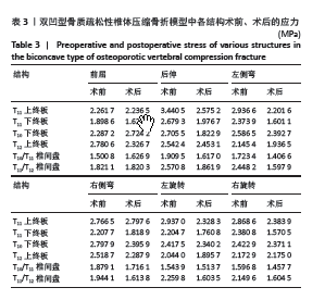
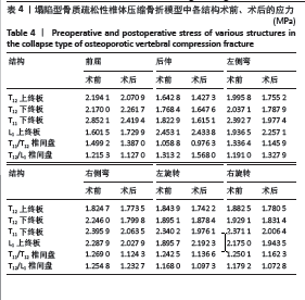
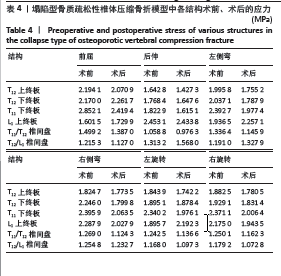
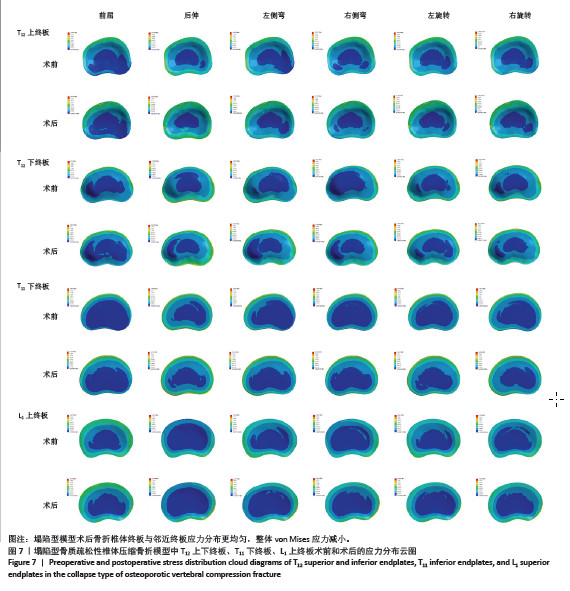
2.3 塌陷型模型结果 2.3.1 骨折椎体终板以及邻近终板的应力变化 在塌陷型模型中,其骨折椎体终板以及邻近终板的应力分布云图和应力数据见图7及表4。在6种椎体生理运动状态下,T12上终板术前的最大von Mises应力值为2.194 1,1.642 8,1.995 8,1.824 7,1.843 9,1.882 5 MPa;术后T12上终板最大von Mises应力值为2.070 9,1.427 3,1.755 2,1.773 5,1.742 2,1.780 5 MPa,相比于术前,T12上终板的应力在术后表现出下降的趋势,前屈减少5.62%,后伸减少13.12%,左侧弯减少12.06%,右侧弯减少2.81%,左旋转减少5.52%,右旋转减少5.42%。在6种椎体生理运动状态下,术前T12下终板的最大von Mises应力值为2.170 0,1.768 4,2.037 1,2.246,1.895 1,1.929 1 MPa;术后T12下终板的最大von Mises应力值则为2.261 7,1.647 6,1.787 9,1.799 8,1.878 4 MPa,与术前相比,术后T12下终板的应力除前屈动作外,其余生理运动状态的应力均明显降低,为前屈增加4.23%,后伸减少6.83%,左侧弯减少12.23%,右侧弯减少19.87%,左旋转减少0.88%,右旋转减少5.06%(图4)。 在6种椎体生理运动状态下,T11下终板术前的最大von Mises应力值为2.852 1,1.822 9,2.392 7,2.395 9,2.340 2,2.371 1 MPa;术后T11下终板最大von Mises应力值为2.419 4,1.615 1,1.977 4,2.063 5,1.976 1,2.006 4 MPa,相比于术前,T11下终板的应力均降低,前屈减少15.17%,后伸减少11.4%,左侧弯减少17.36%,右侧弯减少13.87%,左旋转减少15.56%,右旋转减少15.38%。在6种椎体生理运动状态下,L1上终板术前的最大von Mises应力值为1.601 5,2.453 1,1.936 5,2.287 9,1.895 7, 2.175 0 MPa;术后L1上终板最大von Mises应力值分别为1.729 9,2.433 8,2.257 1,2.027 9,2.192 3,1.943 5 MPa, 术后L1椎体上终板的应力相比术前表现出增大的趋势,仅有后伸动作时减少0.79%,而前屈增加8.02%,左侧弯增加16.56%,右侧弯增加11.36%,左旋转增加15.65%,右旋转增加10.63%(图4)。 2.3.2 椎间盘应力的变化 在塌陷型模型中,其椎间盘的应力分布云图见图5及表4。在6种椎体生理运动状态下,T11/T12椎间盘术前的最大von Mises应力值为1.499 2,1.058 8,1.336 4,1.269,1.242 5,1.250 1 MPa;术后T11/T12椎间盘最大von Mises应力值分别为1.387,0.976 3,1.145 9,1.124 3,1.136 6,1.162 3 MPa,相比于术前,T11/T12椎间盘术后的应力均降低,前屈减少7.48%,后伸减少7.79%,左侧弯减少14.25%,右侧弯减少11.4%,左旋转减少8.52%,右旋转减少7.02%。在6种椎体生理运动状态下,T12/L1椎间盘术前最大von Mises应力值为1.215 3,1.313 2,1.191,1.254 8,1.168,1.179 2 MPa;术后,T12/L1椎间盘最大von Mises应力值分别为1.127,1.568,1.327 9,1.232 7,1.097 3,1.072 8 MPa,相比于术前前,T12/L1椎间盘术后的应力在后伸和左侧弯动作时表现出应力增大,分别为后伸增加19.4%,左侧弯11.49%,而其余动作均有着不同程度的降低,其中前屈减少7.27%,右侧弯减少17.61%,左旋转减少6.05%,右旋转减少9.02%(图4)。"
| [1] 中华医学会骨质疏松和骨矿盐疾病分会,章振林.原发性骨质疏松症诊疗指南(2022)[J].中国全科医学,2023,26(14):1671-1691. [2] WANG F, SUN R, ZHANG SD, et al. Comparison of thoracolumbar versus non-thoracolumbar osteoporotic vertebral compression fractures in risk factors, vertebral compression degree and pre-hospital back pain. J Orthop Surg Res. 2023;18(1):643. [3] KAWANISHI M, TANAKA H, ITO Y, et al. Treatment for Osteoporotic Vertebral Fracture - A Short Review of Orthosis and Percutaneous Vertebroplasty and Balloon Kyphoplasty. Neurospine. 2023;20(4):1124-1131. [4] 任亚楠.椎体强化术治疗骨质疏松椎体压缩性骨折的生物力学分析[D].天津:天津理工大学,2023. [5] CAZZATO RL, BELLONE T, SCARDAPANE M, 等.椎体强化术可降低骨质疏松性椎体压缩骨折病人的12个月死亡率和发病率[J].国际医学放射学杂志,2022,45(1):117. [6] ZHU D, HU JN, WANG L, et al. A Modified Unilateral Extrapedicular Approach Applied to Percutaneous Kyphoplasty to Treat Lumbar Osteoporotic Vertebral Compression Fracture: A Retrospective Analysis. Pain Physician. 2023;26(3):E191-E201. [7] 顾晨希,虞宵,黄安全,等.单侧椎体后外上方入路与双侧椎弓根入路行椎体成型术治疗骨质疏松性椎体压缩骨折的生物力学对比研究[J].生物骨科材料与临床研究,2022,19(5):16-20+26. [8] 杨春雷,王岩群,王卫国,等.研究单侧与双侧经皮椎体后凸成形术治疗老年骨质疏松性胸腰椎压缩性骨折的效果[J].中国现代药物应用,2024,18(4):30-33. [9] 柴大起,马成才.单侧与双侧椎弓根穿刺经皮椎体后凸成形术治疗老年骨质疏松性椎体压缩骨折的疗效比较[J].中国骨与关节损伤杂志,2022,37(7):708-711. [10] 张立创,杨雯,丁广江,等. 个体化单侧椎弓根外入路与双侧椎弓根入路椎体成形后骨水泥的弥散效果 [J]. 中国组织工程研究, 2025,29(4):800-808. [11] 包志强,陈国强,陈贤艺,等.骨质疏松性胸腰椎压缩骨折经皮椎体成形术后非手术椎体继发骨折的危险因素分析[J].中国骨与关节损伤杂志,2024,39(1):73-76. [12] WANG JN, XIE W, SONG DW, et al. Recurrence of Local Kyphosis After Percutaneous Kyphoplasty: The Neglected Injury of the Disc-Endplate Complex. Clin Interv Aging. 2023;18:827-834. [13] MELTON LJ, LANE AW, COOPER C, et al. Prevalence and incidence of vertebral deformities. Osteoporos Int. 1993;3(3):113-119. [14] ISMAIL AA, COOPER C, FELSENBERG D, et al. Number and type of vertebral deformities: epidemiological characteristics and relation to back pain and height loss. European Vertebral Osteoporosis Study Group. Osteoporos Int. 1999;9(3):206-213. [15] 权祯,秦大平,张晓刚,等.骨质疏松性椎体压缩骨折强化术后骨组织-骨水泥界面生物力学应力再平衡机制的有限元研究[J].中国脊柱脊髓杂志,2023,33(12):1107-1118. [16] 吴智华,李任,潘慧玲,等.骨水泥弥散类型对强化椎体生物力学特性影响的有限元分析[J].中国组织工程研究,2023,27(30):4763-4768. [17] 程明,彭诗语,江娇,等.不同治疗方法对骨质疏松性胸腰椎压缩骨折椎体力学稳定性影响的有限元分析[J].中国修复重建外科杂志,2022,36(12):1519-1523. [18] BOGER A, HEINI P, WINDOLF M, et al. Adjacent vertebral failure after vertebroplasty: a biomechanical study of low-modulus PMMA cement. Eur Spine J. 2007;16(12):2118-2125. [19] PENG Y, DU X, HUANG L, et al. Optimizing bone cement stiffness for vertebroplasty through biomechanical effects analysis based on patient-specific three-dimensional finite element modeling. Med Biol Eng Comput. 2018;56(11):2137-2150. [20] 赵文韬,秦大平,张晓刚,等.骨质疏松性椎体压缩骨折椎体强化术后不同椎体高度对相邻椎体应力影响的有限元分析[J].中国骨质疏松杂志,2018,24(9):1141-1147. [21] LIANG D, YE LQ, JIANG XB, et al. Biomechanical effects of cement distribution in the fractured area on osteoporotic vertebral compression fractures: a three-dimensional finite element analysis. J Surg Res. 2015; 195(1):246-256. [22] ZUO XH, CHEN YB, XIE P, et al. Finite element analysis of wedge and biconcave deformity in four different height restoration after augmentation of osteoporotic vertebral compression fractures. J Orthop Surg Res. 2021;16(1):138. [23] YANG H, LIU H, WANG S, et al. Review of Percutaneous Kyphoplasty in China. Spine (Phila Pa 1976). 2016;41 Suppl 19:B52-B58. [24] ZINDRICK MR, WILTSE LL, DOORNIK A, et al. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine (Phila Pa 1976). 1987;12(2):160-166. [25] 蒲俊刚,范伟力,赵建华,等.单侧个体化经椎弓根旁入路穿刺椎体成形术在中段胸椎骨质疏松性椎体压缩骨折中的应用[J].创伤外科杂志,2019,21(8):574-578. [26] 熊小明,宋偲茂,万趸,等.CT影像数据指导单侧入路经皮椎体后凸成形术治疗椎体压缩性骨折[J].中国矫形外科杂志,2012,20(22): 2035-2038. [27] 刘祥飞,何金国,蒋钰钢,等.单侧与双侧入路椎体成形术治疗老年骨质疏松性椎体压缩骨折的有限元分析及临床应用[J].医用生物力学,2018,33(3):218-223. [28] XIONG XM, SUN YL, SONG SM, et al. Efficacy of unilateral transverse process-pedicle and bilateral puncture techniques in percutaneous kyphoplasty for Kummell disease. Exp Ther Med. 2019;18(5):3615-3621. [29] 郭营,李宝田,李骁腾,等.改良单侧经皮椎体后凸成形术结合对侧经皮椎体成形术治疗骨质疏松性椎体压缩性骨折的效果[J].临床医学工程,2024,31(4):459-460. [30] 张志伟,李利,黄兹谕,等.单、双侧椎弓根入路及单侧椎弓根外入路椎体成形治疗胸腰段椎体压缩性骨折:骨水泥灌注量与渗漏率[J].中国组织工程研究,2020,24(9):1353-1358. [31] 高旭,邢文华.有限元分析法在脊柱外科领域的应用[J].中国组织工程研究,2023,27(18):2921-2927. [32] 贺凯,邢文华,李峰,等.有限元法在脊柱胸腰段骨折生物力学分析中的应用及发展方向[J].中国组织工程研究,2025,29(15): 3244-3252. [33] 陈荣彬,李勇,白杰,等.三种骨水泥弥散类型对胸腰段椎体强化术后术椎应力影响的三维有限元分析[J].中国脊柱脊髓杂志,2020, 30(7):628-637. [34] 李安明,史国号,王国柱,等.椎体成形术对相邻椎体生物力学影响的有限元分析[J].重庆医学,2021,50(2):215-219. [35] 李家琼,王冬梅,孙璟川,等.骨水泥对椎体成形术治疗胸腰椎骨质疏松压缩性骨折的生物力学影响[J].医用生物力学,2018,33(1): 6-12. [36] Zuo XH, Chen YB, Xie P, et al. Finite element analysis of wedge and biconcave deformity in four different height restoration after augmentation of osteoporotic vertebral compression fractures. J Orthop Surg Res. 2021;16(1):138. |
| [1] | Chen Huiting, Zeng Weiquan, Zhou Jianhong, Wang Jie, Zhuang Congying, Chen Peiyou, Liang Zeqian, Deng Weiming. Tail anchoring technique of vertebroplasty in treatment of osteoporotic vertebral compression fractures with intravertebral cleft: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2145-2152. |
| [2] | Zeng Xuan, Weng Rui, Ye Shicheng, Tang Jiadong, Mo Ling, Li Wenchao. Two lumbar rotary manipulation techniques in treating lumbar disc herniation: a finite element analysis of biomechanical differences [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2153-2161. |
| [3] | Cheng Qisheng, Julaiti·Maitirouzi, Xiao Yang, Zhang Chenwei, Paerhati·Rexiti. Finite element analysis of novel variable-diameter screws in modified cortical bone trajectory of lumbar vertebrae [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2162-2171. |
| [4] | Wu Hongxu, Liu Xuanyu, Wang Taoyu, Wang Shiyao, Cheng Jingyi, Zhang Mingwen, Zhang Yinxia, Liu Zhihua, Wang Xiaojie. Finite element simulation of scoliosis with muscle unit introduction: verification of correction effect under bidirectional load [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2172-2181. |
| [5] | Liu Jiafu, Ren Ruxia, Liao Zhouwei, Zhou Xiali, Wu Yihong, Zhang Shaoqun. Three-dimensional finite element analysis of cervical spine biomechanical characteristics in a rat model of cervical vertigo [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2182-2190. |
| [6] | Zhou Daobin, Wang Kehao, Xie Yang, Ning Rende. Biomechanical characteristics of volar locking plate only versus combined dorsal mini-plate fixation of distal radius fractures with dorsal ulnar fragment [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2255-2261. |
| [7] | Liu Wenlong, Dong Lei, Xiao Zhengzheng, Nie Yu. Finite element analysis of tibial prosthesis loosening after fixed-bearing unicompartmental knee arthroplasty for osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2191-2198. |
| [8] | Zheng Wangyang, Fei Ji, Yang Di, Zhao Lang, Wang Lingli, Liu Peng, Li Haiyang. Finite element analysis of the force changes of the supraspinatus tendon and glenohumeral joint during the abduction and flexion of the humerus [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2199-2207. |
| [9] | Cai Qirui, Dai Xiaowei, Zheng Xiaobin, Jian Sili, Lu Shaoping, Liu Texi, Liu Guoke, Lin Yuanfang. Mechanical effects of Long’s traction orthopedic method on cervical functional units: quantitative analysis of biomechanical model of head and neck [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2208-2216. |
| [10] | Rao Jingcheng, Li Yuwan, Zheng Hongbing, Xu Zhi, Zhu Aixiang, Shi Ce, Wang Bing, Yang Chun, Kong Xiangru, Zhu Dawei. Biomechanical differences between the new proximal femoral stable intramedullary nail and traditional intramedullary nail#br# [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2217-2225. |
| [11] | Chen Long, Wang Xiaozhen, Xi Jintao, Lu Qilin. Biomechanical performance of short-segment screw fixation combined with expandable polyetheretherketone vertebral body replacement in osteoporotic vertebrae [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2226-2235. |
| [12] | Yan Xiangning, Chen Lei, Chen Yonghuan, Wang Chao, Li Xiaosheng. Influence of different depths and loads on knee joint mechanics and peripheral muscle force characteristics during squatting [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2236-2247. |
| [13] | Zheng Xuying, Hu Hongcheng, Xu Libing, Han Jianmin, Di Ping. Stress magnitude and distribution in two-piece cement-retained zirconia implants under different loading conditions and with varying internal connection shapes [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1979-1987. |
| [14] | Hu Xiongke, Liu Shaohua, Tan Qian, Liu Kun, Zhu Guanghui. Shikonin intervention with bone marrow mesenchymal stem cells improves microstructure of femur in aged mice [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1609-1615. |
| [15] | Cai Ziming, Yu Qinghe, Ma Pengfei, Zhang Xin, Zhou Longqian, Zhang Chongyang, Lin Wenping. Heme oxygenase-1 alleviates lipopolysaccharide-induced inflammatory response in nucleus pulposus mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1624-1631. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||