Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (24): 5224-5236.doi: 10.12307/2025.683
Previous Articles Next Articles
Different electromagnetic stimulation programs improve post-stroke dysphagia: a network Meta-analysis
Hu Tong1, Li Xuan1, Yuan Jing2, Wang Wei3
- 1Rehabilitation Medical College of Shandong University of Traditional Chinese Medicine, Jinan 250300, Shandong Province, China; 2School of Rehabilitation Medicine, Qilu Medical University, Zibo 255300, Shandong Province, China; 3Navy Qingdao Special Service Rehabilitation Center, Qingdao 266071, Shandong Province, China
-
Received:2024-07-02Accepted:2024-08-13Online:2025-08-28Published:2025-02-05 -
Contact:Wang Wei, MD, Associate chief physician, Master’s supervisor, Navy Qingdao Special Service Rehabilitation Center, Qingdao 266071, Shandong Province, China -
About author:Hu Tong, Master’s candidate, Rehabilitation Medical College of Shandong University of Traditional Chinese Medicine, Jinan 250300, Shandong Province, China -
Supported by:Army Healthcare Special Project, No. 20BJZ08 (to WW); Naval Special Service Personnel Injury and Disease Rehabilitation Functional Laboratory Construction Project
CLC Number:
Cite this article
Hu Tong, Li Xuan, Yuan Jing, Wang Wei. Different electromagnetic stimulation programs improve post-stroke dysphagia: a network Meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5224-5236.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
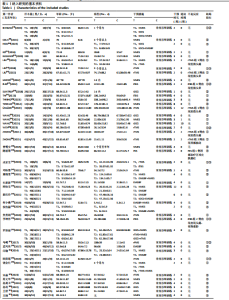
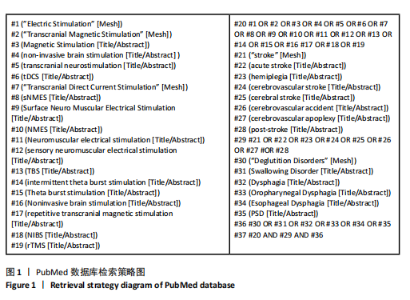
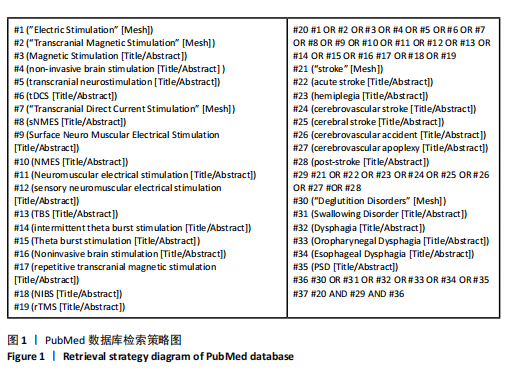
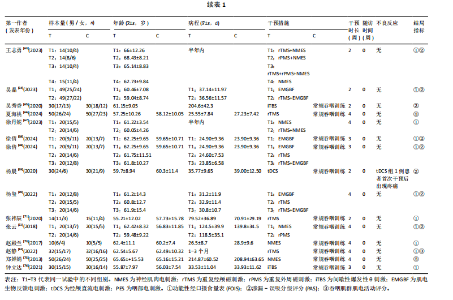
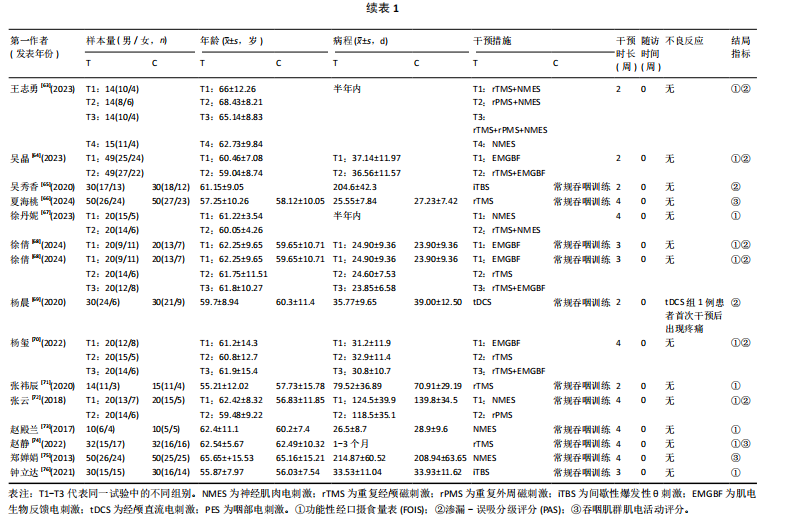
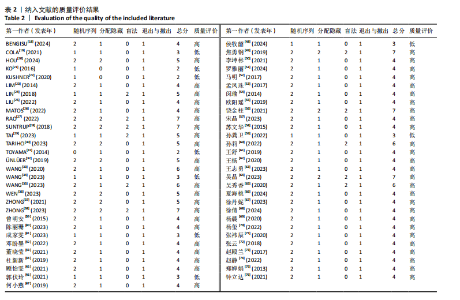
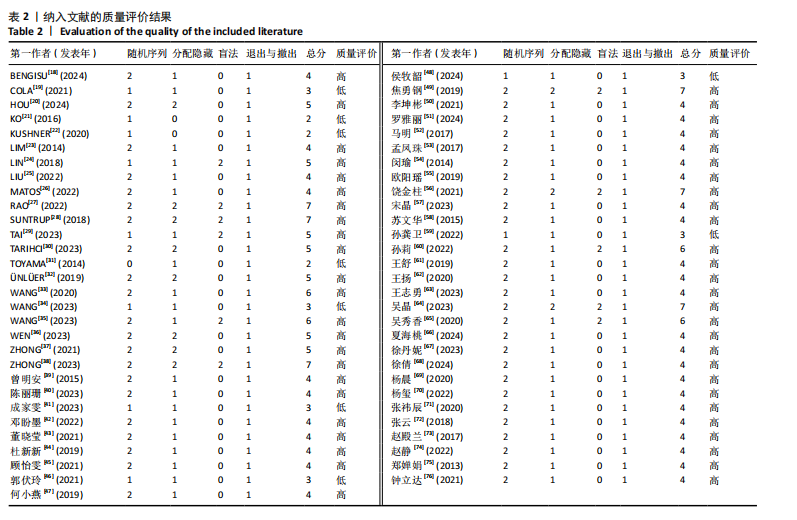
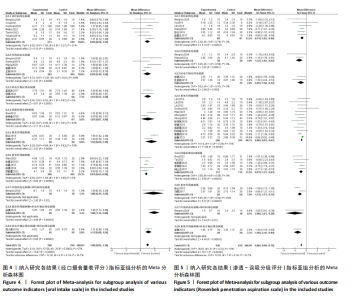
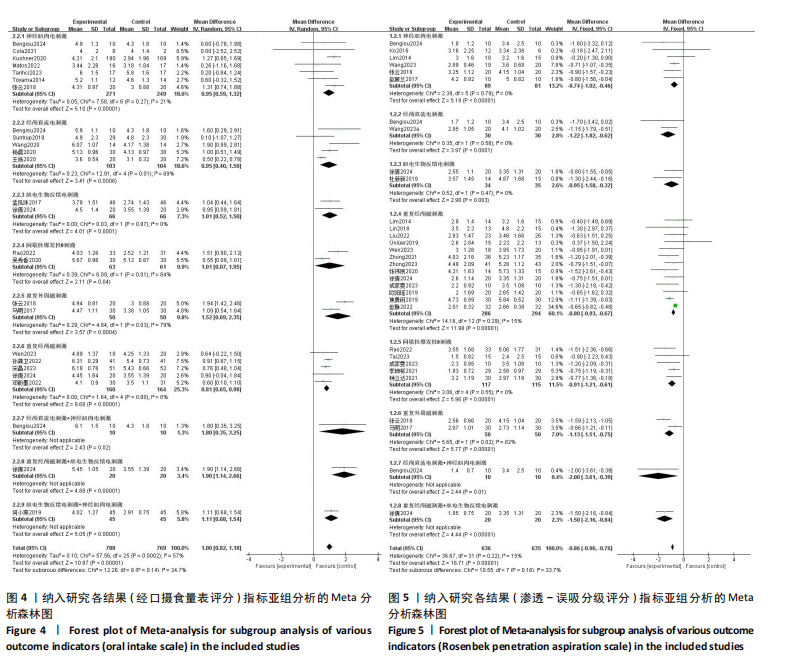
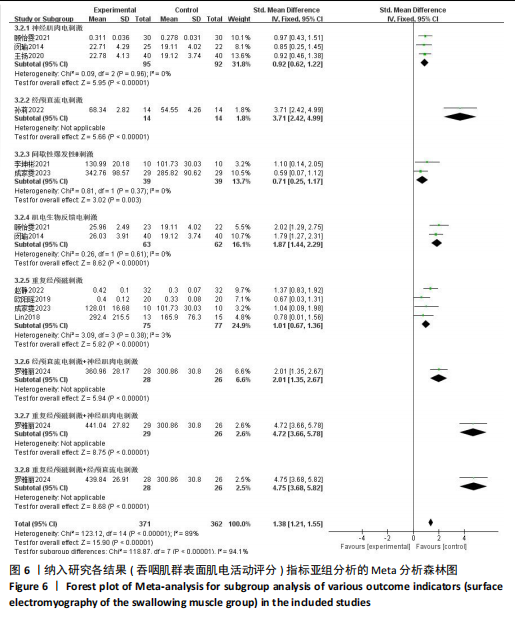
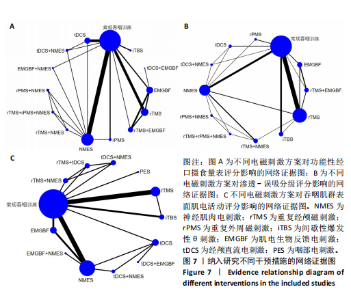
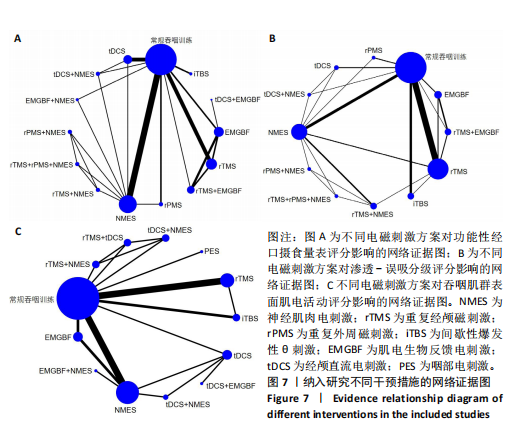
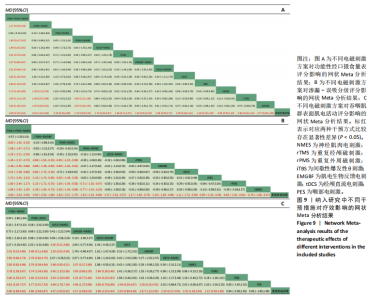
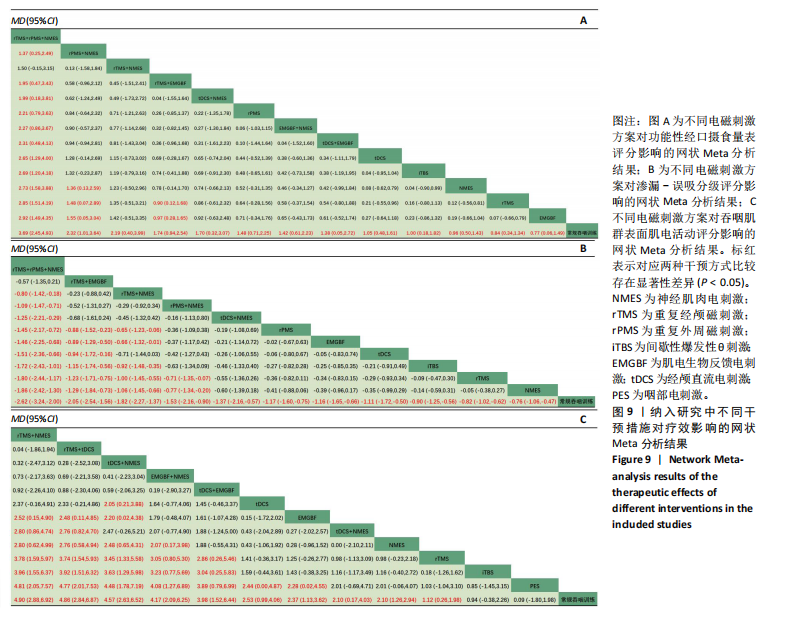
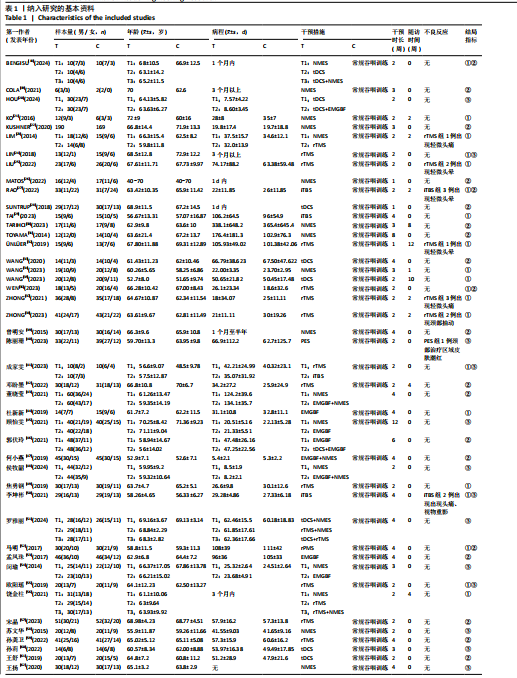
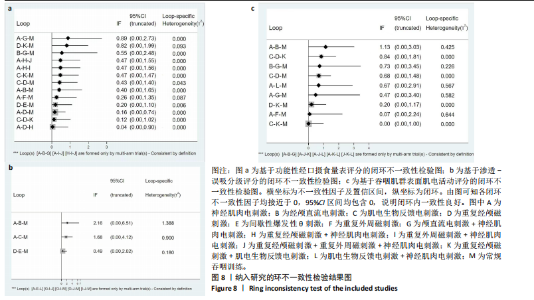
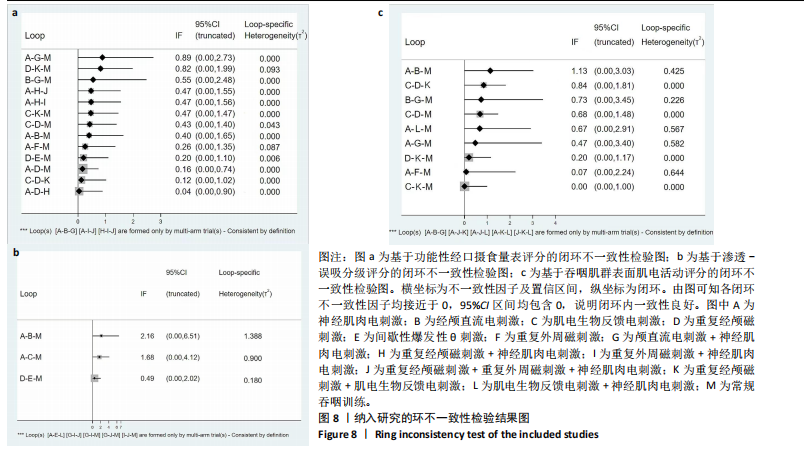
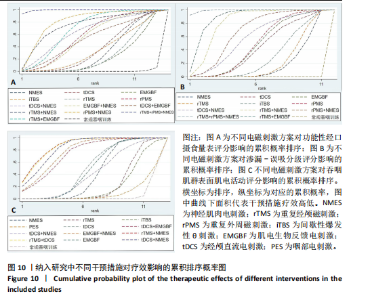
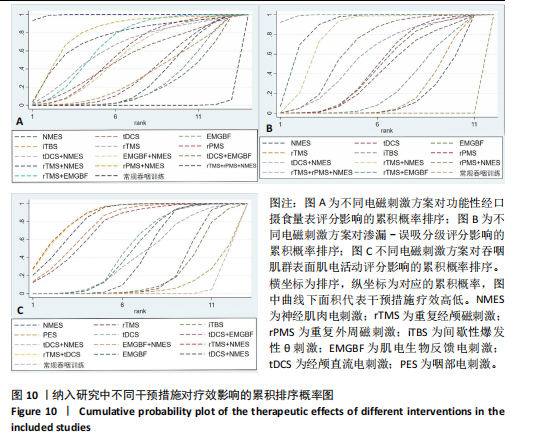
2.2 纳入文献基本特征 文章共纳入59篇文献,发表年限为2013-2024年,包含NMES、PES、rTMS、重复外周磁刺激(repetitive peripheral magnetic stimulation,rPMS)、间歇性爆发性θ刺激(intermittent theta-burst stimulation,iTBS)、肌电生物反馈电刺激(electromyographic biofeedback therapy,EMGBF)、tDCS及其联合电磁刺激,共15种电磁刺激方案。纳入文献的基本特征见表1。 2.3 纳入文献的方法学质量评估 59篇文献提及随机化,其中11篇文献未明确报道随机化方法[19,21-22,24,29,33-34,41,46,48,59],1篇文献没有严格执行随机分组[31],11篇文献采用分配隐藏的方法[20,27-28,30,32,36-38,49,56,64],10篇文献严格执行盲法[24,27-29,34,38,56,60,64-65],25篇文献采取评估者盲法[18-19,23-25,27-31,33,35-37,49,52,55-56,64-65,68,71-73,76]。 所纳入的研究均不存在选择性报告和结果缺失,文中均未提及其他偏倚风险。详细结果见图3。根据修订版Jadad量表进行质量评价结果,1-3分为低质量,4-7分为高质量,结果显示高质量文献50篇[18,20,23-30,32,34-40,42-45,47,49-58,60-76], 低质量文献9篇[19,21-22,31,33,41,46,48,59],平均4.35分,纳入文献总体质量较高,见表2。 2.4 传统Meta分析结果 在改善经口摄食能力方面,涉及22篇文献[18-19,22,26-28,30-31,35-36,39,42,47,52-53,57,59,61,65,68-69,72],包含9种电磁刺激方案,整体异质性检验I2=75%,P < 0.05,提示各研究间差异较大。剔除高异质性文献后整体异质性I2=57%,P < 0.05,异质性仍较高,因此仅对结果做描述性分析,与对照组相比,电磁刺激组(MD=1.00,95%CI:0.82-1.18)能显著提高患者经口摄食能力。根据干预方式的不同进行亚组分析,与常规训练相比,各电磁刺激方案均能显著提高患者经口摄食能力,见图4。 在防误吸能力方面,涉及25篇文献[18,21,23-25,27,29,32-34,36-38,41,44,49-50,52,55,68,71-74,76],包含8种电磁刺激方案,整体异质性检验I2=15%,P=0.22,各研究间差异较小,采用固定效应模型进行分析,结果表明,与对照组相比,电磁刺激组 (MD=-0.86,95%CI:-0.96至-0.76)能显著提高患者防误吸能力(P < 0.05)。根据干预方式的不同进行亚组分析,与常规训练相比,各电磁刺激方案均能显著提高患者防误吸能力,差异有显著性意义 (P < 0.05),见图5。 在提高吞咽肌群肌电活动水平方面,涉及13篇[24,41,45,50-51,54-55,58,60,62,66,74-75]文献,包含8种电磁刺激方案,整体异质性检验I2=89%,P < 0.05,提示各研究间差异较大。逐一剔除文献后异质性没有显著降低,采用随机效应模型进行分析,因此仅对结果做描述性分析,结果表明与对照组相比,电磁刺激组 (SMD=1.38,95%CI:1.21-1.25)能够较好地提高患者吞咽肌群肌电活动水平。按干预方式进行亚组分析后组内异质性显著降低,采用固定效应模型进行分析,结果表明,与常规训练相比,各电磁刺激方案均能显著提高患者咽肌群肌电活动水平(P < 0.05),见图6。 2.5 网状Meta分析结果 2.5.1 网络证据图 各指标的网络证据图,见图7。各圆点分别代表不同干预措施,圆点大小代表参与患者的数量,圆点之间的连线是两种干预措施之间直接比较研究的数量,实线越粗,表明直接比较的研究越多。 2.5.2 不一致性检验结果 在功能性经口摄食量表评分结局指标方面,整体不一致检验P=0.87,节点分裂法对局部进行不一致性检验,结果显示各组比较P > 0.05。在渗透-误吸分级评分结局指标方面,整体不一致检验P=0.25,节点分裂法对局部进行不一致性检验,结果显示各组比较P > 0.05。在吞咽肌群表面肌电活动评分结局指标方面,整体不一致检验P=0.128,节点分裂法对局部进行不一致性检验,结果显示NMES与EMGBF两两对比存在局部不一致性,其他各组P > 0.05。通过Inconsistency图检验结局指标的环不一致性。3个结局指标的环不一致性因子(IF)的95%CI均包含0,表明直接比较和间接比较之间具有较好的一致性,见图8。 2.5.3 纳入研究的累积概率排序比较结果 在功能性经口摄食量表评"
分评分结局指标方面,包括27篇文献[18-19,22,26-28,30-31,35-36,39,42-43,46-47,52-53,57,59,61,63-65,68-70,72],共1 968例患者,涉及13种电磁刺激方案,与常规吞咽训练组相比,电磁刺激组在提高脑卒中后吞咽障碍患者经口摄食能力上效果更优,评分差异均具有显著性意义。在不同电磁刺激方案之间,rTMS+rPMS+NMES明显优于除rTMS+NMES外的其他电磁刺激方案,差异有显著性意义,见图9。各电磁刺激方案的最佳概率排序为rTMS+rPMS+NMES > rPMS+NMES > rTMS+NMES > rTMS+EMGBF > tDCS+NMES > rPMS > EMGBF+NMES > tDCS+EMGBF > tDCS > iTBS > NMES > rTMS > EMGBF > 常规吞咽训练,累计概率比较见图10。 在渗透-误吸分级评分结局指标方面,包括30篇文献[18,21,23-25,27,29,32-34,36-38,41,44,49-50,52,55-56,63-64,67-68,70-74,76],共1 512例患者,涉及11种电磁刺激方案,与常规吞咽训练组相比,电磁刺激组在提高脑卒中后吞咽障碍患者防误吸能力上效果更优,评分差异均具有显著性意义。在不同电磁刺激方案之间,rTMS+rPMS+NMES明显优于除rTMS+EMGBF外的其他电磁刺激方案,差异有显著性意义,见图9。各电磁刺激方案的最佳概率排序为rTMS+rPMS+NMES > rTMS+EMGBF > rTMS+NMES > rPMS+NMES > tDCS+NMES > rPMS > EMGBF > tDCS > iTBS > rTMS > NMES > 常规吞咽训练,累计概率比较见图10。 在吞咽肌群表面肌电活动评分结局指标方面,包括16篇文献[20,24,40-41,45,48,50-51,54-55,58,60,62,66,74-75],共1 165例患者,涉及12种电磁刺激方案,除iTBS和PES外,其他各电磁刺激组均优于常规吞咽训练组,评分差异有显著性意义。在不同电磁刺激方案之间,rTMS+NMES和rTMS+tDCS明显优于其他电磁刺激方案,评分差异有显著性意义,但两组间评分差异无显著性意义,见图9。各电磁刺激方案的最佳概率排序为rTMS+NMES > rTMS+tDCS > tDCS+NMES > EMGBF+NNMES > tDCS+EMGBF > tDCS > EMGBF > tDCS+NMES > NMES > rTMS > iTBS > PES > 常规吞咽训练,累积概率比较见图10。"
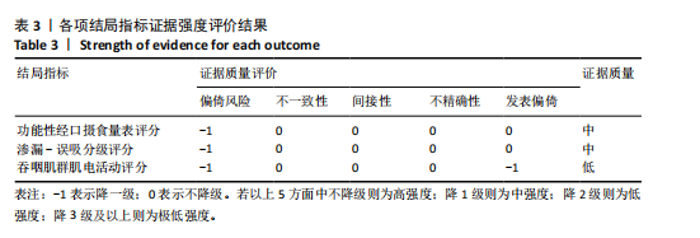
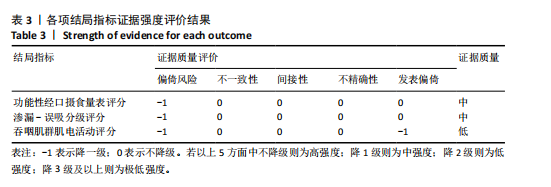
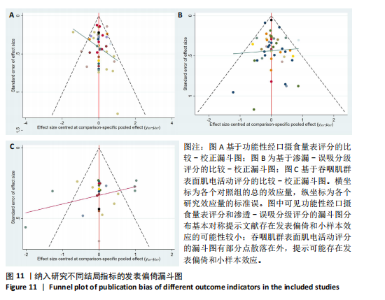
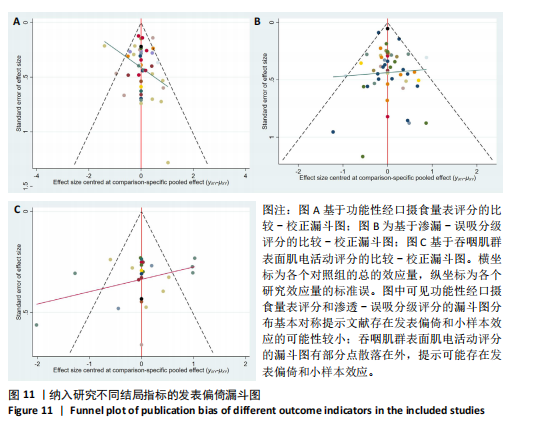
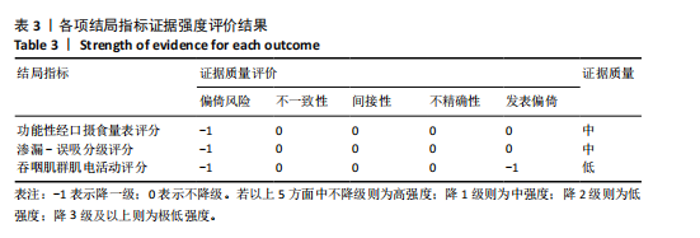
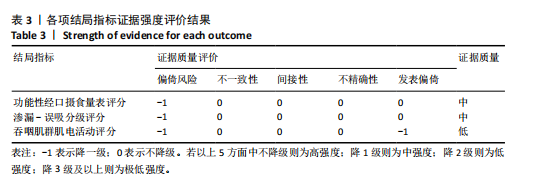
2.6 不良反应分析 所纳入文献报道的不良反应较少,6篇文献报道rTMS组有患者在治疗过程中出现轻微头晕、头痛,结束后症状很快消失[23,25,27,32,37,50]。1篇文献报道rTMS组在刺激小脑区域时[38],患者颈部区域出现肌肉抽动。1篇文献报道tDCS干预后,1例患者首次干预后出现头痛,第2天头痛症状消失[69]。电磁刺激的总体安全性较高。 2.7 发表偏倚分析 各指标的漏斗图见图11。针对功能性经口摄食量表评分和渗漏-误吸分级评分的漏斗图,大部分圆点落在图像上部,整体左右对称性较好,提示文章存在发表偏倚的可能性小。针对吞咽肌群表面肌电活动评分的漏斗图,不完全对称,且部分圆点位于漏斗图外侧,提示文章可能存在一定的小样本效应以及发表偏倚,研究结果需谨慎看待。 2.8 GRADE证据分级结果 针对不同结局指标的纳入研究总体在分配隐藏和盲法上存在偏倚风险,漏斗图显示吞咽肌群表面肌电活动水平存在发表偏倚,因此基于功能性经口摄食量表评分和渗漏-误吸分级评分的结果证据强度为中强度,基于吞咽肌群肌电活动评分的结果证据强度为低强度,见表3。通过分析结果可得中枢与外周的联合磁刺激治疗在改善经口摄食能力和防误吸能力上效果最佳,其次为中枢磁刺激联合外周电刺激。重复经颅磁刺激+神经肌肉电刺激在提高吞咽肌群表面肌电活动水平方面效果明显。对不良反应的分析可得,电磁刺激方案总体安全性较好。经GRADE证据分级可得,中枢与外周的联合磁刺激治疗效果最佳,其次为中枢磁刺激联合外周电刺激,均为强推荐。"
| [1] WEN X, LIU Z, ZHONG L, et al. The Effectiveness of repetitive transcranial magnetic stimulation for post-stroke dysphagia: a systematic review and meta-analysis. Front Hum Neurosci. 2022;16: 841781. [2] SáNCHEZ-SáNCHEZ E, AVELLANEDA-LóPEZ Y, GARCíA-MARíN E, et al. Knowledge and practice of health professionals in the management of dysphagia. Int J Environ Res Public Health. 2021; 18(4):2139. [3] 中国康复医学会吞咽障碍康复专业委员会.中国吞咽障碍康复管理指南(2023版)[J].中华物理医学与康复杂志,2023,45(12):1057-1072. [4] 岑晚霞,张若,古剑雄.神经刺激技术对神经源性吞咽障碍治疗效果的研究进展[J].神经疾病与精神卫生,2023,23(2):139-144. [5] MIRAGLIA F, PAPPALETTERA C, BARBATI SA, et al. Brain complexity in stroke recovery after bihemispheric transcranial direct current stimulation in mice. Brain Commun. 2024;6(3): fcae137. [6] HUH JW, PARK E, MIN YS, et al. Optimal placement of electrodes for treatment of post-stroke dysphagia by neuromuscular electrical stimulation combined with effortful swallowing. Singapore Med J. 2020;61(9):487-491. [7] 杜锦超,张承栋,雷俊芳,等.经颅直流电刺激的不同刺激方式对脑卒中后吞咽障碍治疗效果的网状meta分析[J].中国康复医学杂志, 2024,39(4):558-564. [8] 郁满华,李军文,叶子翔,等.重复经颅磁刺激治疗脑卒中后吞咽障碍疗效的Meta分析[J].神经损伤与功能重建,2021,16(6):311-315. [9] 杨晨,窦祖林.非侵入性脑刺激技术治疗卒中后吞咽障碍疗效的meta分析[J].中国康复医学杂志,2022,37(7):948-954. [10] 韩春彦,赵存,王兴蕾,等.13种干预方案治疗脑卒中吞咽困难效果的网状Meta分析[J].护理研究,2020,34 (11):1869-1877. [11] CHENG I, SASEGBON A, HAMDY S. Effects of neurostimulation on poststroke dysphagia: a synthesis of current evidence from randomized controlled trials. Neuromodulation. 2021;24(8): 1388-1401. [12] ZHU H, DENG X, LUAN G, et al. Comparison of efficacy of non-pharmacological intervention for post-stroke dysphagia: a systematic review and Bayesian network meta-analysis. BMC Neurosci. 2023; 24(1):53. [13] 贾宏声,王璠,陈春,等.不同生物制剂治疗类风湿性关节炎有效性及安全性的网状Meta分析[J].中国组织工程研究,2024,28(29):4748-4756. [14] 中华医学会神经病学分会,中华医学会神经病学分会脑血管病学组.中国急性缺血性脑卒中诊治指南2018[J].中华神经科杂志,2018,51(9): 666-682. [15] 柳青,翟伟,谭亚芹,等.临床研究文献质量评价工具浅析[J].中国针灸,2014,34(9):919-922. [16] GUYATT GH, OXMAN AD, SCHÜNEMANN HJ, et al. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64(4):380-382. [17] 张新新,高克,谢世栋,等.非手术治疗慢性踝关节不稳者足踝功能和动态平衡能力的网状Meta分析[J].中国组织工程研究,2025,29(9): 1931-1944. [18] BENGISU S, DEMIR N, KRESPI Y. Effectiveness of conventional dysphagia therapy (CDT), neuromuscular electrical stimulation (NMES), and transcranial direct current stimulation (tDCS) in acute post-stroke dysphagia: a comparative evaluation. Dysphagia. 2024;39(1):77-91. [19] COLA PC, ONOFRI SMM, RUBIRA CJ, et al. Electrical, taste, and temperature stimulation in patients with chronic dysphagia after stroke: a randomized controlled pilot trial. Acta Neurol Belg. 2021;121(5):1157-1164. [20] HOU M, ZHAO Y, ZHAO L, et al. Efficacy of game training combined with surface electromyography biofeedback on post-stroke dysphagia. Geriatr Nurs. 2024;55: 255-262. [21] KO KR, PARK HJ, HYUN JK, et al. Effect of laryngopharyngeal neuromuscular electrical stimulation on dysphonia accompanied by dysphagia in post-stroke and traumatic brain injury patients: a pilot study. Ann Rehabil Med. 2016;40(4):600‐610. [22] KUSHNER DS, JOHNSON-GREENE D, CORDERO MK, et al. Swallowing outcomes and discharge destinations in acute stroke tube-feeding dependent dysphagia patients treated with neuromuscular electrical stimulation during inpatient rehabilitation. Am J Phys Med Rehabil. 2020;99(6):487-494. [23] LIM KB, LEE HJ, YOO J, et al. Effect of low-frequency rTMS and NMES on subacute unilateral hemispheric stroke with dysphagia. Ann Rehabil Med. 2014;38(5):592‐602. [24] LIN WS, CHOU CL, CHANG MH, et al. Vagus nerve magnetic modulation facilitates dysphagia recovery in patients with stroke involving the brainstem - A proof of concept study. Brain Stimulation. 2018;11(2):264-270. [25] LIU HY, PENG Y, LIU ZC, et al. Hemodynamic signal changes and swallowing improvement of repetitive transcranial magnetic stimulation on stroke patients with dysphagia: a randomized controlled study. Front Neurol. 2022;11;13:918974. [26] MATOS KC, DE OLIVEIRA VF, DE OLIVEIRA PLC, et al. Combined conventional speech therapy and functional electrical stimulation in acute stroke patients with dyphagia: a randomized controlled trial. BMC Neurol. 2022;22(1):231. [27] RAO J, LI F, ZHONG L, et al. Bilateral cerebellar intermittent theta burst stimulation combined with swallowing speech therapy for dysphagia after stroke: a randomized, double-blind, sham-controlled, clinical trial. Neurorehabil Neural Repair. 2022;36(7):437-448.
[28] SUNTRUP-KRUEGER S, RINGMAIER C, MUHLE P, et al. Randomized trial of transcranial direct current stimulation for poststroke dysphagia. Ann Neurol. 2018;83(2):328-340. [29] TAI JH, HU RP, FAN SJ, et al. Theta-burst transcranial magnetic stimulation for dysphagia patients during recovery stage of stroke: a randomized controlled trial. Eur J Phys Rehabil Med. 2023;59(5):543-553. [30] TARIHCI CAKMAK E, SEN EI, DORUK C, et al. The effects of neuromuscular electrical stimulation on swallowing functions in post-stroke dysphagia: a randomized controlled trial. Dysphagia. 2023; 38(3):874-885. [31] TOYAMA K, MATSUMOTO S, KURASAWA M, et al. Novel neuromuscular electrical stimulation system for treatment of dysphagia after brain injury. Neurol Med Chir (Tokyo). 2014;54(7):521-528. [32] ÜNLÜER N, TEMUçIN ÇM, DEMIR N, et al. Effects of low-frequency repetitive transcranial magnetic stimulation on swallowing function and quality of life of post-stroke patients. Dysphagia. 2019; 34(3):360-371. [33] WANG ZY, CHEN JM, LIN ZK, et al. Transcranial direct current stimulation improves the swallowing function in patients with cricopharyngeal muscle dysfunction following a brainstem stroke. Neurol Sci. 2020;41(3):569-574. [34] WANG LY, SHI AQ, XUE H, et al. Efficacy of transcranial direct current stimulation combined with conventional swallowing rehabilitation training on post-stroke dysphagia. Dysphagia. 2023;38(6):1537-1545. [35] WANG Y, HE YX, JIANG LL, et al. Effect of transcutaneous auricular vagus nerve stimulation on post-stroke dysphagia. J Neurol. 2023;270(2): 995-1003. [36] WEN X, YANG Q, LIU ZC, et al. The effect of repetitive transcranial magnetic stimulation in synchronization with effortful swallowing on post-stroke dysphagia. Dysphagia. 2023; 38(3):912-922. [37] ZHONG LD, RAO JZ, WANG J, et al. Repetitive transcranial magnetic stimulation at different sites for dysphagia after stroke: a randomized, observer-blind clinical trial. Front Neurol. 2021;12:625683. [38] ZHONG LD, WEN X, LIU ZC, et al. Effects of bilateral cerebellar repetitive transcranial magnetic stimulation in poststroke dysphagia: a randomized sham-controlled trial. Neurorehabilitation. 2023; 52(2):227-234. [39] 曾明安,陈玲,王如蜜,等.低频电刺激结合康复训练进行吞咽障碍管理的疗效观察[J].中国康复医学杂志,2015,30(9):951-953. [40] 陈丽珊,周惠嫦,张盘德,等.口腔内低频电刺激对脑卒中吞咽障碍患者舌功能的疗效观察[J].中国康复,2023,38(10): 610-612. [41] 成家雯,王先斌,吴霜.高频rTMS与iTBS对单侧大脑半球卒中后吞咽障碍者吞咽功能电生理指标的影响[J].贵州医科大学学报,2022, 47(6):678-685. [42] 邓盼墨,阮璎璐,程冰苑,等.重复经颅磁刺激技术治疗脑卒中后吞咽功能障碍的研究[J].中国医刊,2022,57(4):461-464. [43] 董晓莹,张影.肌电生物反馈联合吞咽训练及低频电刺激对卒中后并发吞咽障碍者康复效果及舌骨喉复合体动度的影响[J].湖南师范大学学报(医学版),2021, 18(5):116-120. [44] 杜新新,王强,孟萍萍,等.肌电生物反馈强化训练对脑卒中后吞咽障碍患者吞咽功能的影响[J].中华物理医学与康复杂志,2019,41(6):411-415. [45] 顾怡雯,舒锦.表面肌电生物反馈与神经肌肉电刺激对脑卒中吞咽障碍疗效及生活质量的影响[J].中国康复,2021,36(10): 599-603. [46] 郭伏玲,夏文广,张阳普,等.经颅直流电联合表面肌电生物反馈治疗脑卒中后吞咽障碍的疗效观察[J].神经损伤与功能重建,2021, 16(12):766-768. [47] 何小燕,钟建兵,刘剑.电生理疗法联合吞咽-摄食训练治疗脑卒中后吞咽障碍疗效观察[J].中华老年多器官疾病杂志,2019,18(5):360-364. [48] 侯牧韶,赵艺杰,李红玲.表面肌电生物反馈治疗早期脑卒中后吞咽障碍的疗效观察[J].脑与神经疾病杂志,2024,32(3): 138-143. [49] 焦勇钢,袁明贤,戴颖仪.双侧重复经颅磁刺激对急性脑梗死后吞咽困难的影响[J].实用医学杂志,2019,35(10):1586-1589. [50] 李坤彬,吴志远,温小鹏,等.小脑间歇性θ短阵脉冲刺激对小脑卒中吞咽障碍的影响及机制[J].中华物理医学与康复杂志,2021,43(12):1100-1104. [51] 罗雅丽,陈劲松,陈莎莎,等.不同电磁刺激方案干预脑卒中后假性球麻痹吞咽障碍的对比研究[J].中华全科医学,2024,22(4):669-673. [52] 马明,杨玺,蔡倩,等.重复性外周磁刺激联合吞咽功能训练治疗脑卒中后咽期吞咽障碍的疗效观察[J].中华物理医学与康复杂志,2017, 39(10):749-752. [53] 孟凤珠,温凯,高华,等.肌电生物反馈联合康复训练治疗脑梗死后吞咽障碍疗效分析[J].神经损伤与功能重建,2017,12(5):445-446. [54] 闵瑜,颜海霞,黄志锐,等.肌电生物反馈治疗脑卒中后吞咽障碍的疗效观察[J].中华物理医学与康复杂志,2014,36(8):583-586. [55] 欧阳瑶,朱其秀,阎文静,等.高频重复经颅磁刺激对单侧大脑半球卒中后患者吞咽障碍的影响[J].中华物理医学与康复杂志,2019,41(4):261-265. [56] 饶金柱,李华娇,王晶,等.重复经颅磁刺激联合神经肌肉电刺激治疗卒中后吞咽障碍的疗效分析[J].神经损伤与功能重建,2021,16(7):373-377. [57] 宋晶,王笑丰,李永,等.高频、低频rTMS作用健侧半球吞咽皮质代表区对老年脑卒中后吞咽障碍的影响对比[J].中国老年学杂志,2023, 43(16):3863-3867. [58] 苏文华,阎文静,钟明华,等.神经肌肉电刺激对脑卒中后吞咽障碍患者吞咽功能及其表面肌电图的影响[J].中华物理医学与康复杂志, 2015,37(3):183-186. [59] 孙龚卫,杨柳,孙小星.高频rTMS作用健侧半球吞咽皮质代表区联合吞咽康复训练治疗脑卒中后吞咽障碍的临床研究[J].中国康复,2022, 37(1):7-11. [60] 孙莉,王舒,沈晓艳.不同强度经颅直流电刺激治疗真性球麻痹吞咽障碍的疗效观察[J].神经损伤与功能重建,2022,17(10):587-590. [61] 王舒,沈晓艳,莫丹,等.经颅直流电刺激联合吞咽训练对脑卒中后吞咽功能障碍的临床疗效观察[J].神经损伤与功能重建,2019,14(4):209-211. [62] 王扬,周达岸.神经肌肉电刺激对卒中后吞咽障碍的治疗作用[J].广东医学,2020,41(19): 1999-2004. [63] 王志勇,柏俊惠,成柯岭,等.下颌舌骨肌外周磁刺激联合中枢磁刺激对脑卒中后吞咽障碍的影响[J].中华物理医学与康复杂志,2023,45(12): 1119-1124. [64] 吴晶,张伟,陈焱强,等.双侧重复经颅磁刺激联合肌电生物反馈治疗脑卒中吞咽障碍的临床研究[J].中国康复,2023,38(6):323-327. [65] 吴秀香,李晓丹,王莉,等.iTBS经颅磁刺激治疗缺血性脑卒中后吞咽障碍随机对照临床研究[J].新疆医科大学学报,2020,43(9):1228-1232. [66] 夏海桃,佟强,王爱凤,等.高频经颅磁刺激联合康复训练对脑卒中后吞咽障碍患者表面肌电图的影响[J].中华保健医学杂志,2024,26(1):30-33. [67] 徐丹妮,金敏敏,王中莉,等.重复经颅磁刺激辅助治疗对脑卒中患者吞咽障碍的疗效观察[J].浙江医学,2023,45(11):1186-1189. [68] 徐倩,韩珍真,朱冬燕,等.健侧高频重复经颅磁刺激结合生物反馈下的空吞咽训练对脑卒中后吞咽障碍的影响[J].中华物理医学与康复杂志,2024,46(1):17-22. [69] 杨晨,张俊,孙菲,等.经颅直流电刺激治疗脑卒中后真假性球麻痹吞咽障碍的疗效观察[J].中华物理医学与康复杂志,2020,42(3):199-204. [70] 杨玺,蔡倩,徐亮,等.重复经颅磁刺激联合表面肌电生物反馈对脑卒中后吞咽障碍患者吞咽功能的影响[J].中华物理医学与康复杂志, 2022,44(7):603-606. [71] 张祎辰,王强,孟萍萍,等.不同频率健侧半球重复经颅磁刺激对脑卒中后吞咽障碍的影响[J].中华物理医学与康复杂志,2020,42(4):295-299. [72] 张云,马明,蔡倩,等.外周磁刺激与神经肌肉电刺激治疗脑卒中后咽期吞咽障碍的疗效对比[J].中华物理医学与康复杂志,2018,40(6):424-427. [73] 赵殿兰,王强,孟萍萍,等.强化神经肌肉电刺激对脑卒中吞咽障碍患者吞咽功能及舌骨喉复合体运动速度的影响[J].中华物理医学与康复杂志,2017,39(6):427-432. [74] 赵静,闫莹莹.双侧高频重复经颅磁刺激治疗单侧脑卒中后吞咽障碍的临床研究[J].中西医结合心脑血管病杂志,2022,20(23):4372-4375. [75] 郑婵娟,夏文广,张阳普,等.神经肌肉电刺激联合吞咽训练治疗脑卒中后吞咽障碍的疗效观察[J].中华物理医学与康复杂志,2013,35(3): 201-204. [76] 钟立达,刘惠宇,鲍晓,等.小脑重复经颅磁刺激治疗脑卒中后吞咽障碍的疗效观察[J].中国康复,2021,36(2):106-108. [77] 窦祖林.吞咽障碍的规范化评估与治疗中值得注意的几个问题[J].中国康复医学杂志,2020, 35(3):257-259. [78] QIU H, LI F, ZHANG S, et al. Surface electromyographic characteristics of forearm muscles after ulnar and radius fracture inchildren. Front Pediatr. 2023;11:1143047. [79] 谢逍,魏继鸿,刘双,等.低频脉冲电刺激联合摄食-吞咽训练在AIS后吞咽障碍的应用及疗效[J].西部医学,2023,35(6):875-880. [80] VELDMAN MP, MAURITS NM, ZIJDEWIND I, et al. Somatosensory electrical stimulation improves skill acquisition, consolidation, and transfer by increasing sensorimotor activity and connectivity. J Neurophysiol. 2018;120(1):281-290. [81] ROQUE C, PINTO N, VAZ PATTO M, et al. Astrocytes contribute to the neuronal recovery promoted by high-frequency repetitive magnetic stimulation in in vitro models of ischemia. J Neurosci Res. 2021; 99(5):1414-1432. [82] 俞风云,朱玉连,梁思捷,等.经颅和外周磁刺激治疗脑卒中后上肢运动功能障碍的随机对照研究[J].中国康复医学杂志,2021,36(5):538-545. [83] FEURRA M, BLAGOVECHTCHENSKI E, NIKULIN VV, et al. State-dependent effects of transcranial oscillatory currents on the motor system during action observation. Sci Rep. 2019;9(1):12858. [84] MRACHACZ-KERSTING N, STEVENSON AJT, JøRGENSEN HRM, et al. Brain state-dependent stimulation boosts functional recovery following stroke. Ann Neurol. 2019;85(1):84-95. [85] 朱光跃,陈思韵,霍聪聪,等.外周联合中枢双靶磁刺激促进脑卒中运动功能障碍康复专家共识[J].中国康复医学杂志,2023,38(7):880-884. [86] QI F, NITSCHE MA, REN X, et al. Top-down and bottom-up stimulation techniques combined with action observation treatment in stroke rehabilitation: a perspective. Front Neurol. 2023; 14:1156987. [87] CARSON RG, BUICK AR. Neuromuscular electrical stimulation-promoted plasticity of the human brain. J Physiol. 2021;599(9):2375-2399. [88] 袁佳,冯文锋,豆运香,等.基于神经电生理探讨重复外周磁刺激治疗腰椎间盘突出症[J].实用医学杂志,2024,40(12):1665-1670. [89] KENNEY-JUNG DL, BLACKER CJ, CAMSARI DD, et al. Transcranial direct current stimulation: mechanisms and psychiatric applications. Child Adolesc Psychiatr Clin N Am. 2019;28(1):53-60. [90] 艾一楠,李莉莉,尹明宇,等.不同治疗时机的经颅直流电刺激治疗脑卒中后认知障碍的初步研究[J].中国康复医学杂志,2021,36(3):315-321. [91] 刘员辰,张立新.经颅直流电刺激治疗卒中后认知障碍的相关研究进展[J].康复学报,2024, 34(3):304-311. [92] CHERVYAKOV AV, CHERNYAVSKY AY, SINITSYN DO, et al. Possible mechanisms underlying the therapeutic effects of transcranial magnetic stimulation. Front Hum Neurosci. 2015;9:303. [93] SHENG R, CHEN C, CHEN H, et al. Repetitive transcranial magnetic stimulation for stroke rehabilitation: insights into the molecular and cellular mechanisms of neuroinflammation. Front Immunol. 2023;14:1197422. [94] 尚莹春,张涛.重复经颅磁刺激对认知功能的作用及其分子机理的研究进展[J].电工技术学报,2021,36(4):685-692. [95] 柯嘉洽,邹晓佩,王春燕,等.经颅直流电刺激和经颅磁刺激在脑卒中上肢运动功能恢复的应用进展[J].中国神经精神疾病杂志,2021, 47(1):50-55. |
| [1] | Yang Yuanyuan, Zhou Shanshan, Cheng Xiaofei, Feng Luye, Tang Jiqin. Network meta-analysis of non-invasive brain stimulation in the treatment of lower limb motor dysfunction after stroke [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1008-1018. |
| [2] | Wang Zheng, Cheng Ji, Yu Jinlong, Liu Wenhong, Wang Zhaohong, Zhou Luxing. Progress and future perspectives on the application of hydrogel materials in stroke therapy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-10. |
| [3] | Wang Juan, Wang Guanglan, Zuo Huiwu. Efficacy of exercise therapy in the treatment of anterior cruciate ligament reconstruction patients: #br# a network meta-analysis #br# [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1714-1726. |
| [4] | Wang Mi, Ma Shujie, Liu Yang, Qi Rui. Identification and validation of characterized gene NFE2L2 for ferroptosis in ischemic stroke [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1466-1474. |
| [5] | Gao Yang, Qin Hewei, Liu Dandan. ACSL4 mediates ferroptosis and its potential role in atherosclerotic cardiovascular disease [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1239-1247. |
| [6] | Yang Bo, Pan Xinfang, Chang Liuhui, Ni Yong. Correlation of echocardiographic parameters with disability at 3 months after acute ischemic stroke [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7544-7551. |
| [7] | Chen Ying, Guo Xiaojing, Mo Xueni, Ma Wei, Wu Shangzhi, Li Xiangling, Xie Tingting. Analysis of diagnostic biomarkers for ischemic stroke and experimental validation of targeted cuproptosis related genes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7562-7570. |
| [8] | Zhu Chuanxi, Qiu Long, Li Lingxu, Ji Guangcheng. Chinese herbal prescription combined with head acupuncture exercise therapy improves limb spasticity in rats with ischemic stroke [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7571-7577. |
| [9] | Tian Jinxin, Zhao Yuxin, Hu Tong, Cui Tiantian, Ma Lihong. Effects of different transcranial magnetic stimulation modes on refractory depression in adults: a network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7639-7648. |
| [10] | Wang Xuesong, Wang Yue, Xu Yan, Zeng Wenhui, Lu Wenming, Tang Xingkun, Chen Wenjie, Ye Junsong. Brain-computer interface combined with different therapies for limb dysfunction in stroke patients: effectiveness and mechanism analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6538-6546. |
| [11] | Wang He, Yu Shaohong, . Meta-analysis of transcranial direct current stimulation in improving lower limb motor dysfunction in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6556-6565. |
| [12] | Ping Xingfeng, Huang Zongxuan, Li Kai, Xie Guangmin, Lyu Junying. Regularity of prescriptions for ischemic stroke based on latent structure combined with association rules [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6277-6284. |
| [13] | Wang Jiaru, Zhang Ying, Yang Yong, Qi Wen, Xiao Huaye, Ma Qiuping, Yang Lianzhao, Luo Ziwei, He Yaqing, Zhang Jiangyin, Wei Jiawen, Meng Yuan, Tan Silian. Systematic review of machine learning models for predicting functional recovery and prognosis in stroke [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6317-6325. |
| [14] | Wang Zhifeng, Yang Jiao, Xi Yujiang, Xu Shuangfeng, Shi Ting, Lan Junfeng, Hao Zhihui, He Pengfen, Yang Aiming, Pan Pan, Wang Jian. Biomarkers affecting the progression of mild to moderate cognitive impairment after stroke: #br# a non-targeted metabolomics analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5116-5126. |
| [15] | Cao Haijie, Song Huijie, Sun Yalu, Zhang Guangyou, Li Xiang. A wearable exoskeleton with posture feedback improves abnormal gait in patients with stroke [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5127-5133. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||