Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (12): 2590-2604.doi: 10.12307/2025.372
Previous Articles Next Articles
Effect of low-volume high-intensity interval training on cardiovascular risk factor in obese or overweight populations: a Meta-analysis
Li Xiupeng1, Su Yuying1, 2, Wang Yuetong3, Peng Liang1, Wang Yida4, Jing Wen1
- 1School of Physical Education, Bohai University, Jinzhou 121013, Liaoning Province, China; 2School of Physical Training, 3School of Education, Beijing Sport University, Beijing 100086, China; 4College of Physical Education and Health, Dalian University of Technology, Dalian 116024, Liaoning Province, China
-
Received:2024-04-18Accepted:2024-05-23Online:2025-04-28Published:2024-09-11 -
Contact:Su Yuying, PhD, School of Physical Education, Bohai University, Jinzhou 121013, Liaoning Province, China; School of Physical Training, Beijing Sport University, Beijing 100086, China -
About author:Li Xiupeng, School of Physical Education, Bohai University, Jinzhou 121013, Liaoning Province, China -
Supported by:Liaoning Provincial Department of Education Basic Research Project - Youth Project, No. LJKQR20222558 (to SYY); National Social Science Foundation of China - General Program, No. 22BTY080 (to JW)
CLC Number:
Cite this article
Li Xiupeng, Su Yuying, Wang Yuetong, Peng Liang, Wang Yida, Jing Wen. Effect of low-volume high-intensity interval training on cardiovascular risk factor in obese or overweight populations: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(12): 2590-2604.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
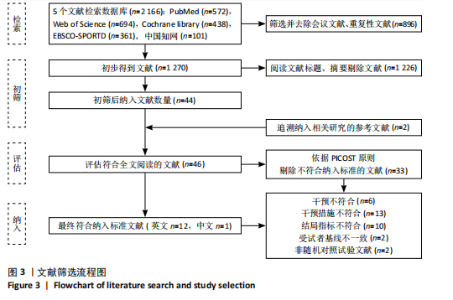
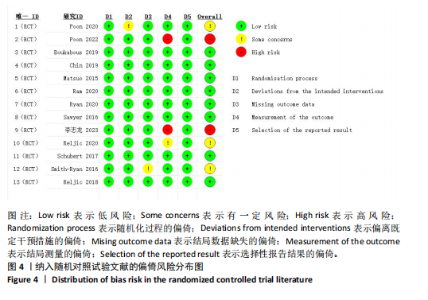
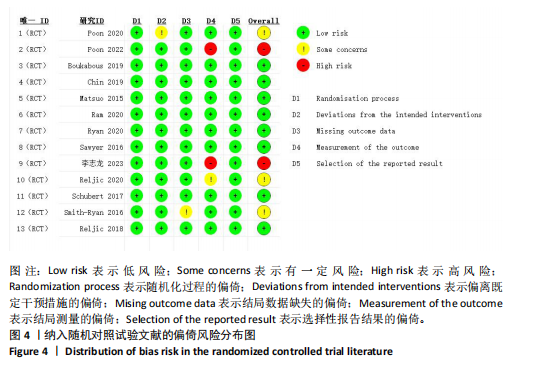
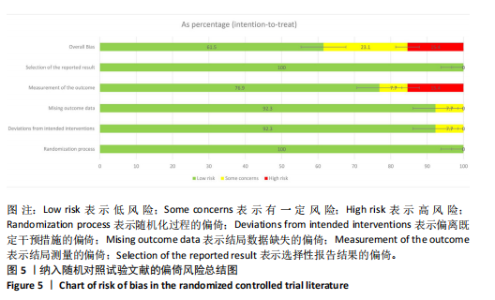
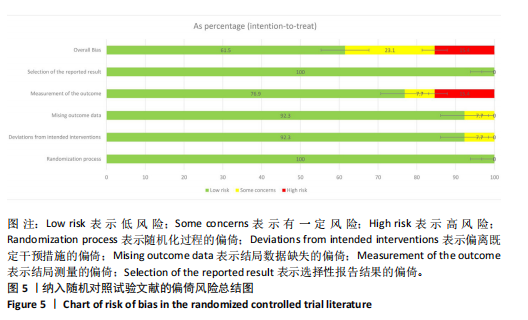
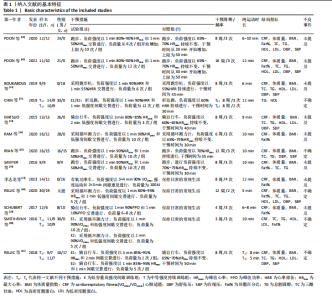
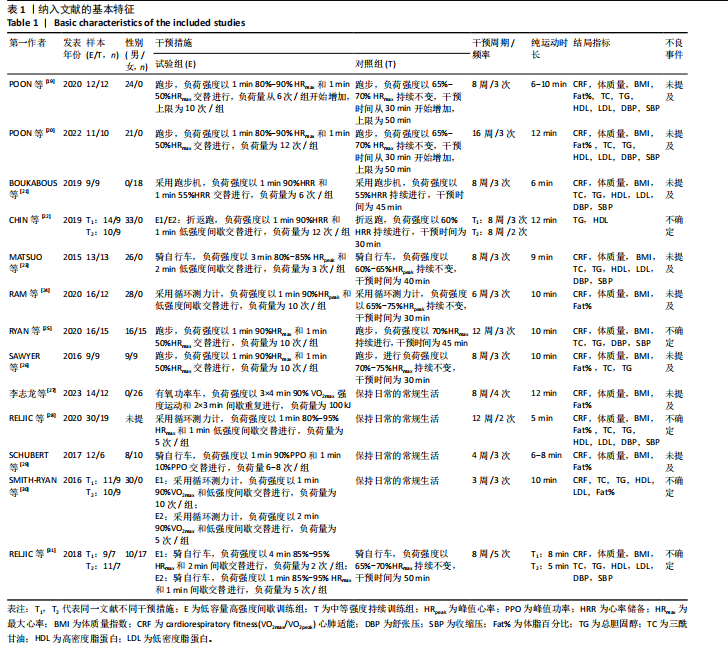
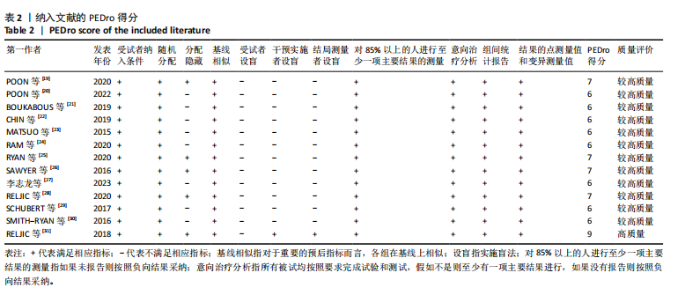
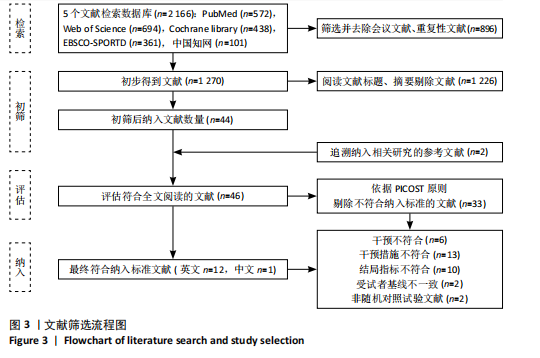
2.1 文献检索结果 通过检索词从5个数据库中共检索出2 166篇文献,经阅读题目和摘要去除非低容量高强度间歇训练干预文献后得到46篇研究文献,最后阅读全文剔除儿童青少年干预、非肥胖/超重以及伴有其他严重疾病或并发症、物理或药物治疗、急性运动干预、非随机对照试验和对照组干预不符的文献33篇,最终纳入13篇文献[19-31],包括英文12篇[19-26,28-31],中文1篇[27],见图3。 2.2 纳入文献基本特征 纳入的13篇文献中,肥胖或超重患者共包含349例[19-31]。其中,试验组全部采用低容量高强度间歇训练,方案采用自行车、循环测力计以及通过跑步和折返跑的形式进行运动。对照组采用与试验组一致的运动方式进行中等强度持续训练。干预周期为3-16周,低容量高强度间歇训练纯运动时长为5-12 min。纳入文献基本特征见表1。 2.3 纳入文献的质量评价结果 根据PEDro量表标准,对被纳入研究文献进行文章质量评价。共计筛选出13篇文献[19-31],其中按照评分标准判定为较高质量文献的有12篇,得分在6分及以上即为较高质量文献。这些文献的评分多为6-8分,其中仅有1篇评为9分的高质量文献。综合而言,所涉及文献的纳入标准较为严格,整体上文献的方法学较为可靠,质量较高,见表2。 RoB 2.0工具评估的偏倚风险结果如图4,5所示。其中,研究均为随机对照试验,对于识别或招募偏倚和结局数据缺失的偏倚发现均有92.3%被评为“低风险”以及7.7%为“有一定风险”。对于结局测量的偏倚发现有76.0%被评为“低风险”,7.7%为“有一定风险”以及"
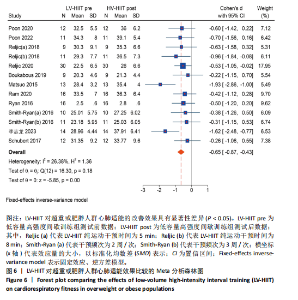
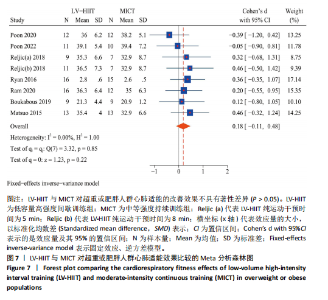
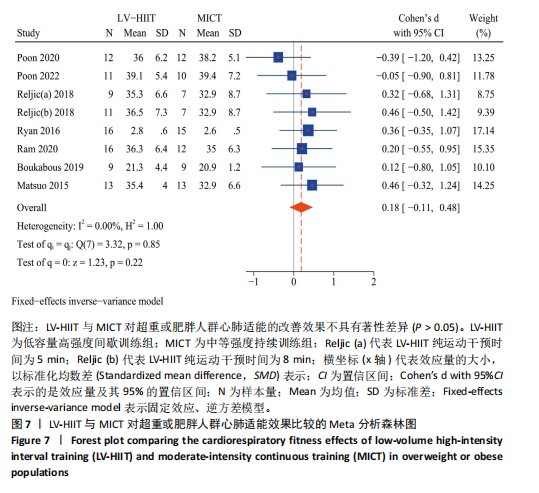
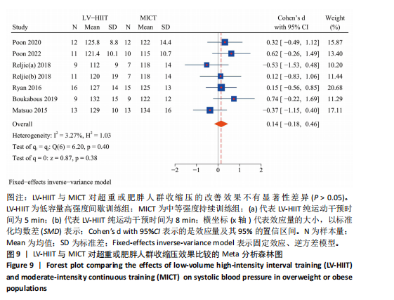
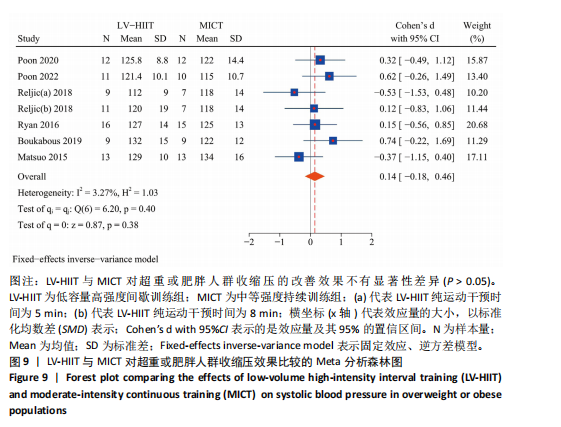
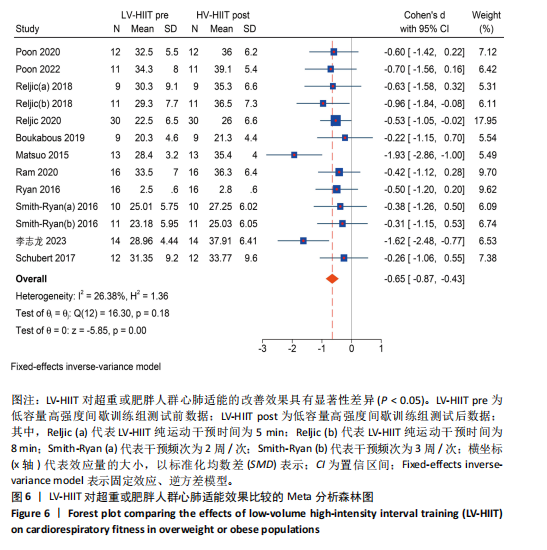
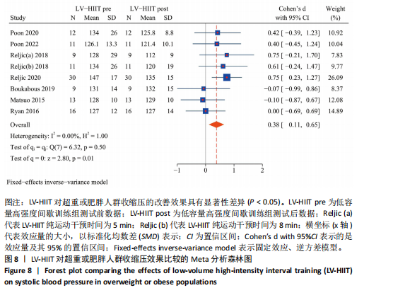
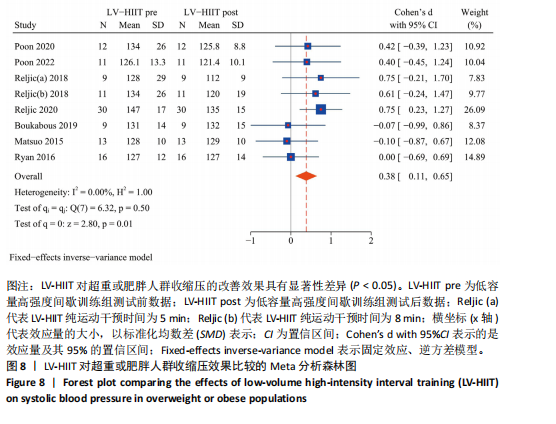
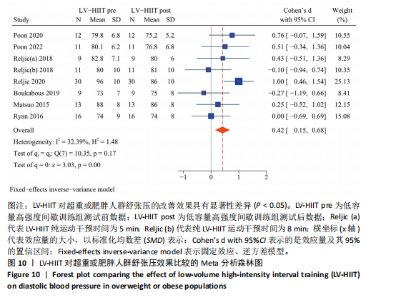
15.4%为“高风险”。文献整体偏倚分析发现,61.5%被评为“低风险”,23.1%为“有一定风险”以及15.4%为“高风险”。 2.4 Meta分析结果 2.4.1 低容量高强度间歇训练对肥胖或超重人群心血管功能干预效果的Meta分析心肺适能:低容量高强度间歇训练干预共纳入11项研究的13个效应量指标,共计患者174例[19-21,23-25,27-31]。研究间存在低度异质性(I2=26.38%),故选取固定效应模型。低容量高强度间歇训练合并效应量(SMD=-0.65,95%CI:-0.87至-0.43,P < 0.05)具有显著性意义,表明低容量高强度间歇训练干预可以改善心肺适能效果,见图6。低容量高强度间歇训练与中等强度持续训练相比共纳入7项研究的8个效应量指标,共计患者175例[19-20,23-24,29-31]。研究间不存在异质性(I2=0.00%),故选取固定效应模型。低容量高强度间歇训练与中等强度持续训练合并效应量(SMD=0.18,95%CI:-0.11-0.48,P > 0.05)不具有显著性意义,表明两者干预效果无显著性差异,见图7。 收缩压:低容量高强度间歇训练干预对共纳入7项研究的8个效应量指标,共计患者111例[19-21,23,25,28,31]。研究间不存在异质性(I2=0.00%),故选取固定效应模型。低容量高强度间歇训练合并效应量(SMD=0.38,95%CI:0.11-0.65,P < 0.05)具有显著性意义,表明低容量高强度间歇训练干预可以改善收缩压效果,见图8。低容量高强度间歇训练与中等强度持续训练相比共纳入6篇研究的7个效应量指标[19-21,23,25,31],共计患者147例。研究间存在低度异质性(I2=3.27%),故选取固定效应模型。低容量高强度间歇训练与中等强度持续训练合并效应量(SMD=0.14,95%CI:-0.18-0.46,P > 0.05)不具有显著性意义,表明两者比较干预效果无显著性差异,见图9。 舒张压:低容量高强度间歇训练干预对共纳入7项研究的8个效应量指标,共计患者111例[19-21,23,25,28,31]。研究间存在低度异质性(I2=32.29%),故选取固定效应"
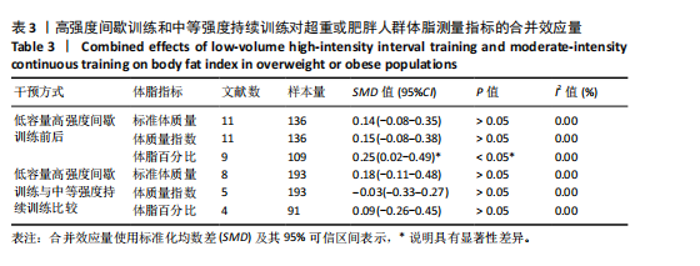
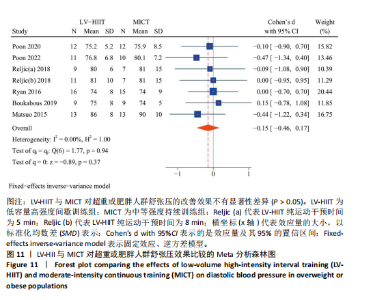
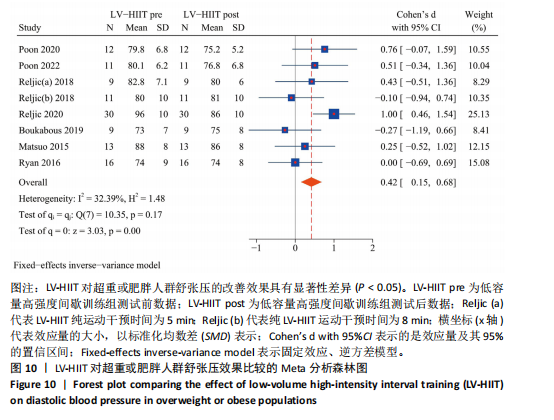
模型。低容量高强度间歇训练合并效应量(SMD=0.42,95%CI:0.15-0.68,P < 0.05)具有显著性意义,表明低容量高强度间歇训练干预可以改善舒张压效果,见图10。低容量高强度间歇训练与中等强度持续训练相比共纳入6项研究的7个效应量指标,共计患者147例[19-21,23,25,31]。研究间不存在异质性(I2=0.00%),故选取固定效应模型。低容量高强度间歇训练与中等强度持续训练合并效应量(SMD=-0.15,95%CI:-0.46-0.17,P > 0.05)不具有显著性意义,表明两者比较干预效果无显著性差异,见图11。 综合来看,低容量高强度间歇训练可以有效提升肥胖或超重人群心肺适能水平和促使肥胖或超重人群收缩压和舒张压水平降低,并恢复到血压正常值范围。低容量高强度间歇训练与中等强度持续训练相比发现,两组干预对心血管功能指标的改善效果相似,侧面说明短时间的低容量高强度间歇训练相比于长时间的中等强度持续训练更具有时间效益。 2.4.2 低容量高强度间歇训练对肥胖或超重人群体脂干预效果的Meta分析结果 见表3。 标准体质量:低容量高强度间歇训练干预研究纳入11项研究的12个效应量,共计患者136例[19-21,23-29,31]。研究间不存在异质性(I2=0.00%),故选取固定效应模型。低容量高强度间歇训练干预效果(SMD=0.14,95%CI:-0.08-0.35,P > 0.05)不具有显著性意义,表明合并效应量不具有显著性效果。低容量高强度间歇训练与中等强度持续训练相比研究纳入9项研究的10个效应量,共计患者193例[19-26,31]。研究间不存在异质性(I2=0.00%),故选取固定效应模型。低容量高强度间歇训练与中等强度持续训练干预效果(SMD=0.18,95%CI:-0.11-0.48,P > 0.05)不具有显著性意义,表明合并效应量不具有显著性效果。 体质量指数:低容量高强度间歇训练干预研究纳入11项研究的12个效应量,共计患者136例[19-21,23-29,31]。研究间不存在异质性(I2=0.00%),故选取固定效应模型。低容量高强度间歇训练干预效果(SMD=0.15,"
95%CI:-0.08-0.38,P > 0.05)不具有显著性意义,表明合并效应量不具有显著性效果。低容量高强度间歇训练与中等强度持续训练相比研究纳入8项研究的10个效应量,共计患者193例[19-21,23-26,31]。研究间不存在异质性(I2=0.00%),故选取固定效应模型。低容量高强度间歇训练与中等强度持续训练干预效果(SMD=-0.03,95%CI:-0.33-0.27,P > 0.05)不具有显著性意义,表明合并效应量不具有显著性效果。 体脂百分比:低容量高强度间歇训练干预研究纳入8项研究的9个效应量,共计患者109例[19-20,24,26-30]。研究间不存在异质性(I2=0.00%),故选取固定效应模型。低容量高强度间歇训练干预效果(SMD=0.25,95%CI:0.02-0.49,P < 0.05)具有显著性意义,表明合并效应量具有显著性效果。低容量高强度间歇训练与中等强度持续训练相比研究纳入5项研究的4个效应量,共计患者91例[19,20,24-26]。研究间不存在异质性(I2=0.00%),故选取固定效应模型。低容量高强度间歇训练与中等强度持续训练干预效果(SMD=0.09,95%CI:-0.26-0.45,P > 0.05)不具有显著性意义,表明合并效应量不具有显著性效果。 综合来看,低容量高强度间歇训练可以显著降低超重或肥胖人群体脂百分比(P < 0.05),但对标准体质量和身体质量分数改善无效果(P > 0.05)。低容量高强度间歇训练与中等强度持续训练相比对体脂干预效果3个指标方面均无显著优势(P > 0.05),说明低容量高强度间歇训练与中等强度持续训练干预效果相同,因此研究推断可能存在潜在的优势,但由于纳入相关研究较少,未来仍需相关研究验证在该方面的有效性。目前低容量高强度间歇训练在改善体脂方面效果虽然具有潜在优势,但仅在改善体脂百分比方面具有显著性效果,且支撑相关结果的试验数据偏少,故不进行低容量高强度间歇训练与中等强度持续训练两者间亚组分析、敏感性分析以及发表偏倚检验。 2.4.3 低容量高强度间歇训练对肥胖或超重人群血脂干预效果的Meta分析结果 见表4。"
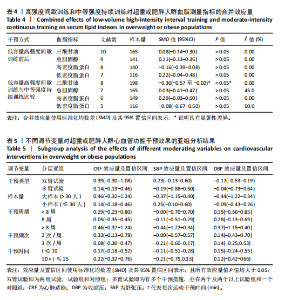
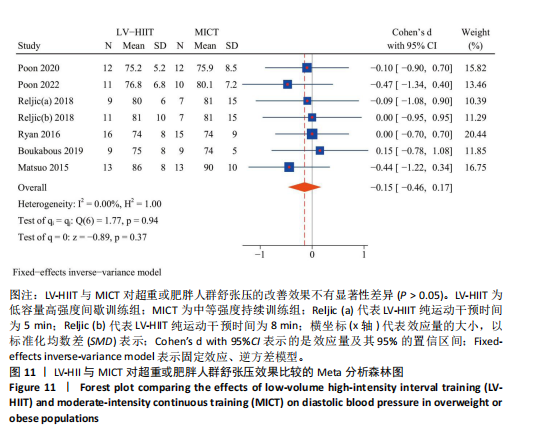
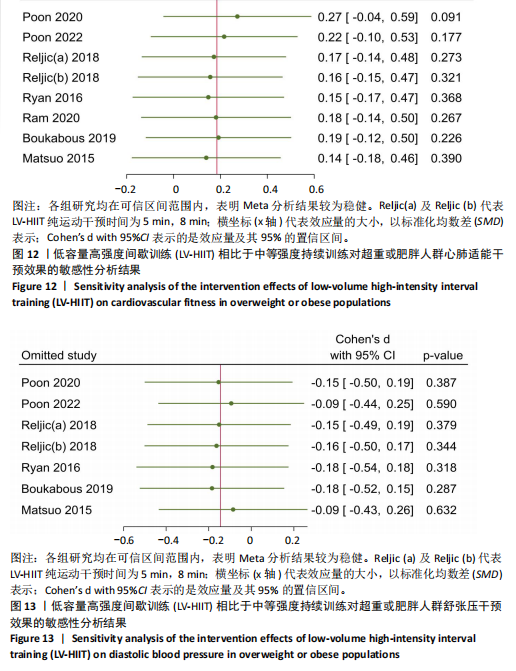
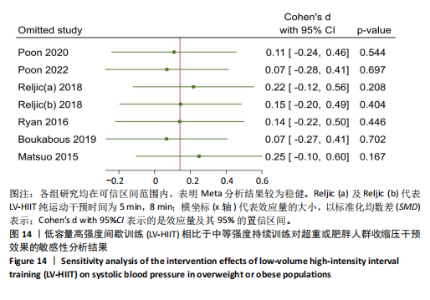
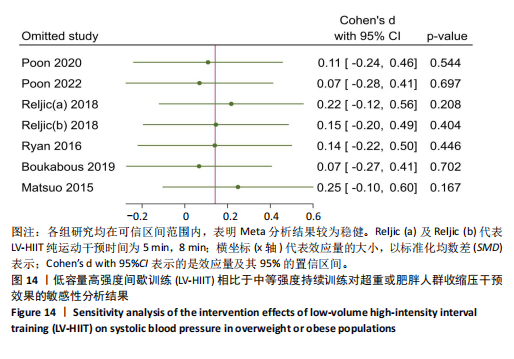
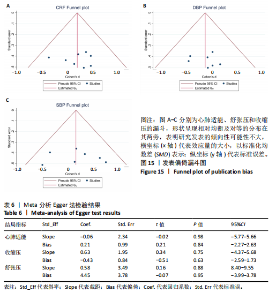
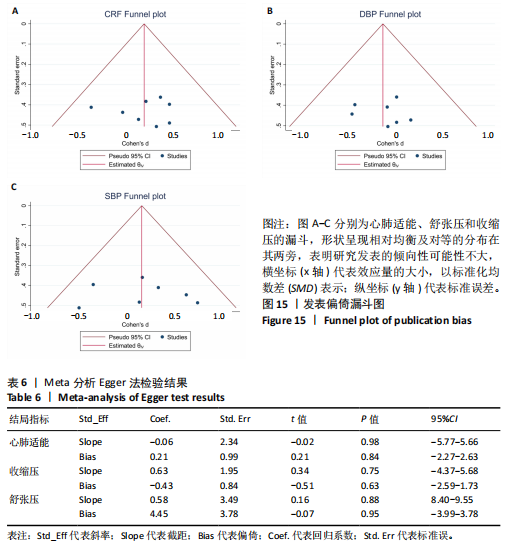
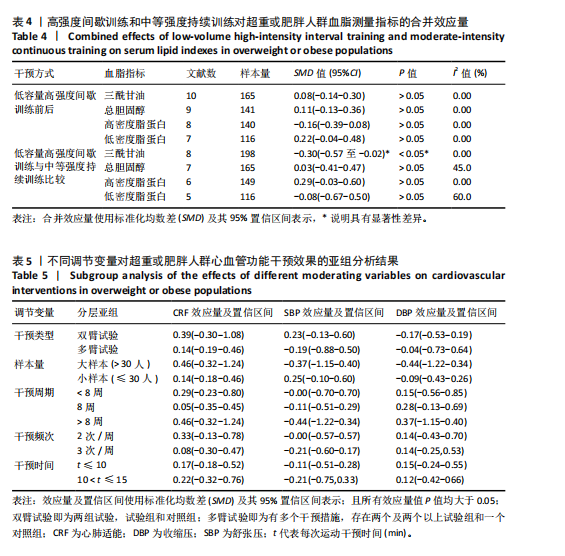
三酰甘油:低容量高强度间歇训练干预研究纳入10项研究的13个效应量,共计患者165例[19-23,25-26,28,30-31]。 研究间存在异质性(I2=0.00%),故选取固定效应模型。低容量高强度间歇训练干预效果(SMD=0.08,95%CI:-0.14-0.30,P > 0.05)不具有显著性意义,表明合并效应量不具有显著性效果。低容量高强度间歇训练与中等强度持续训练相比共纳入8项研究的10个效应量,共计患者198例[19-23,25-26,31]。研究间不存在异质性(I2=0.00%),故选取固定效应模型。低容量高强度间歇训练与中等强度持续训练干预效果(SMD=-0.30,95%CI:-0.57至-0.02,P < 0.05)具有显著性意义,表明合并效应量具有显著性效果。 总胆固醇:低容量高强度间歇训练干预研究纳入9项研究的11个效应量,共计患者141例[19-21,23,25-26,28,30-31]。研究间不存在异质性(I2=0.00%),故选取固定效应模型。低容量高强度间歇训练干预效果(SMD=0.11,95%CI:-0.13-0.36,P > 0.05)不具有显著性意义,表明合并效应量不具有显著性效果。低容量高强度间歇训练与中等强度持续训练相比共纳入7项研究的8个效应量,共计患者165例[19-21,23,25-26,31]。研究间存在低度异质性(I2=45.0%),故选取固定效应模型。低容量高强度间歇训练与中等强度持续训练干预效果(SMD=0.03,95%CI:-0.41-0.47,P > 0.05)不具有显著性意义,表明合并效应量不具有显著性效果。 高密度脂蛋白:低容量高强度间歇训练干预研究纳入8项研究的11个效应量,共计患者140例[19-23,28,30-31]。研究间不存在异质性(I2=0.00%),故选取固定效应模型。低容量高强度间歇训练干预效果(SMD=-0.16,95%CI:-0.39-0.08,P > 0.05)不具有显著性差异。低容量高强度间歇训练与中等强度持续训练相比共纳入6项研究的8个效应量,共计患者149例[19-23,31]。研究间不存在异质性(I2=0.00%),故选取固定效应模型。低容量高强度间歇训练与中等强度持续训练干预效果(SMD=0.29,95%CI:-0.03-0.60,P > 0.05)不具有显著性意义,表明合并效应量不具有显著性效果。 低密度脂蛋白:低容量高强度间歇训练干预研究纳入7项研究的9个效应量,共计患者116例[19-21,23,28,30-31]。研究间不存在异质性(I2=0.00%),故选取固定效应模型。低容量高强度间歇训练干预效果(SMD=0.22,95%CI:-0.04-0.48,P > 0.05)不具有显著性差异。低容量高强度间歇训练与中等强度持续训练相比共纳入5项研究的6个效应量,共计患者116例[19-21,23,31]。研究间存在中度异质性(I2=60.0%),故选取随机效应模型。低容量高强度间歇训练与中等强度持续训练干预效果(SMD=-0.08,95%CI:-0.67-0.50,P > 0.05)不具有显著性意义,表明合并效应量不具有显著性效果。 综上所述,低容量高强度间歇训练对超重或肥胖人群的三酰甘油、总胆固醇、高密度脂蛋白和低密度脂蛋白指标没有改善效果(P > 0.05)。但两者对比发现,中等强度持续训练对三酰甘油干预效果优于低容量高强度间歇训练(P < 0.05),但在改善总胆固醇、高密度脂蛋白和低密度脂蛋白方面两者效果相当,因此研究推断可能存在具有中等强度持续训练类似的效果,但由于纳入相关研究较少,未来仍需相关研究验证在该方面的有效性。目前低容量高强度间歇训练在改善血脂方面的效果仍待考究,但支撑相关结果的试验数据偏少,故不进行低容量高强度间歇训练与中等强度持续训练两者间亚组分析、敏感性分析以及发表偏倚检验。 2.4.4 亚组分析结果 设置调节变量对心脏适能、舒张压、收缩压指标进行低容量高强度间歇训练与中等强度持续训练亚组分析,经研究发现两组间异质性均小于50%,故合并效应量选取固定效应模型,见表5。干预类型方面,双臂试验和多臂试验对3个指标干预效果均无显著优势。样本量大小方面,小样本和大样本对3个指标干预效果均无显著优势。干预周期方面,干预小于8周、8周以及大于8周干预对3个指标干预效果均无显著优势。干预频次方面,干预2次/周和3次/周对3个指标均干预效果无显著优势。干预时间方面,干预t≤10 min和10 min < t≤15 min两者干预效果相似,且低容量高强度间歇训练更具有时间效益。 2.5 敏感性分析结果 为保证Meta分析结果的可靠性,文章进行了Leave-One-Out敏感性分析,即逐一移除每项研究并重新估算总体合并效应量的效果,以此考察任一单项研究对总体结果的影响,结果如图12-14所示。结果显示,有3项指标整体效应量在逐一剔除仍表现为一致性。这说明该Meta分析的结论对于个别研究影响不敏感,结果较为稳定,"
| [1] 李靖,张漓.健康中国建设中慢性病防治体医融合的试点经验、现实挑战及应对策略[J].体育科学,2020,40(12):73-82. [2] BREEN C, O CONNELL J, GEOGHEGAN J, et al. Obesity in adults: a 2022 adapted clinical practice guideline for Ireland. Obes Facts. 2022;15(6):736-752. [3] ELAGIZI A, KACHUR S, LAVIE CJ, et al. An overview and update on obesity and the obesity paradox in cardiovascular diseases. Prog Cardiovasc Dis. 2018;61(2):142-150. [4] PICHE M, TCHERNOF A, DESPRE J. Obesity phenotypes, diabetes, and cardiovascular diseases. Circ Res. 2020;126(11):1477-1500. [5] HORWIC TB, FONAROW GC, CLARK AL. Obesity and the obesity paradox in heart failure. Prog Cardiovasc Dis. 2018;61(2): 151-156. [6] NCD Risk Factor Collaboration (NCD-RiskC). Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet. 2024;403(10431):1027-1050. [7] DENG F, LV JH, WANG HL, et al. Expanding public health in China: an empirical analysis of healthcare inputs and outputs. Public health. 2017;142:73-84. [8] KEATING SE, MACHAN EA, O’Connor HT, et al. Continuous exercise but not high intensity interval training improves fat distribution in overweight adults. J Obes. 2014;2014:834865. [9] GHARDASHI-AFOUSI A, HOLISAZ MT, SHIRVANI H, et al. The effects of low-volume high-intensity interval versus moderate intensity continuous training on heart rate variability, and hemodynamic and echocardiography indices in men after coronary artery bypass grafting: a randomized clinical trial study. ARYA Atheroscler. 2018;14(6):260. [10] WANG Y, FAN C, CHENG L, et al. A comparative analysis of energy expenditure and substrate metabolism in male university students with overweight/obesity: Tabata vs HIIT and MICT. Front Endocrinol (Lausanne). 2024; 15:1323093. [11] WANG Y, WANG S, MENG X, et al. Effect of high-intensity interval training and moderate-intensity continuous training on cardiovascular risk factors in adolescents: Systematic review and meta-analysis of randomized controlled trials. Physiol Behav. 2024;275:114459. [12] WELSH A, HAMMAD M, PINA IL, et al. Obesity and cardiovascular health. Eur J Prevent Cardiol. 2024. doi: 10.1016/j.beem. 2013.01.004. [13] GIBALA MJ, LITTLE JP, MACDONALD MJ, et al. Physiological adaptations to low‐volume, high‐intensity interval training in health and disease. J Physiol. 2012;590(5): 1077-1084. [14] SABAG A, LITTLE JP, JOHNSON NA. Low‐volume high‐intensity interval training for cardiometabolic health. J Physiol. 2022; 600(5):1013-1026. [15] 高思垚,吕万刚,聂应军.不同运动方式对中国超重或肥胖人群代谢指标影响的元分析[J].中国体育科技,2021,57(10): 46-54. [16] VIANA RB, NAVES JPA, COSWIG VS, et al. Is interval training the magic bullet for fat loss? A systematic review and meta-analysis comparing moderate-intensity continuous training with high-intensity interval training (HIIT). Br J Sports Med. 2019;53(10):655-664. [17] MARTIN-SMITH R, COX A, BUCHAN DS, et al. High intensity interval training (HIIT) improves cardiorespiratory fitness (CRF) in healthy, overweight and obese adolescents: a systematic review and meta-analysis of controlled studies. Int J Environ Res Public Health.2020;17(8):2955. [18] YIN M, LI H, BAI M, et al. Is low-volume high-intensity interval training a time-efficient strategy to improve cardiometabolic health and body composition? A meta-analysis. Appl Physiol Nutr Metab. 2024;49(3):273-292. [19] POON ET, LITTLE JP, SIT CH, et al. The effect of low-volume high-intensity interval training on cardiometabolic health and psychological responses in overweight/obese middle-aged men. J Sports Sci. 2020;38(17):1997-2004. [20] POON ET, SIU PM, WONG PIPIT W, et al. Alternating high-intensity interval training and continuous training is efficacious in improving cardiometabolic health in obese middle-aged men. J Exerc Sci Fit. 2022;20(1):40-47. [21] BOUKABOUS I, MARCOTTE-CHENARD A, AMAMOU T, et al. Low-volume high-intensity interval training versus moderate-intensity continuous training on body composition, cardiometabolic profile, and physical capacity in older women. J Aging Phys Act. 2019;27(6):879-889. [22] CHIN EC, YU AP, LAI CW, et al. Low-frequency HIIT improves body composition and aerobic capacity in overweight men. Med Sci Sports Exerc. 2020;52(1):56-66. [23] MATSUO T, SO R, SHIMOJO N, et al. Effect of aerobic exercise training followed by a low-calorie diet on metabolic syndrome risk factors in men. Nutr Metab Cardiovasc Dis. 2015;25(9):832-838. [24] RAM A, MARCOS L, JONES MD, et al. The effect of high-intensity interval training and moderate-intensity continuous training on aerobic fitness and body composition in males with overweight or obesity: a randomized trial. Obes Med. 2020;17:100187. [25] RYAN BJ, SCHLEH MW, Ahn C, et al. Moderate-intensity exercise and high-intensity interval training affect insulin sensitivity similarly in obese adults. J Clin Endocrinol Metab. 2020; 105(8):e2941-e2959. [26] SAWYER BJ, TUCKER WJ, BHAMMAR DM, et al. Effects of high-intensity interval training and moderate-intensity continuous training on endothelial function and cardiometabolic risk markers in obese adults. J Appl Physiol. 2016;121(1):279-288. [27] 李志龙,单示标,解萧,等.高、低运动量HIIT对青年肥胖女性减肥效果的对比研究[J].南京体育学院学报,2023,22(5): 40-46. [28] RELJIC D, FRENK F, HERRMANN HJ, et al. Low-volume high-intensity interval training improves cardiometabolic health, work ability and well-being in severely obese individuals: a randomized-controlled trial sub-study. J Transl Med. 2020;18:1-15. [29] SCHUBERT MM, CLARKE HE, SEAY RF, et al. Impact of 4 weeks of interval training on resting metabolic rate, fitness, and health-related outcomes. Appl Physiol Nutr Metab. 2017;42(10):1073-1081. [30] SMITH-RYAN AE, TREXLER ET, WINGFIELD HL, et al. Effects of high-intensity interval training on cardiometabolic risk factors in overweight/obese women. J Sports Sci. 2016;34(21):2038-2046. [31] RELJIC D, WITTMANN F, FISCHER JE. Effects of low-volume high-intensity interval training in a community setting: a pilot study. Eur J Appl Physiol. 2018;118:1153-1167. [32] EGGER M, SMITH GD, SCHNEIDER M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629-634. [33] FISHMAN B, SHLOMAI G, TWID G, et al. Renal glucosuria is associated with lower body weight and lower rates of elevated systolic blood pressure: results of a nationwide cross-sectional study of 2.5 million adolescents. Cardiovasc Diabetol. 2019;18:1-8. [34] JUNG ME, LOCKE SR, BOURNE JE, et al. Cardiorespiratory fitness and accelerometer-deter mined physical activity following one year of free-living high-intensity interval training and moderate-intensity continuous training: a randomized trial. Int J Behav Nutr Phys Act. 2020;17:1-10. [35] LIU Y, ZHI-JIAN W, BAO-HU L, et al. Relationships between cardiopulmonary function and dangerous cardiovascular factors in Chinese adults: a cross-sectional study. 2024. doi:10.21203/rs.3.rs-3938895/v1. [36] CHEN X, HE H, XIE K, et al. Effects of various exercise types on visceral adipose tissue in individuals with overweight and obesity: a systematic review and network meta‐analysis of 84 randomized controlled trials. Obes Rev. 2024;25(3):e13666. [37] SWIFT DL, JOHANNSEN NM, LAVIE CJ, et al. The role of exercise and physical activity in weight loss and maintenance. Prog Cardiovasc Dis. 2014;56(4):441-447. [38] THOMPSON PD, ARENA R, RIEBE D, et al. ACSM’s new preparticipation health screening recommendations from ACSM’s guidelines for exercise testing and prescription. Curr Sports Med Rep. 2013; 12(4):215-217. [39] 殷明越,陈志力,李汉森,等.碎片化运动:兼具应用可行性与健康促进效果的新策略[J].西安体育学院学报,2023,40(5):615-627. [40] LITTLE JP, LANGLEY J, LEE M, et al. Sprint exercise snacks: a novel approach to increase aerobic fitness. Eur J Appl Physiol. 2019;119:1203-1212. [41] REED JL, TERADA T, COTIE LM, et al. The effects of high-intensity interval training, Nordic walking and moderate-to-vigorous intensity continuous training on functional capacity, depression and quality of life in patients with coronary artery disease enrolled in cardiac rehabilitation: a randomized controlled trial. Prog Cardiovasc Dis. 2022;70:73-83. [42] PETERMAN JE, HARBER MP, IMBODEN MT, et al. Accuracy of exercise-based equations for estimating cardiorespiratory fitness. Med Sci Sports Exerc. 2021;53(1):74. [43] GONCALVES C, RAIMUNDO A, Abreu A, et al. Exercise intensity in patients with cardiovascular diseases: systematic review with meta-analysis. Int J Environ Res Public Health. 2021;18(7):3574. [44] ANDO T, PIAGGI P, BOGARDUS C, et al. VO2max is associated with measures of energy expenditure in sedentary condition but does not predict weight change. Metabolism. 2019; 90:44-51. [45] HARBER MP, MYERS J, BONIKonikowske AR, et al. Assessing cardiorespiratory fitness in clinical and community settings: Lessons and advancements in the 100th year anniversary of VO2max. Prog Cardiovasc Dis. 2024;83:36-42. [46] TJØNNA AE, LEINAN IM, BARTNES AT, et al. Low-and high-volume of intensive endurance training significantly improves maximal oxygen uptake after 10-weeks of training in healthy men. PLoS One. 2013; 8(5):e65382. [47] VOLLAARD NB, METCALFE RS. Research into the health benefits of sprint interval training should focus on protocols with fewer and shorter sprints. Sports Med. 2017;47:2443-2451. [48] DU L, ZHANG X, CHEN K, et al. Effect of high-intensity interval training on physical health in coronary artery disease patients: a meta-analysis of randomized controlled trials. J Cardiovasc Dev Dis. 2021; 8(11):158. [49] YUE T, WANG Y, LIU H, et al. Effects of high-intensity interval vs. moderate-intensity continuous training on cardiac rehabilitation in patients with cardiovascular disease: a systematic review and meta-analysis. Front Cardiovasc Med. 2022;9:845225. [50] RELJIC D, KOLLER A, HERRMANN HJ, et al. Differential effects of very-low-volume exercise modalities on telomere length, inflammation, and cardiometabolic health in obese metabolic syndrome patients: a subanalysis from two randomized controlled trials. Antioxidants.2023;12(10):1847. [51] BIRKETT ST, NICHOLS S, SAWREY R, et al. The effects of low-volume high-intensity interval training and circuit training on maximal oxygen uptake. J Sports Med Phys Fitness. 2019;15:443-451. [52] GHARDASHI-AFOUSI A, HOLISAZ MT, Shirvani H, et al. The effects of low-volume high-intensity interval versus moderate intensity continuous training on heart rate variability, and hemodynamic and echocardiography indices in men after coronary artery bypass grafting: a randomized clinical trial study. ARYA atheroscler. 2018;14(6):260. [53] LYALL DM, CELIS-MORALES C, WARD J, et al. Association of body mass index with cardiometabolic disease in the UK Biobank: a Mendelian randomization study. JAMA Cardiol. 2017;2(8):882-889. [54] FEIGIN VL, STARK BA, JOHNSON CO, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20(10):795-820.
[55] MARCEAU F, REGOLI D. Bradykinin receptor ligands: therapeutic perspectives. Nat Rev Drug Discov. 2004;3(10):845-852. [56] SHARMA JN. Hypertension and the bradykinin system. Curr Hypertens Rep. 2009;11(3):178-181. [57] PAL S, RADAVELLI-BAGATINI S, HO S. Potential benefits of exercise on blood pressure and vascular function. J Am Soc Hypertens. 2013;7(6):494-506. [58] WHELTONS P, CHIN A, XIN X, et al. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136(7):493-503. [59] GRASSI G, MARK A, ESLER M. The sympathetic nervous system alterations in human hypertension. Circ Res. 2015; 116(6):976-990. [60] WAY KL, SABAG A, SULTANA RN, et al. The effect of low-volume high-intensity interval training on cardiovascular health outcomes in type 2 diabetes: a randomised controlled trial. Int J Cardiol. 2020;320:148-154. [61] OLEA MA, MANCILLA R, MARTINEZ S, et al. Effects of high intensity interval training on blood pressure in hypertensive subjects. Rev Med Chil. 2017;145(9):1154-1159. [62] LEE K, SONG YM, SUNG J. Which obesity indicators are better predictors of metabolic risk?: healthy twin study. Obesity. 2008;16(4):834-840. [63] WINDING KM, MUNCH GW, LEPSEN UW, et al. The effect on glycaemic control of low‐volume high‐intensity interval training versus endurance training in individuals with type 2 diabetes. Diabetes Obes Metab. 2018;20(5):1131-1139. [64] SULTANA RN, SABAG A, KEATING SE, et al. The effect of low-volume high-intensity interval training on body composition and cardiorespiratory fitness: a systematic review and meta-analysis. Sports Med. 2019;49:1687-1721. [65] Li F, NIE J, ZHANG H, et al. Effects of matched intermittent and continuous exercise on changes of cardiac biomarkers in endurance runners. Front Physiol. 2020; 11:30. [66] ALVES JW, FARIAS-JUNIOR LF, Alves CPDL, et al. Low-volume high-intensity interval training sessions with different work-recovery durations and muscle damage in trained men. Res Q Exerc Sport. 2023;94(1):73-81. [67] PURDOM T, KRAVITZ L, DOKLADNY K, et al. Understanding the factors that effect maximal fat oxidation. J Int Soc Sports Nutr. 2018;15(1):3. [68] MEDICA EM. Excess post-exercise oxygen consumption and fat oxidation in recreationally trained men following exercise of equal energy expenditure: comparisons of spinning and constant endurance exercise. J Sports Med Phys Fitness. 2017;(12):1781-1789. [69] WANNAMETHEE G, SHAPER AG. The association between heart rate and blood pressure, blood lipids and other cardiovascular risk factors. J Cardiovasc Risk. 1994;1(3):223-230. [70] KARIM MN, AHMED KR, Bukht MS, et al. Pattern and predictors of dyslipidemia in patients with type 2 diabetes mellitus. Diabetes Metab Syndr. 2013;7(2):95-100. [71] TOBERT JA, NEWMAN CB. Management of dyslipidemia for cardiovascular disease risk reduction. Ann Intern Med. 2016; 164(7):509. [72] HEDAYATINA M, ASADI Z, ZARE-FEYZABADI R, et al. Dyslipidemia and cardiovascular disease risk among the MASHAD study population. Lipids Health Dis. 2020;19:1-11. [73] WARNER SO, YAO MV, CASON RL, et al. Exercise-induced improvements to whole body glucose metabolism in type 2 diabetes: the essential role of the liver. Front Endocrinol. 2020;11:557166. [74] TREFTS E, WILLIAMS AS, WASSERMAN DH. Exercise and the regulation of hepatic metabolism. Prog Mol Biol Transl Sci. 2015; 135:203-225. [75] PETERSEN AMW, Pedersen BK. The anti-inflammatory effect of exercise. J Appl Physiol. 2005;98(4):1154-1162. [76] ISLAM H, GIBALA MJ, Little JP. Exercise snacks: a novel strategy to improve cardiometabolic health. Exerc Sport Sci Rev. 2022;50(1):31-37. [77] YIN M, DENG S, CHEN Z, et al. Exercise snacks are a time-efficient alternative to moderate-intensity continuous training for improving cardiorespiratory fitness but not maximal fat oxidation in inactive adults: a randomized controlled trial. Appl Physiol Nutr Metab. 2024. doi: 10.1139/apnm-2023-0593. [78] NIESTE I, FRANSSEN WM, SPAAS J, et al. Lifestyle interventions to reduce sedentary behaviour in clinical populations: a systematic review and meta-analysis of different strategies and effects on cardiometabolic health. Prev Med. 2021; 148:106593. [79] GARDNER B, SMITH L, LORENCATTO F, et al. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychol Rev. 2016;10(1):89-112. |
| [1] | Chen Jiayong, Tang Meiling, Lu Jianqi, Pang Yan, Yang Shangbing, Mao Meiling, Luo Wenkuan, Lu Wei, Zhou Jiatan. Based on Mendelian randomization, the causal relationship between 1400 metabolites and sarcopenia and the correlation analysis of cardiovascular disease were investigated [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-11. |
| [2] | Sun Yundi, Cheng Lulu, Wan Haili, Chang Ying, Xiong Wenjuan, Xia Yuan. Effect of neuromuscular exercise for knee osteoarthritis pain and function: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1945-1952. |
| [3] | Wang Yida, Liu Jun, Wang Xiaoling, Wang Liyan, Yang Chengru, Zhang Xuexiao. Effects of wearable electronic device-based interventions on physical activity and sedentary behavior in healthy adolescents: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1693-1704. |
| [4] | Zhang Zixian, Xu Youliang, Wu Shaokui, Wang Xiangying. Effects of blood flow restriction training combined with resistance training on muscle indicators in college athletes: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1705-1713. |
| [5] | Wang Juan, Wang Guanglan, Zuo Huiwu. Efficacy of exercise therapy in the treatment of anterior cruciate ligament reconstruction patients: #br# a network meta-analysis #br# [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1714-1726. |
| [6] | Zheng Huakun, Yin Mingyue, Liu Qian. Effects of interval and continuous training on the quality of life in physically inactive adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1727-1740. |
| [7] | Wang Feng, Cao Chunfeng, He Chao, Zhang Tao, Zhou Zixian, Zhu Fengchen. All-inside versus traditional techniques of anterior cruciate ligament reconstruction: meta-analysis of therapeutic efficacy and radiological outcomes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7629-7638. |
| [8] | Liu Chenchen, Liu Ruize, Bao Mengmeng, Fang Li, Cao Liquan, Wu Jiangbo. Blood flow restriction training intervention in the elderly with sarcopenic obesity [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6963-6970. |
| [9] | Liu Liguo, Qiu Mingwang, Huang Yanling, Fan Zhiyong, Wu Shan, Guo Rusong. Reporting quality of randomized controlled trials on acupuncture and manipulation for greater occipital neuralgia evaluated using the CONSORT statement and STRICTA checklist [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6566-6573. |
| [10] | Liu Haowei, Tian Haodong, Huang Li, Yu Hanglin, Peng Li. Acute effects of blood flow restriction resistance exercise on serum metabolites in obese young men [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6249-6259. |
| [11] | Yu Bingbing, Wang Tingting, Fang Junlin, Guo Yun, Huang Yingru. Acupuncture for treatment of postmenopausal osteoporosis: meta-analysis, systematic evaluation and trial sequential analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6305-6316. |
| [12] | Chen Jinjie, Li Geng, Jiang Yefan. Role of Siblings protein family in cardiovascular diseases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5171-5178. |
| [13] | Deng Yiran, Wang Xianliang, Li Dandan. Meta-analysis of exercise intervention on cardiopulmonary function in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5203-5211. |
| [14] | Hu Tong, Li Xuan, Yuan Jing, Wang Wei. Different electromagnetic stimulation programs improve post-stroke dysphagia: a network Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5224-5236. |
| [15] |
Yang Fengying, Zhao Yuqing, You Huijuan, Zhang Pengyi, Chen Yan, Wang Qinglu, Liu Yingying .
Macrophage efferocytosis: a new target for the treatment of obesity-related metabolic diseases #br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(2): 430-440.
|
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||