Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (32): 5203-5209.doi: 10.12307/2024.509
Previous Articles Next Articles
Sleep characteristics and risk of osteoarthritis: a two-sample and multivariate Mendelian randomization study
Chen Jixin1, 2, Yu Weijie1, 2, Guo Tianci1, 2, Zhou Qinxin3, Niu Puyu1, 2, Ye Yuntian1, 2, Liu Aifeng1, 2
- 1Department of Traumatology and Orthopedics, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin 300381, China; 2National Clinical Research Center for Chinese Medicine Acupuncture and Moxibustion, Tianjin 300381, China; 3Department of Traumatology and Orthopedics, Shaoxing Traditional Chinese Medicine Hospital, Shaoxing 312000, Zhejiang Province, China
-
Received:2023-09-18Accepted:2023-10-20Online:2024-11-18Published:2023-12-29 -
Contact:Liu Aifeng, Chief physician, Doctoral supervisor, Department of Traumatology and Orthopedics, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin 300381, China; National Clinical Research Center for Chinese Medicine Acupuncture and Moxibustion, Tianjin 300381, China; National Clinical Research Center for Chinese Medicine Acupuncture and Moxibustion, Tianjin 300381, China -
About author:Chen Jixin, MD candidate, Department of Traumatology and Orthopedics, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin 300381, China; National Clinical Research Center for Chinese Medicine Acupuncture and Moxibustion, Tianjin 300381, China -
Supported by:National Natural Science Foundation of China, No. 81873316 (to LAF); Cross-research Project of Bone Disease Prevention and Treatment, Chinese Association of Chinese Medicine, No. 2023-GBJC-04 (to LAF); Jinmen Medical Talent Project of Tianjin Health Commission, No. TJSJMYXYC-D2-028 (to LAF)
CLC Number:
Cite this article
Chen Jixin, Yu Weijie, Guo Tianci, Zhou Qinxin, Niu Puyu, Ye Yuntian, Liu Aifeng. Sleep characteristics and risk of osteoarthritis: a two-sample and multivariate Mendelian randomization study[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(32): 5203-5209.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
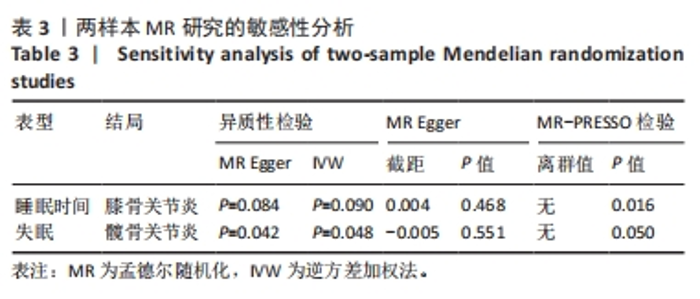
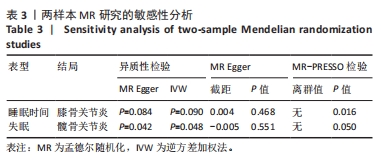
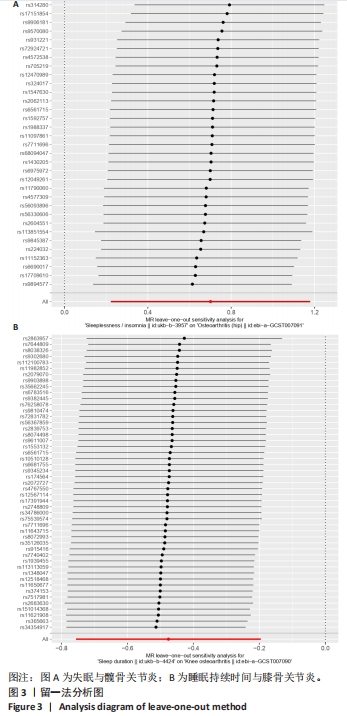
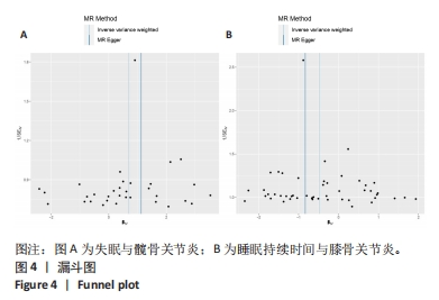
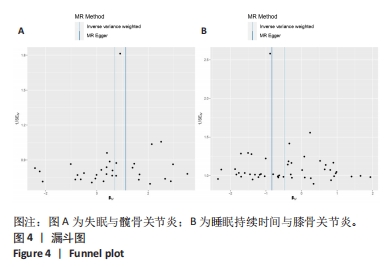
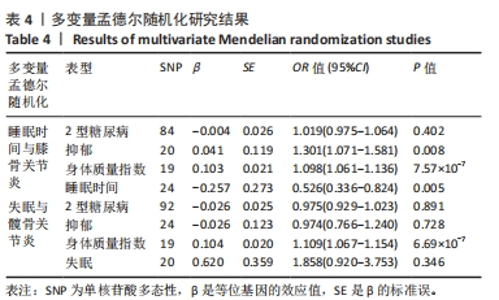
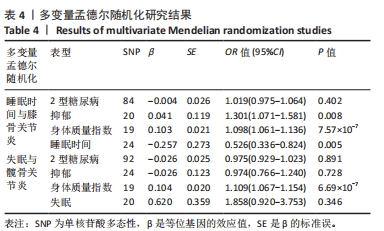
2.1 工具变量的选取 根据筛选标准,7个睡眠表型的工具变量被纳入研究。在该研究中,每个工具变量的 F 统计量均> 10,表明研究中存在弱工具变量偏倚的证据较低。 2.2 两样本MR研究 使用Cochran’s Q 检验检测工具变量的异质性,P > 0.05,可认为工具变量间不存在异质性,主要使用固定效应模型的 IVW 进行因果关系的探讨;反之,使用随机效应模型。根据表2所示的IVW结果,睡眠时间与膝骨关节炎发病存在负相关的因果关联,失眠与膝骨关节炎、髋骨关节炎发病存在正相关的因果关联,但失眠与膝骨关节炎的结果中,MR Egger和IVW总效应值的方向相反,故排除。其余睡眠表型未见因果关联。"
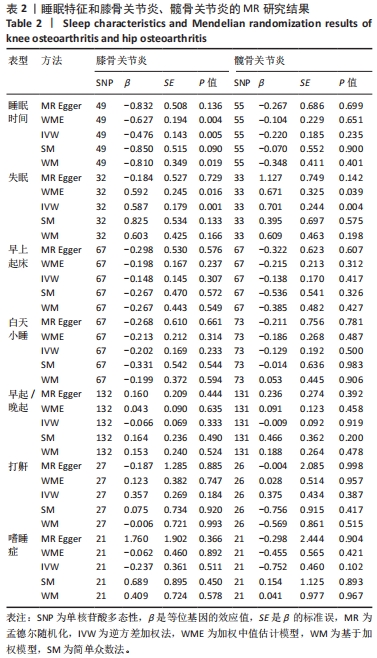

在失眠与髋骨关节炎的关联研究中,首先从失眠GWAS中提取42个显著相关水平(P < 5×10-8)和连锁不平衡(r2 < 0.001,10 000 kb)的SNP,与提取的髋骨关节炎数据集合并,并删除回文SNP共3个(rs2644128, rs2803296, rs8180817),检索PhenoScanner数据库,删除与身体质量指数相关6个SNP(rs10838708,rs11635495,rs2014830,rs2297787,rs4886860,rs56365214),MR-PRESSO 分析无离群值,SNP的F统计量为29.85-199.34。最终纳入33个SNP进行失眠与髋骨关节炎的MR分析,统计效能为1。5种统计方法结果相似,总效应值的方向一致,呈正相关,其中IVW和WME的统计学结果显著。MR Egger、WME、IVW、SM、WM的结果分别为(OR=3.086,95%CI:0.712-13.382,P=0.136)、(OR=1.957, 95%CI:1.034-3.702,P=0.004)、(OR=2.016,95%CI:1.249-3.254,P=0.005)、(OR=1.485,95%CI:0.378-5.825,P=0.090)、(OR=1.838,95%CI:0.742-4.556,P=0.019),结果表明失眠可能是髋骨关节炎发病的风险因素。随着失眠的次数增多,髋骨关节炎的发病风险随之增加,见图2A。 在睡眠时间与膝骨关节炎的关联研究中,首先从睡眠时间GWAS中提取71个显著相关水平(P < 5×10-8)和连锁不平衡(r2 < 0.001,10 000 kb)的SNP,与提取的膝骨关节炎数据集合并,并删除6个回文SNP(rs1972712,rs1611719,rs1517572,rs2236295,rs55658675,rs6889592),检索PhenoScanner数据库,删除与身体质量指数相关16个SNP(rs11039216,rs113021516,rs13107325,rs1463053,rs17732997,rs2186122,rs2192528,rs2279681,rs2279681,rs34556183,rs62444917,rs7016314,rs7115856,rs72771082,rs7831557,rs8047587),MR-PRESSO分析无离群值,SNP的F统计量为30.05-224.46。最终纳入49个SNP进行睡眠时间与膝骨关节炎的MR分析,统计效能为0.98。5种统计方法结果相似,总效应值的方向一致,呈正相关,其中IVW、WM和WME的统计学结果显著。MR Egger、WME、IVW、SM、WM的结果分别为(OR=0.435,95%CI:0.161-1.178, P=0.108)、(OR=0.534,95%CI:0.365-0.782,P=0.001)、(OR=0.621,95%CI:0.470-0.822,P=0.001)、(OR=0.427,95%CI:0.156-1.171,P=0.105)、(OR=0.445,95%CI:0.225-0.881,P=0.024),结果表明,睡眠持续时间可能是膝骨关节炎发病的保护因素。随着睡觉持续时间的减少,膝骨关节炎的发病风险随之增加,见图2B。"

| [1] KOLASINSKI SL, NEOGI T, HOCHBERG MC, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020;72(2):220-233. [2] SHARMA L. Osteoarthritis of the Knee. N Engl J Med. 2021;384(1):51-59. [3] SCHÄFER N, GRÄSSEL S. Targeted therapy for osteoarthritis: progress and pitfalls. Nat Med. 2022;28(12):2473-2475. [4] TONG L, YU H, HUANG X, et al. Current understanding of osteoarthritis pathogenesis and relevant new approaches. Bone Res. 2022;10(1):60. [5] XIE J, WANG Y, LU L, et al. Cellular senescence in knee osteoarthritis: molecular mechanisms and therapeutic implications. Ageing Res Rev. 2021;70:101413. [6] YAO Q, WU X, TAO C, et al. Osteoarthritis: pathogenic signaling pathways and therapeutic targets. Signal Transduct Target Ther. 2023;8(1):56. [7] MCKENNA S, LARKIN L, DONNELLY A, et al. OP0267-HPR “I NEVER THOUGHT EXERCISE COULD HELP IMPROVE MY SLEEP”: Experiences of people with rheumatoid arthritis on the impact of exercise on sleep. Ann Rheum Dis. 2020; 79(Suppl 1): 161-167. [8] JACOB L, SMITH L, KONRAD M, et al. Association between sleep disorders and osteoarthritis: A case-control study of 351,932 adults in the UK. J Sleep Res. 2021;30(6):e13367. [9] JUNG JH, SEOK H, CHOI SJ, et al. The association between osteoarthritis and sleep duration in Koreans: a nationwide cross-sectional observational study. Clin Rheumatol. 2018;37(6):1653-1659. [10] PARK HM, KWON YJ, KIM HS, et al. Relationship between Sleep Duration and Osteoarthritis in Middle-Aged and Older Women: A Nationwide Population-Based Study. J Clin Med. 2019;8(3):356. [11] LATORRE D, SALLUSTO F, BASSETTI CLA, et al. Narcolepsy: a model interaction between immune system, nervous system, and sleep-wake regulation. Semin Immunopathol. 2022;44(5):611-623. [12] IRWIN MR, STRAUB RH, SMITH MT. Heat of the night: sleep disturbance activates inflammatory mechanisms and induces pain in rheumatoid arthritis. Nat Rev Rheumatol. 2023;19(9):545-559. [13] XING X, WANG Y, PAN F, et al. Osteoarthritis and risk of type 2 diabetes: A two-sample Mendelian randomization analysis. J Diabetes. 2023 Jul 31. doi: 10.1111/1753-0407.13451. [14] ZHANG L, ZHANG W, WU X, et al. A sex- and site-specific relationship between body mass index and osteoarthritis: evidence from observational and genetic analyses. Osteoarthritis Cartilage. 2023;31(6):819-828. [15] BAROWSKY S, JUNG JY, NESBIT N, et al. Cross-Disorder Genomics Data Analysis Elucidates a Shared Genetic Basis Between Major Depression and Osteoarthritis Pain. Front Genet. 2021;12:687687. [16] NAZARZADEH M, PINHO-GOMES AC, BIDEL Z, et al. Plasma lipids and risk of aortic valve stenosis: a Mendelian randomization study. Eur Heart J. 2020;41(40):3913-3920. [17] LAWLOR DA, HARBORD RM, STERNE JA, et al. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med. 2008;27(8):1133-1163. [18] CLAYTON GL, SOARES AG, GOULDING N, et al. A framework for assessing selection and misclassification bias in mendelian randomisation studies: an illustrative example between body mass index and covid-19. BMJ. 2023;381:e072148. [19] SKRIVANKOVA VW, RICHMOND RC, WOOLF BAR, et al. Strengthening the reporting of observational studies in epidemiology using mendelian randomisation (STROBE-MR): explanation and elaboration. BMJ. 2021;375:n2233. [20] FABER BG, FRYSZ M, BOER CG, et al. The identification of distinct protective and susceptibility mechanisms for hip osteoarthritis: findings from a genome-wide association study meta-analysis of minimum joint space width and Mendelian randomisation cluster analyses. EBioMedicine. 2023;95:104759. [21] YANG J, LIU P, WANG S, et al. Causal relationship between sarcopenia and osteoarthritis: a bi-directional two-sample mendelian randomized study. Eur J Med Res. 2023;28(1):327. [22] SU D, AI Y, ZHU G, et al. Genetically predicted circulating levels of cytokines and the risk of osteoarthritis: A mendelian randomization study. Front Genet. 2023;14:1131198. [23] ZHANG Y, XIE J, WEN S, et al. Evaluating the causal effect of circulating proteome on the risk of osteoarthritis-related traits. Ann Rheum Dis. 2023 Aug 18. doi: 10.1136/ard-2023-224459. [24] TACHMAZIDOU I, HATZIKOTOULAS K, SOUTHAM L, et al. Identification of new therapeutic targets for osteoarthritis through genome-wide analyses of UK Biobank data. Nat Genet. 2019;51(2):230-236. [25] HOWARD DM, ADAMS MJ, CLARKE TK, et al. Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. Nat Neurosci. 2019;22(3):343-352. [26] XUE A, WU Y, ZHU Z, et al. Genome-wide association analyses identify 143 risk variants and putative regulatory mechanisms for type 2 diabetes. Nat Commun. 2018;9(1):2941. [27] BURGESS S, DAVEY SMITH G, DAVIES NM, et al. Guidelines for performing Mendelian randomization investigations: update for summer 2023. Wellcome Open Res. 2023;4:186. [28] SKRIVANKOVA VW, RICHMOND RC, WOOLF BAR, et al. Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization: The STROBE-MR Statement. JAMA. 2021;326(16):1614-1621. [29] QIU S, ZHENG K, HU Y, et al. Genetic correlation, causal relationship, and shared loci between vitamin D and COVID-19: A genome-wide cross-trait analysis. J Med Virol. 2023;95(5):e28780. [30] LEVIN MG, JUDY R, GILL D, et al. Genetics of height and risk of atrial fibrillation: A Mendelian randomization study. PLoS Med. 2020;17(10):e1003288. [31] CODD V, NELSON CP, ALBRECHT E, et al. Identification of seven loci affecting mean telomere length and their association with disease. Nat Genet. 2013;45(4):422-427. [32] LI W, LU Q, QIAN J, et al. Assessing the causal relationship between genetically determined inflammatory biomarkers and low back pain risk: a bidirectional two-sample Mendelian randomization study. Front Immunol. 2023;14:1174656. [33] YUAN S, MIAO Y, RUAN X, et al. Therapeutic role of interleukin-1 receptor antagonist in pancreatic diseases: mendelian randomization study. Front Immunol. 2023;14:1240754. [34] HAN Y, ZHANG Y, ZENG X. Assessment of causal associations between uric acid and 25-hydroxyvitamin D levels. Front Endocrinol (Lausanne). 2022;13:1024675. [35] DOBRIJEVIC E, VAN ZWIETEN A, KIRYLUK K, et al. Mendelian randomization for nephrologists. Kidney Int. 2023 Sep 30. doi: 10.1016/j.kint.2023.09.016. [36] LI J, BAI H, QIAO H, et al. Causal effects of COVID-19 on cancer risk: A Mendelian randomization study. J Med Virol. 2023;95(4):e28722. [37] YAO S, ZHANG M, DONG SS, et al. Bidirectional two-sample Mendelian randomization analysis identifies causal associations between relative carbohydrate intake and depression. Nat Hum Behav. 2022;6(11):1569-1576. [38] SHANG W, ZHANG S, QIAN H, et al. Association of gut microbiota with COVID-19 susceptibility and severity: A two-sample Mendelian randomization study. J Med Virol. 2023;95(4):e28734. [39] MAZIDI M, SHEKOOHI N, KATSIKI N, et al. Impact of lifetime concentration of mannose on renal function: insights from Mendelian randomization. Eur Heart J. 2022;43(S2):ehac544.2612. [40] ZHOU F, LI S, XU H. Insomnia, sleep duration, and risk of anxiety: A two-sample Mendelian randomization study. J Psychiatr Res. 2022;155:219-225. [41] LEE MS, SHIN JS, LEE J, et al. The association between mental health, chronic disease and sleep duration in Koreans: a cross-sectional study. BMC Public Health. 2015;15:1200. [42] GONZALEZ C, KUSKO D, SIBILLE K, et al. Clinical pain, pain catastrophizing, and sleep quality in Ethnic/Race Groups with or at risk for Knee Osteoarthritis: A moderated mediation model. J Pain. 2021;22(5):598. [43] WANG Y, LI X, ZHANG Y, et al. Association of Sleep Disturbance With Catastrophizing and Knee Pain: Data From the Osteoarthritis Initiative. Arthritis Care Res (Hoboken). 2023;75(10):2134-2141. [44] VITIELLO MV, ZHU W, VON KORFF M, et al. Long-term improvements in sleep, pain, depression, and fatigue in older adults with comorbid osteoarthritis pain and insomnia. Sleep. 2022;45(2):zsab231. [45] IRWIN MR, OPP MR. Sleep Health: Reciprocal Regulation of Sleep and Innate Immunity. Neuropsychopharmacology. 2017;42(1):129-155. [46] WOODELL-MAY JE, SOMMERFELD SD. Role of Inflammation and the Immune System in the Progression of Osteoarthritis. J Orthop Res. 2020;38(2):253-257. [47] NA HS, PARK JS, CHO KH, et al. Interleukin-1-Interleukin-17 Signaling Axis Induces Cartilage Destruction and Promotes Experimental Osteoarthritis. Front Immunol. 2020;11:730. [48] ROHLEDER N, ARINGER M, BOENTERT M. Role of interleukin-6 in stress, sleep, and fatigue. Ann N Y Acad Sci. 2012;1261:88-96. [49] WU J, LI Q, DENG J, et al. Association between IL-33 and other inflammatory factors in patients with rheumatoid arthritis and in fibroblast-like synoviocytes in vitro. Exp Ther Med. 2021;21(2):161. [50] HOSSAIN FM, HONG Y, JIN Y, et al. Physiological and Pathological Role of Circadian Hormones in Osteoarthritis: Dose-Dependent or Time-Dependent? J Clin Med. 2019;8(9):1415. [51] CHAPUT JP, MCHILL AW, COX RC, et al. The role of insufficient sleep and circadian misalignment in obesity. Nat Rev Endocrinol. 2023;19(2):82-97. [52] MULUGETA A, ESHETIE TC, KASSIE GM, et al. Association Between Metabolically Different Adiposity Subtypes and Osteoarthritis: A Mendelian Randomization Study. Arthritis Care Res (Hoboken). 2023;75(4):885-892. [53] LI W, WANG Z, CAO J, et al. Melatonin improves the homeostasis of mice gut microbiota rhythm caused by sleep restriction. Microbes Infect. 2023;25(6): 105121. [54] ZHANG M, ZHANG M, KOU G, et al. The relationship between gut microbiota and inflammatory response, learning and memory in mice by sleep deprivation. Front Cell Infect Microbiol. 2023;13:1159771. [55] LIU L, TIAN F, LI GY, et al. The effects and significance of gut microbiota and its metabolites on the regulation of osteoarthritis: Close coordination of gut-bone axis. Front Nutr. 2022;9:1012087. [56] GUAN Z, JIN X, GUAN Z, et al. The gut microbiota metabolite capsiate regulate SLC2A1 expression by targeting HIF-1α to inhibit knee osteoarthritis-induced ferroptosis. Aging Cell. 2023;22(6):e13807. [57] BIRNEY E. Mendelian Randomization. Cold Spring Harb Perspect Med. 2022;12(4): a041302. [58] WEITH M, BEYER A. The next step in Mendelian randomization. Elife. 2023;12: e86416. |
| [1] | Li Yongjie, Fu Shenyu, Xia Yuan, Zhang Dakuan, Liu Hongju. Correlation of knee extensor muscle strength and spatiotemporal gait parameters with peak knee flexion/adduction moment in female patients with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1354-1358. |
| [2] | Du Changling, Shi Hui, Zhang Shoutao, Meng Tao, Liu Dong, Li Jian, Cao Heng, Xu Chuang. Efficacy and safety of different applications of tranexamic acid in high tibial osteotomy [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1409-1413. |
| [3] | Huang Xiarong, Hu Lizhi, Sun Guanghua, Peng Xinke, Liao Ying, Liao Yuan, Liu Jing, Yin Linwei, Zhong Peirui, Peng Ting, Zhou Jun, Qu Mengjian. Effect of electroacupuncture on the expression of P53 and P21 in articular cartilage and subchondral bone of aged rats with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1174-1179. |
| [4] | Zhang Zeyi, Yang Yimin, Li Wenyan, Zhang Meizhen. Effect of foot progression angle on lower extremity kinetics of knee osteoarthritis patients of different ages: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 968-975. |
| [5] | Shen Feiyan, Yao Jixiang, Su Shanshan, Zhao Zhongmin, Tang Weidong. Knockdown of circRNA WD repeat containing protein 1 inhibits proliferation and induces apoptosis of chondrocytes in knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 499-504. |
| [6] | Lu Mengya, Wu Xian, She Zeyu, Xia Shuai, Lu Man, Yang Yonghui. Acupotomy prevents knee osteoarthritis in rats by modulating chondrocyte apoptosis in the mitochondrial pathway [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(32): 5190-5195. |
| [7] | Fu Qiangchang, Zheng Liming, Jiang Lifeng. High tibial osteotomy promotes cartilage regeneration in the treatment of knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(32): 5243-5248. |
| [8] | Ren Weiliang, Jiao Yongwei, Zhang Jian, Yang Liying, Yang Qi. Modulatory effect of resveratrol on oxidative stress and inflammatory factors in the joint fluid of rats with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(32): 5154-5158. |
| [9] | Hou Zengtao, Dong Zhiwei, Zhang Jinfeng, Yang Xiaohui, Fan Xiao. Platelet-rich fibrin regulates apoptosis to promote cartilage repair in rats with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(32): 5167-5171. |
| [10] | Yin Linwei, Huang Xiarong, Sun Guanghua, Liu Jing, Zhong Peirui, Wang Jinling, Chen Jiaqian, Wen Xing, Gan Shaoting, Hu Wentao, Li Mengmeng, Zhou Jun. Pulsed electromagnetic fields inhibit knee cartilage degeneration in aged rats [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(28): 4522-4527. |
| [11] | Liu Mengfei, Ma Pengcheng, Yin Can, Jiang Kan, Ju Xiaochen. Three-dimensional finite element analysis of effects of different bone densities on various intraarticular structures after unicompartmental knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(24): 3801-3806. |
| [12] | Wang Hu, Feng Shuo, Zhang Qiang, Chen Jiahao, Chen Xiangyang. Effect of varus and valgus angles of tibial prosthesis on short-term outcome of fixed bearing unicompartmental knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(24): 3827-3832. |
| [13] | Li Chun, Zhang Yanlin, Liu Di, Wang Minglei, Wang Duo, Liu Junwei, Wu Yongli. Effect of warm-needling moxibustion on anterior cruciate ligament injury repair and related growth factors in rabbits with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3621-3626. |
| [14] | Wu Ruiqi, Zhou Yi, Xia Tian, Zhang Chi, Yang Qipei, Zhang Xuan, Zhang Yazhong, Cui Wei. Mendelian randomization study on the association between rheumatoid arthritis and osteoporosis and bone mineral density [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3715-3721. |
| [15] | Yang Yongze, Cheng Qinghao, Zhang Anren, Yang Xin, Zhang Zhuangzhuang, Fan Hua, Zhang Fukang, Guo Hongzhang. Advantages and disadvantages of trauma effects during robot-assisted total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(21): 3413-3417. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||