Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (21): 3413-3417.doi: 10.12307/2024.079
Previous Articles Next Articles
Advantages and disadvantages of trauma effects during robot-assisted total knee arthroplasty
Yang Yongze1, Cheng Qinghao2, Zhang Anren1, Yang Xin1, Zhang Zhuangzhuang1, Fan Hua1, Zhang Fukang1, Guo Hongzhang2
- 1First Clinical Medical College of Gansu University of Chinese Medicine, Lanzhou 780000, Gansu Province, China; 2Fourth Ward of Department of Orthopedics, Gansu Provincial Hospital, Lanzhou 780000, Gansu Province, China
-
Received:2023-04-24Accepted:2023-05-15Online:2024-07-28Published:2023-09-28 -
Contact:Guo Hongzhang, MD, Chief physician, Fourth Ward of Department of Orthopedics, Gansu Provincial Hospital, Lanzhou 780000, Gansu Province, China -
About author:Yang Yongze, Master candidate, First Clinical Medical College of Gansu University of Chinese Medicine, Lanzhou 780000, Gansu Province, China -
Supported by:Gansu Provincial Natural Science Foundation, No. 20JR10RA358 (to GHZ)
CLC Number:
Cite this article
Yang Yongze, Cheng Qinghao, Zhang Anren, Yang Xin, Zhang Zhuangzhuang, Fan Hua, Zhang Fukang, Guo Hongzhang. Advantages and disadvantages of trauma effects during robot-assisted total knee arthroplasty[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(21): 3413-3417.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
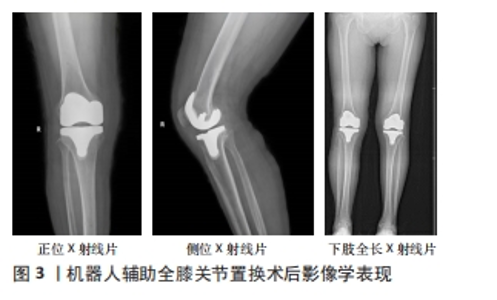
2.1 减轻周围软组织损伤 TKA是一种治疗晚期膝骨关节炎的有效方法,手术目标是用人工植入物代替病变的骨头,恢复下肢力线对齐,保持关节线,平衡屈曲伸展间隙。为了实现这些目标,TKA过程中对周围软组织包膜的保护至关重要[6-8]。 关节周围软组织结构的意外损伤,如副韧带、后交叉韧带或伸肌机制,可能损害术后临床和功能恢复,降低稳定性及植入物存活率[9-11]。KHLOPAS等[12]开展了一项尸体标本研究,比较RATKA和传统TKA在术中保护软组织方面的差异,结果显示 RATKA可以更好地保护内、外侧副韧带,完整保留后交叉韧带胫骨侧止点,而传统手术的6具标本中有2具后交叉韧带胫骨侧止点被手术器械损伤,甚至离断。在另一项尸体研究中HAMPP等[13]发现与传统TKA标本相比,RATKA中后交叉韧带的损伤明显较小(P < 0.001),RATKA标本内侧副韧带、髂胫束、腘窝和髌韧带的损伤无显著变化,结果表明,与传统TKA相比,使用RATKA时可能发生的软组织损伤更少,这是由于机器人辅助技术增强了术前计划、术中实时反馈和触觉束缚锯片的作用。此外,也可能与RATKA锯片振荡的有效宽度(或总切削尖端偏移)较小有关[14],同时也可能是在传统TKA手术中倾向于产生完全横贯的胫骨切除术,而RATKA手术旨在保护后交叉韧带,而后交叉韧带是胫骨后移的主要制约因素,在关节屈伸中起重要作用。但这些结论是基于尸体标本研究,具有一定局限性。 最近一项临床前瞻性队列研究报道,与传统TKA相比RATKA可减少医源性软组织包膜损伤,如韧带损伤;与传统TKA相比,RATKA患者的宏观软组织损伤评分提高了58分(P < 0.05),宏观软组织损伤评分用于评估关节周围软组织的不同区域损伤程度,这说明RATKA可减少骨和软组织损伤[15]。SIEBERT等[16]回顾性分析了120例患者,其中70例接受了RATKA,50例接受了传统TKA,并报告前者的软组织肿胀要小得多。这可能归因于在机器人辅助下,限定于立体定向窗口边界的锯片动作可能有助于更好地控制骨切除的准确性并限制对关节周围软组织包膜的损伤。此外,RATKA 无需行胫骨前脱位和向外侧翻转髌骨的处理,降低了髌腱、股四头肌腱和腘窝周围软组织的损伤风险,这也是RATKA术后患者软组织肿胀较轻的原因之一[15]。见图3。"
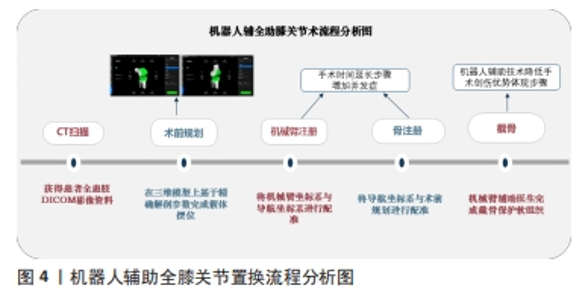
2.2 精确截骨 RATKA作为一种提高截骨准确性的技术,可有效减少肢体对齐异常值[17-19]。在这些系统中,RATKA 术中截骨量和截骨角度已根据术前规划在系统中预先设定,相当于给“有创操作”限定了区域,机械手臂末端的磨钻涉及到的所有操作均在红外摄像头实时监视下完成,若磨钻活动范围超出预先设定区域,“自动操作”就会立即停止。BATHIS等[20]通过分析50例骨切除术患者证实了RATKA的准确性,其股骨远端和胫骨切除术的偏差分别为0.6 mm(SD=0.4)和0.7 mm(SD=0.5)。此外,MASON等[21]报道,91%的患者髋膝踝角为(180±3)°,实现了机械对准理想偏差。总体而言,机器人手臂辅助技术可以准确执行术前骨切除计划并实现理想的屈伸间隙平衡[22],这对于机械对齐和韧带张力非常重要。 XU等[5]通过量化RATKA手术各个具体操作步骤的具体时间,结果发现RATKA有利于在手术时间水平上控制创伤反应。最主要是RATKA显著缩短了骨切割和间隙平衡所需的时间:RATKA的持续时间分别比传统TKA短5.3 min(P=0.010)和2.2 min(P=0.021)。这一发现在已往研究表明,TKA期间的截骨错误和重复截骨可导致股骨干骺端窦腔过度开放、凝血因子耗尽和进行性炎症级联反应[23-24]。其次,之所以RATKA的手术时间明显长于传统TKA,在于RATKA的手术时间增加主要集中在术前计划和术中登记阶段,也就是说,这两阶段的时间增加不会影响与关节腔打开相关的时间,或干扰髓腔,从而引发创伤和炎症。 2.3 术后疼痛 对TKA的需求逐年增加,人们担心满足它所需的可用医疗资源。为了降低医疗资源的消耗,临床采取通过围术期患者优化、多模式镇痛推动了患者术后功能恢复。患者的术后疼痛是术后住院时间延长、镇痛需求、并发症和患者不满意度增加的主要原因[25]。值得注意的是,由于退行性膝关节炎主要好发于老年群体,在受到手术的创伤打击或TKA前疼痛“灾难化”(过分强调消极方面或经历的后果)时,往往表现出焦虑或不安[26-27],这一部分群体中有相当数量患者长期处于独居状态下并且长期受到行动不便和疼痛的困扰,如果术后无法尽早恢复功能或是术后疼痛时,患者会表现出高度焦虑、抑郁,进而影响预后,导致恶性循环的后果[28-30]。因此,TKA除了恢复患者身体健康外,也要注意对其心理健康影响,但很少有干预措施针对这些因素进行干预,部分研究表明减轻患者的术后疼痛和快速康复是一个不错的干预措施,而机器人辅助可能是实现这一措施的有效媒介之一[31-33]。 另外,RATKA可以提供准确的骨切割,降低截骨失败率,减少软组织不必要的释放,该技术理论上可以最大限度地减少了两者的损伤程度,并且两者也都被认为是重要的疼痛发生器[34-35]。根据现有的研究报道,行RATKA的患者阿片类药物消耗量的减少与骨创伤较少有关,也可能是由于在RATKA恢复下肢力线时股骨远端不需要髓内导引板或钻孔,并且软组织释放小创伤较少等,相应的减少阿片类药物的摄入可能有助于降低阿片类药物依赖的风险[36-38]。 RICE等[39]研究发现传统TKA术后6,12个月中重度疼痛的发生率分别为21%和16%。BHIMANI等[34]研究发现,与传统TKA患者相比,接受RATKA的患者在静息和活动时的疼痛程度更低(P <?0.05),每天需要的吗啡当量更少。此外,KAYANI等[40]进行的前瞻性队列研究中,40例患者接受了传统TKA治疗,另有40 例患者接受了RATKA治疗,接受机器人治疗组的患者术后疼痛水平、镇痛需求、物理治疗次数均较传统组减少;并且与接受传统TKA的患者相比,研究结果还表明,RATKA可显著减轻术后疼痛(P < 0.001),这与先前发表的研究相似[34]。这可能也与RATKA减少了手术过程中对胫骨半脱位的需求有关,它仅在组件置入期间需要胫骨半脱位,从而减少软组织损伤。见图4。"
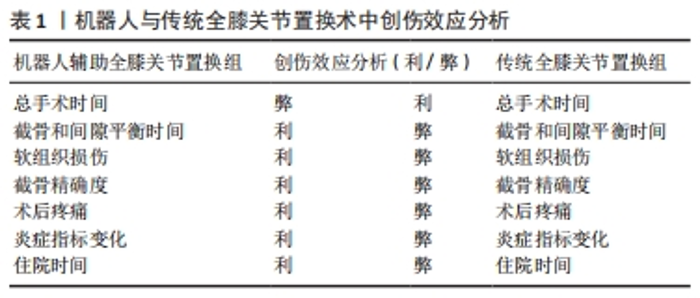
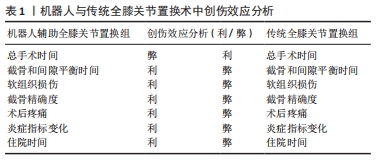
2.4 术后炎症指标变化 血液生化标志物的动态变化被认为是反映TKA创伤严重程度的一个重要参考因素。OELSNER等[41]指出术后C-反应蛋白在住院期间达到峰值,并在2周时恢复到基线水平;纤维蛋白原在C-反应蛋白后达到峰值,并在6周后恢复到基线水平。TKA术前C-反应蛋白升高与术后急性期反应更强烈相关[41-42]。 在一项对中国患者的回顾性研究中,结果显示RATKA组患者术后第1天的白细胞介素6水平显著降低,并且炎症反应的差异在术后第3天变得更加明显,并且RATKA组患者的C-反应蛋白、血沉和白细胞介素6水平显著低于传统TKA组(P < 0.05)[43]。这项研究首次通过血液标志物的比较展示了RATKA在术后恢复中的优势,虽然血清炎症标志物是手术结局的间接代表,但它们是非常客观的,这些差异可能反映在切口愈合、下肢血栓和手术部位疼痛上。RATKA的优势也表现在术后患者血浆D-二聚体水平升高程度上,有研究报道D-二聚体的血浆浓度反映了凝血和纤维蛋白溶解的整体激活[44-46],同时血浆D-二聚体水平升高相关的因素包括创伤、凝血功能障碍等 [45,47]。血浆D-二聚体水平是TKA后静脉血栓栓塞症诊断最有用的实验室检查之一,血浆D-二聚体正常可安全排除静脉血栓栓塞症[48]。在SIU 等[49]的一项前瞻性研究中,结果显示与进行传统TKA的患者相比,术后24 h RATKA组患者中观察到血浆D-二聚体水平降低。这表明RATKA可以减轻手术创伤程度,并且相对于传统TKA而言术后下肢深静脉血栓栓塞的可能性更小,但这一可能性结果需要高质量的循证医学证据加以验证。 此外,XU等[5]发现与传统TKA相比,RATKA可以进一步降低急性期炎症反应中经典生化标志物的含量(P <?0.05),如C-反应蛋白、血沉和D-二聚体等。KAYANI等[40]也进行了类似的观察,术后第7天白细胞介素6、肿瘤坏死因子α、血沉、C-反应蛋白、乳酸脱氢酶和肌酸激酶水平分别比传统TKA ( all P?<?0.05)术后低70.9%,42.4%,38.1%,61.4%,16.3%和47.5%。两组炎症指标的差异,可能与上文提到的RATKA组在股骨截骨术中未使用髓内定位以及使用机械臂截骨术可防止软组织损伤并减少韧带释放有关。 2.5 缩短住院时间 在过去十几年中实施机器人辅助技术在初次TKA后的住院时间明显减少[50]。机器人辅助技术、植入物设计和制造方面的技术进步在为患者提供更精确的截骨量和伸屈平衡间隙、更好的植入物方面发挥了作用,从而带来更好的术后结果、更快的康复和更短的住院时间。KAYANI等[51]证明与传统TKA组相比,RATKA组患者住院时间更短,RATKA的中位出院时间为77 h ,而传统夹具辅助TKA的中位出院时间为105 h;术后第2天(P=0.03)及以后RATKA组镇痛药用量更少。当然这与RATKA可以减少不必要的软组织释放、并且减少了医源性关节损伤有关。这一过程有助于限制局部炎症反应,减轻术后疼痛和肢体肿胀,从而增加出院时膝关节屈曲度,提高患者的满意度,缩短术后住院时间[32,52]。同时可以减少住院期间一些非阿片类药物的用量,并且患者出院后的康复治疗也相应减少,减轻了患者的医疗支出负担[35,50,53]。 RATKA与传统TKA创伤效应综合分析见表1。"

2.6 其他优势 一方面,有研究表明在机器人队列中术后24,72 h可溶性P-选择素的血清水平显著降低[54]。在接受常规TKA的受试者中,术后24,72 h观察到血清可溶性P-选择素更显著的激增。相关文献表明,血清可溶性P-选择素水平与TAK术后急性心肌梗死和静脉血栓栓塞症发生有关,血浆可溶性P-选择素的浓度与Gensini评分、血管病变数量和冠状动脉病变类型呈正相关[55]。另一方面,RATKA术后血红蛋白水平下降较少;相关研究发现两组术前血红蛋白浓度无统计学差异,术后与RATKA患者相比传统TKA组患者血红蛋白减少更多(P < 0.001)。此外,在传统术中固定截骨器械会产生不同数量钉道,对于患者来说也是创伤,而 RATKA 技术无需行股骨髓内定位及胫骨髓外定位,与前者相比相对微创。并且RATKA术中使用磨钻或者较传统术中使用的更轻薄的往复锯截骨,可以减少对骨床不必要的创伤,为后期翻修手术奠定良好基础。"

| [1] KIM CW, LEE CR, GWAK HC, et al. The Effects of Surgical Technique in Total Knee Arthroplasty for Varus Osteoarthritic Knee on the Rotational Alignment of Femoral Component: Gap Balancing Technique versus Measured Resection Technique. J Knee Surg. 2020;33(2):144-151. [2] FENG B, ZHU W, BIAN YY, et al. China artificial joint annual data report. Chin Med J (Engl). 2020;134(6):752-753. [3] REGINSTER JY. The prevalence and burden of arthritis . Rheumatology (Oxford). 2002;41 Supp 1:3-6. [4] KARTHIK K, COLEGATE-STONE T, DASGUPTA P, et al. Robotic surgery in trauma and orthopaedics: a systematic review . Bone Joint J. 2015;97-b(3):292-299. [5] XU Z, LI H, LIU Z, et al. Robot-assisted surgery in total knee arthroplasty: trauma maker or trauma savior? A prospective, randomized cohort study. Burns Trauma. 2022;10:tkac034. [6] GRIFFIN FM, INSALL JN, SCUDERI GR. Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty. 2000;15(8):970-973. [7] MIHALKO WM, WHITESIDE LA, KRACKOW KA. Comparison of ligament-balancing techniques during total knee arthroplasty. J Bone Joint Surg Am. 2003;85-A Suppl 4:132-135. [8] WHITESIDE LA, SAEKI K, MIHALKO WM. Functional medical ligament balancing in total knee arthroplasty. Clin Orthop Relat Res. 2000;(380):45-57. [9] JAFFE WL, DUNDON JM, CAMUS T. Alignment and Balance Methods in Total Knee Arthroplasty. J Am Acad Orthop Surg. 2018;26(20):709-716. [10] PETERS CL, JIMENEZ C, ERICKSON J, et al. Lessons learned from selective soft-tissue release for gap balancing in primary total knee arthroplasty: an analysis of 1216 consecutive total knee arthroplasties: AAOS exhibit selection . J Bone Joint Surg Am. 2013;95(20):e152. [11] MA Y, CHEN WJ, NAGAMINE R. Comparative evaluation of posterior cruciate ligament in total knee arthroplasty. J Orthop Surg (Hong Kong). 2017;25(1): 2309499017690976. [12] KHLOPAS A, CHUGHTAI M, HAMPP EL, et al. Robotic-Arm Assisted Total Knee Arthroplasty Demonstrated Soft Tissue Protection. Surg Technol Int. 2017;30: 441-446. [13] HAMPP EL, SODHI N, SCHOLL L, et al. Less iatrogenic soft-tissue damage utilizing robotic-assisted total knee arthroplasty when compared with a manual approach: A blinded assessment. Bone Joint Res. 2019;8(10):495-501. [14] XIA R, TONG Z, HU Y, et al. ‘Skywalker’ surgical robot for total knee arthroplasty: An experimental sawbone study. Int J Med Robot. 2021;17(5):e2292. [15] KAYANI B, KONAN S, PIETRZAK JRT, et al. Iatrogenic Bone and Soft Tissue Trauma in Robotic-Arm Assisted Total Knee Arthroplasty Compared With Conventional Jig-Based Total Knee Arthroplasty: A Prospective Cohort Study and Validation of a New Classification System. J Arthroplasty. 2018;33(8):2496-2501. [16] SIEBERT W, MAI S, KOBER R, et al. Technique and first clinical results of robot-assisted total knee replacement. Knee. 2002;9(3):173-180. [17] KAYANI B, KONAN S, AYUOB A, et al. Robotic technology in total knee arthroplasty: a systematic review . EFORT Open Rev. 2019;4(10):611-617. [18] HAMPP EL, CHUGHTAI M, SCHOLL LY, et al. Robotic-Arm Assisted Total Knee Arthroplasty Demonstrated Greater Accuracy and Precision to Plan Compared with Manual Techniques. J Knee Surg. 2019;32(3):239-350. [19] THILAK J, BABU BC, THADI M, et al. Accuracy in the Execution of Pre-operative Plan for Limb Alignment and Implant Positioning in Robotic-arm Assisted Total Knee Arthroplasty and Manual Total Knee Arthroplasty: A Prospective Observational Study. Indian J Orthop. 2021;55(4):953-960. [20] BÄTHIS H, PERLICK L, TINGART M, et al. Intraoperative cutting errors in total knee arthroplasty. Arch Orthop Trauma Surg. 2005;125(1):16-20. [21] MASON JB, FEHRING TK, ESTOK R, et al. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 2007;22(8): 1097-1106. [22] CLEMENT ND, WEIR DJ, DEEHAN DJ. Robotic-arm Assisted Total Knee Arthroplasty: the Relationship between Bone Resection, Gap Balancing and Resultant Implant Alignment. Arch Bone Jt Surg. 2023;11(4):278-284. [23] HEIM CE, YAMADA KJ, FALLET R, et al. Orthopaedic Surgery Elicits a Systemic Anti-Inflammatory Signature. J Clin Med. 2020;9(7):2123. [24] LANGKILDE A, JAKOBSEN TL, BANDHOLM TQ, et al. Inflammation and post-operative recovery in patients undergoing total knee arthroplasty-secondary analysis of a randomized controlled trial. Osteoarthritis Cartilage. 2017;25(8): 1265-1273. [25] ZHANG S, HUANG Q, XIE J, et al. Factors influencing postoperative length of stay in an enhanced recovery after surgery program for primary total knee arthroplasty. J Orthop Surg Res. 2018;13(1):29. [26] HECHT CJ, 2ND, BURKHART RJ, KARIMI AH, et al. What is the Association Between Clinically Diagnosed Psychiatric Illness and Total Joint Arthroplasty? A Systematic Review Evaluating Outcomes, Healthcare Use, and Patient-reported Outcome Measures. Clin Orthop Relat Res. 2023;481(5):947-964. [27] BIAN T, SHAO H, ZHOU Y, et al. Does psychological distress influence postoperative satisfaction and outcomes in patients undergoing total knee arthroplasty? A prospective cohort study. BMC Musculoskelet Disord. 2021;22(1):647. [28] LEE NK, WON SJ, LEE JY, et al. Presence of Night Pain, Neuropathic Pain, or Depressive Disorder Does Not Adversely Affect Outcomes After Total Knee Arthroplasty: A Prospective Cohort Study. J Korean Med Sci. 2022;37(43):e309. [29] GOH GS, LIOW MHL, TAY YWA, et al. The long-term impact of preoperative psychological distress on functional outcomes, quality of life, and patient satisfaction after total knee arthroplasty. Bone Joint J. 2020;102-b(7):845-851. [30] HARMER JR, WYLES CC, DUONG SQ, et al. Depression and anxiety are associated with an increased risk of infection, revision, and reoperation following total hip or knee arthroplasty. Bone Joint J. 2023;105-b(5):526-533. [31] RU YF, HE RX. [Early clinical application of Mako robot-assisted total knee arthroplasty in knee osteoarthritis. Zhongguo Gu Shang. 2023;36(2):133-139. [32] SAMUEL LT, KARNUTA JM, BANERJEE A, et al. Robotic Arm-Assisted versus Manual Total Knee Arthroplasty: A Propensity Score-Matched Analysis. J Knee Surg. 2023; 36(1):105-114. [33] JOO PY, CHEN AF, RICHARDS J, et al. Clinical results and patient-reported outcomes following robotic-assisted primary total knee arthroplasty : a multicentre study. Bone Jt Open. 2022;3(8):589-595. [34] BHIMANI SJ, BHIMANI R, SMITH A, et al. Robotic-assisted total knee arthroplasty demonstrates decreased postoperative pain and opioid usage compared to conventional total knee arthroplasty. Bone Jt Open. 2020;1(2):8-12. [35] GREGORY DA, COPPOLECCHIA A, SCOTTI DJ, et al. A 90-Day Episode-of-Care Analysis Including Computed Tomography Scans of Robotic-Arm Assisted versus Manual Total Knee Arthroplasty. J Knee Surg. 2022. doi: 10.1055/s-0042-1749083. [36] CLARK G, STEER R, TIPPETT B, et al. Short-Term Benefits of Robotic Assisted Total Knee Arthroplasty Over Computer Navigated Total Knee Arthroplasty Are Not Sustained With No Difference in Postoperative Patient-Reported Outcome Measures. Arthroplast Today. 2022;14:210-5.e0. [37] MARCHAND RC, SODHI N, KHLOPAS A, et al. Patient Satisfaction Outcomes after Robotic Arm-Assisted Total Knee Arthroplasty: A Short-Term Evaluation. J Knee Surg. 2017;30(9):849-853. [38] GREINER JJ, WANG JF, MITCHELL J, et al. Opioid Use in Robotic-Arm Assisted Total Knee Arthroplasty: A Comparison to Conventional Manual Total Knee Arthroplasty. Surg Technol Int. 2020;37:280-289. [39] RICE DA, KLUGER MT, MCNAIR PJ, et al. Persistent postoperative pain after total knee arthroplasty: a prospective cohort study of potential risk factors. Br J Anaesth. 2018;121(4):804-812. [40] KAYANI B, KONAN S, TAHMASSEBI J, et al. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J. 2018;100-b(7):930-937. [41] OELSNER WK, ENGSTROM SM, BENVENUTI MA, et al. Characterizing the Acute Phase Response in Healthy Patients Following Total Joint Arthroplasty: Predictable and Consistent. J Arthroplasty. 2017;32(1):309-314. [42] WINDISCH C, BRODT S, ROEHNER E, et al. The C-reactive protein level after total knee arthroplasty is gender specific. Knee Surg Sports Traumatol Arthrosc. 2016;24(10):3163-3167. [43] XU JZ, LI LL, FU J, et al. Comparison of serum inflammatory indicators and radiographic results in MAKO robotic-assisted versus conventional total knee arthroplasty for knee osteoarthritis: a retrospective study of Chinese patients. BMC Musculoskelet Disord. 2022;23(1):418. [44] PABINGER I, AY C. Biomarkers and venous thromboembolism. Arterioscler Thromb Vasc Biol. 2009;29(3):332-336. [45] RIVA N, VELLA K, HICKEY K, et al. Biomarkers for the diagnosis of venous thromboembolism: D-dimer, thrombin generation, procoagulant phospholipid and soluble P-selectin. J Clin Pathol. 2018;71(11):1015-1022. [46] MITANI G, TAKAGAKI T, HAMAHASHI K, et al. Associations between venous thromboembolism onset, D-dimer, and soluble fibrin monomer complex after total knee arthroplasty. J Orthop Surg Res. 2015;10:172. [47] ADAM SS, KEY NS, GREENBERG CS. D-dimer antigen: current concepts and future prospects. Blood. 2009;113(13):2878-2887. [48] TAN M, VAN ROODEN CJ, WESTERBEEK RE, et al. Diagnostic management of clinically suspected acute deep vein thrombosis. Br J Haematol. 2009;146(4): 347-360. [49] SIU KK, WU KT, KO JY, et al. Effects of computer-assisted navigation versus the conventional technique for total knee arthroplasty on levels of plasma thrombotic markers: a prospective study. Biomed Eng Online. 2019;18(1):99. [50] MONT MA, KHLOPAS A, CHUGHTAI M, et al. Value proposition of robotic total knee arthroplasty: what can robotic technology deliver in 2018 and beyond?. Expert Rev Med Devices. 2018;15(9):619-630. [51] KAYANI B, TAHMASSEBI J, AYUOB A, et al. A prospective randomized controlled trial comparing the systemic inflammatory response in conventional jig-based total knee arthroplasty versus robotic-arm assisted total knee arthroplasty. Bone Joint J. 2021;103-b(1):113-122. [52] KAYANI B, KONAN S, TAHMASSEBI J, et al. An assessment of early functional rehabilitation and hospital discharge in conventional versus robotic-arm assisted unicompartmental knee arthroplasty: a prospective cohort study. Bone Joint J. 2019;101-b(1):24-33. [53] ONG KL, COPPOLECCHIA A, CHEN Z, et al. Robotic-Arm Assisted Total Knee Arthroplasty: Cost Savings Demonstrated at One Year . Clinicoecon Outcomes Res. 2022;14:309-318. [54] KUO SJ, SIU KK, WU KT, et al. The Differential Systemic Biological Effects between Computer Navigation and Conventional Total Knee Arthroplasty (TKA) Surgeries: A Prospective Study. J Pers Med. 2022;12(11):1835. [55] QU XB, SUN ZQ, CHEN MJ, et al. The study of soluble P-selectin levels and it’s correlation to the severity of coronary artery lesions in coronary heart disease. Zhonghua Liu Xing Bing Xue Za Zhi. 2005;26(8):617-621. [56] NARKBUNNAM R, PORNRATTANAMANEEWONG C, RUANGSOMBOON P, et al. Alignment accuracy and functional outcomes between hand-held navigation and conventional instruments in TKA: a randomized controlled trial. BMC Musculoskelet Disord. 2022;23(1):1017. [57] ZHAO HY, YEERSHENG R, KANG XW, et al. The effect of tourniquet uses on total blood loss, early function, and pain after primary total knee arthroplasty: a prospective, randomized controlled trial. Bone Joint Res. 2020;9(6):322-332. [58] LOOMANS L, LEIRS G, VANDENNEUCKER H. Operating room efficiency after the implementation of MAKO robotic-assisted total knee arthroplasty. Arch Orthop Trauma Surg. 2023. doi: 10.1007/s00402-023-04834-w. [59] NOGALO C, MEENA A, ABERMANN E, et al. Complications and downsides of the robotic total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2023;31(3):736-750. [60] RAJ S, BOLA H, YORK T. Robotic-assisted knee replacement surgery & infection: A historical foundation, systematic review and meta-analysis. J Orthop. 2023;40: 38-46. [61] LIOW MHL, GOH GS, WONG MK, et al. Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(9): 2942-2951. [62] MONT MA, COOL C, GREGORY D, et al. Health Care Utilization and Payer Cost Analysis of Robotic Arm Assisted Total Knee Arthroplasty at 30, 60, and 90 Days. J Knee Surg. 2021;34(3):328-337. |
| [1] | Li Yongjie, Fu Shenyu, Xia Yuan, Zhang Dakuan, Liu Hongju. Correlation of knee extensor muscle strength and spatiotemporal gait parameters with peak knee flexion/adduction moment in female patients with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1354-1358. |
| [2] | Shan Jiaxin, Zhang Yilong, Wu Hongtao, Zhang Jiayuan, Li Anan, Liu Wengang, Xu Xuemeng, Zhao Chuanxi. Changes in muscle strength and pain in patients receiving Jianpi Yiqi Huoxue Formula after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1378-1382. |
| [3] | Qi Haodong, Lu Chao, Xu Hanbo, Wang Mengfei, Hao Yangquan. Effect of diabetes mellitus on perioperative blood loss and pain after primary total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1383-1387. |
| [4] | Li Xiaoqiang, Chen Wei, Li Mingyue, Shan Tianchi, Shen Wen. Value of preoperative quantitative ultrasound analysis of quadriceps femoris in predicting chronic post-surgical pain after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1388-1393. |
| [5] | Du Changling, Shi Hui, Zhang Shoutao, Meng Tao, Liu Dong, Li Jian, Cao Heng, Xu Chuang. Efficacy and safety of different applications of tranexamic acid in high tibial osteotomy [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1409-1413. |
| [6] | Huang Xiarong, Hu Lizhi, Sun Guanghua, Peng Xinke, Liao Ying, Liao Yuan, Liu Jing, Yin Linwei, Zhong Peirui, Peng Ting, Zhou Jun, Qu Mengjian. Effect of electroacupuncture on the expression of P53 and P21 in articular cartilage and subchondral bone of aged rats with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1174-1179. |
| [7] | Li Rui, Zhang Guihong, Wang Tao, Fan Ping. Effect of ginseng polysaccharide on the expression of prostaglandin E2/6-keto-prostaglandin 1alpha in traumatic osteoarthritis model rats [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1235-1240. |
| [8] | Wang Tihui, Wang Xu, Wu Jinqing, Chen Jiliang, Wang Xiaolu, Miao Juan. Application of three-dimensional simulated osteotomy of the distal femur in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 905-910. |
| [9] | Zhao Rushun, Hao Yangquan, Xu Peng, Zheng Xin, Jiang Yonghong, Zhang Yuting, Wang Mengfei, Lu Chao. Effect of different locations of necrotic focus on the natural course of non-traumatic osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 917-921. |
| [10] | Yang Yifeng, Huang Jian, Ye Nan, Wang Lin. Ischemia-reperfusion injury in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 955-960. |
| [11] | Zhang Zeyi, Yang Yimin, Li Wenyan, Zhang Meizhen. Effect of foot progression angle on lower extremity kinetics of knee osteoarthritis patients of different ages: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 968-975. |
| [12] | Shen Feiyan, Yao Jixiang, Su Shanshan, Zhao Zhongmin, Tang Weidong. Knockdown of circRNA WD repeat containing protein 1 inhibits proliferation and induces apoptosis of chondrocytes in knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 499-504. |
| [13] | Liu Yuhan, Fan Yujiang, Wang Qiguang. Comparison of protocols for constructing animal models of early traumatic knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 542-549. |
| [14] | Wang Xinmin, Yan Wenkai, Song Yahui, Liu Fei. Leukocyte- and platelet-rich fibrin with autologous hamstring tendon for traumatic patella dislocation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 404-410. |
| [15] | Li Chun, Zhang Yanlin, Liu Di, Wang Minglei, Wang Duo, Liu Junwei, Wu Yongli. Effect of warm-needling moxibustion on anterior cruciate ligament injury repair and related growth factors in rabbits with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3621-3626. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||