Chinese Journal of Tissue Engineering Research ›› 2018, Vol. 22 ›› Issue (11): 1781-1785.doi: 10.3969/j.issn.2095-4344.0179
Previous Articles Next Articles
Asymptomatic bacteriuria before arthroplasty
Zhang Qing-yu1, Gao Fu-qiang2, Sun Wei2
- 1China-Japan Friendship Hospital, Peking Union Medical College, Beijing 100029, China; 2First Department of Orthopedics,Osteonecrosis and Joint Reservation Reconstruction Center, China-Japan Friendship Hospital, Beijing 100029, China
-
Online:2018-04-18Published:2018-04-18 -
Contact:Sun Wei, Chief physician, Professor, Doctoral supervisor, Master’s supervisor, First Department of Orthopedics, Osteonecrosis and Joint Reservation Reconstruction Center, China-Japan Friendship Hospital, Beijing 100029, China -
About author:Zhang Qing-yu, Doctoral candidate, China-Japan Friendship Hospital, Peking Union Medical College, Beijing 100029, China -
Supported by:the General Project of National Natural Science Foundation of China, No. 81372013 and 81672336
CLC Number:
Cite this article
Zhang Qing-yu, Gao Fu-qiang, Sun Wei. Asymptomatic bacteriuria before arthroplasty[J]. Chinese Journal of Tissue Engineering Research, 2018, 22(11): 1781-1785.
share this article
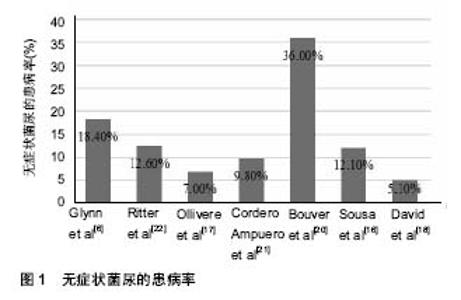
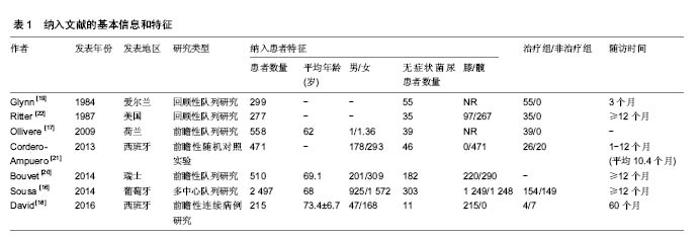
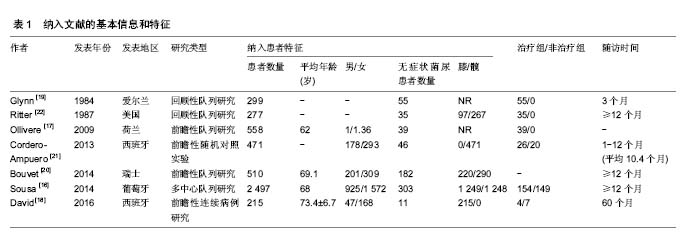
2.1 关节置换术前无症状菌尿的患病率 纳入的7项研究报道的无症状菌尿在关节置换术患者中的患病率并不一致,最低的只有5.1%,最高达到36.0%(图1),这与不同研究中对无症状菌尿的定义、纳入的人群特征和采样过程等有关。大部分研究将清洁中段尿培养结果>105 CFU/mL定义为阳性[16-19,21-22],而Bouvet等[20]采用了一种并不常用的诊断标准,即将尿培养结果>103 CFU/mL定义为阳性,因此其阳性率明显高于其他研究。仅来自同一中心的2项研究在纳入患者时排除了围手术期留置导尿管的患者,而围手术期导尿被认为是关节置换术后感染的一项危险因素,而且这2项研究分别只纳入髋关节置换和膝关节置换患者,在样本留取和细菌培养等操作方面具有同质性[18,21]。其结果显示单纯股骨头置换的患者中无症状菌尿的患病率高于全髋关节置换的患者,这主要是由于与后者相比,前者的年龄更大,且常常来自急诊。"

2.2 无症状菌尿是关节置换术后假体周围感染的独立危险因素 假体周围感染是关节置换术后最为可怕的并发症之一,患者需要应用抗菌药物和手术干预[23-25]。目前关节置换术后假体周围感染的发生率在1%左右,如何采 取措施预防假体周围感染的发生是骨科医生面临的问题[26-28]。在本文纳入的文献中,有4项研究了关节置换术前无症状菌尿和假体周围感染的关系,其中2项分别只研究髋和膝关节置换的患者[18,21],另外2项则同时纳入了髋膝关节置换患者[16,22]。 一项随机对照试验纳入了471例行髋关节置换术且无尿路症状和围手术期导尿的患者,发现无症状菌尿患者共46例并将其分为特异性抗生素治疗组和非治疗组,治疗组给予尿培养结果敏感的特异性抗生素治疗7 d。随访期间共发现13例假体周围感染,仅有1例发生于尿培养阳性的患者,且该患者属于治疗组,培养出的病原体类型也和术前泌尿系感染的不相同[21]。来自同一中心的另一前瞻性研究则纳入了215例接受全膝关节置换的患者,最终发现无症状菌尿患者11例并分为2组,治疗组4例给予尿培养结果敏感的抗生素治疗,非治疗组7例患者则仅接受传统预防方案。术后随访至少4年,仅治疗组在术后第3个月有1例假体周围感染,而且细菌培养的结果同样与术前尿培养结果不同,非治疗组无假体周围感染发生[18]。Ritter等[22]则纳入了277例接受膝或髋关节置换术的患者,共发现35例术前无症状菌尿,术后随访至少1年,最长16年,期间发生3例假体周围感染均证实与术前的无症状菌尿无关。目前关于假体周围感染和术前无症状菌尿的最大规模的数据来自2014年发表的一项多中心队列研究,共纳入2 497例关节置换患者,术前尿培养发现无症状菌尿患者303例,多因素方差分析显示无症状菌尿是关节置换术后假体周围感染的独立危险因素(OR=3.95,95%CI: 1.52-10.26),然而,术前尿培养结果和术后假体深部分离出的病原体均不一致[16]。 2.3 关节置换术前无症状菌尿与术区浅表感染 术区的浅表感染常发生于术后前4周,大多数情况下并不需要手术干预,给予及时有效口服抗生素治疗多数能够痊愈。Glynn等[19]回顾性分析了299例接受髋/膝关节置换的患者,其中55例患者存在术前无症状菌尿,均在围手术期行10 d微生物敏感的抗生素治疗。随访3个月,2例浅表感染,术前尿培养结果均示大肠埃希菌,术后切口细菌培养则均示葡萄球菌,作者在结论中虽然建议对术前无症状菌尿给予对症的口服抗生素治疗,但他们的结果并不能很好的支持这一观点。在另一项纳入558例接受择期关节置换患者的研究中,39例术前患无症状菌的患者均接受抗生素治疗,但其术后切口延迟愈合或细菌培养阳性的发生率仍要明显高于无菌尿患者(P < 0.02),采用单因素方差分析的方法,无症状菌尿组发生各种切口事件的概率约是其他患者的2.4倍[17]。 2.4 患无症状菌尿的患者有着较高的治疗后泌尿系感染复发率 在关节置换术前1 d及术后第3天,Bouvet等[20]对510例术前无泌尿系症状的患者行尿培养,术前常规头孢呋辛预防感染,该抗生素的抗菌谱能够覆盖65%术前菌尿,但术后尿培养结果显示菌尿患病率并未下降,而且手术前后尿培养结果的相符率只有49%,头孢呋辛的抗菌谱对术后菌尿的覆盖率则降到了11%;术后25例患者有尿路感染症状,其中超过2/3的尿培养结果与术前不一致。Glynn等[19]的数据指出大肠埃希菌感染占术前无症状菌尿的78%,然而只占术后泌尿系感染的39%。Sousa等[16]则表明无症状菌尿组的术后尿路感染发生率并不较无菌尿组高(OR=1.74,95%CI: 0.65-4.64)。这些研究说明患有无症状菌尿的患者具有较高的治疗后泌尿系感染复发率。 2.5 无症状菌尿患者术后感染并发症发生的原因 综合纳入的研究,作者发现术前患有无症状菌尿的患者在术后有着较高的假体周围及浅表术区的感染率,即使给予有效的抗生素治疗,也并不能降低这些危险事件的发生。术前无症状菌尿是关节置换术后假体周围感染的独立危险因素,而且很可能是术区浅表感染的危险因素,但在所有研究中,并没有发现1例术后感染是术前泌尿系感染通过直接或血源性播散导致的,这表明术前无症状菌尿与关节置换术后感染之间并不是直接的因果关系。对于这一现象目前并没有可靠的解释。作者注意到,患无症状菌尿的患者有着较高的泌尿系感染复发率,即使给予相关治疗,也会在很短时间内复发,而且治疗后感染的病原体种类与治疗前相比存在着较大的差异[19-20]。复发的尿路感染可能是导致关节置换术后假体周围感染的来源之一,但相关研究中并未在抗生素治疗结束后再次复查尿培养。另一种可能的解释是无症状菌尿患者皮肤菌群的构成具有特异性,在Sousa等[16]的研究中,43例假体周围感染中有32例发生于术后前6周,提示手术中污染的可能性很大,同时作者指出,发生于无症状菌尿患者的假体周围感染中,培养结果示革兰阴性菌的比例要明显高于发生于无菌尿患者。Ollivere等[17]也指出无症状菌尿患者和无菌尿患者在发生浅表术区感染时,培养结果示厌氧菌的比例具有明显的差异。由于目前的研究数量和质量有限,术前无症状菌尿患者在关节置换术后有着较高假体周围和浅表术区感染率的原因尚需进一步验证。 2.6 指南中关于关节置换术前无症状菌尿的意见 关于如何处理关节置换术前的无症状菌尿,相关的国际指南中给出的建议并不多。英国骨科协会关于初次全髋关节置换术的指南支持术前常规尿液筛查,但并没有指出无症状菌尿是否需要治疗[29]。苏格兰校际指南网(Scottish Intercollegiate Guidelines Network,SIGN)和国家卫生医疗质量标准署(National Institute for Health and Care Excellence,NICE)则指出除了怀孕状况下,患无症状菌尿的患者并不需要在骨科手术前接受特异性抗生素治疗[30]。2013年的一份关于骨科感染的国际指南也指出关节置换术前常规尿路筛查不再是必须的,除非患者既往或现在有尿路感染的症状[31]。 2.7 对无症状菌尿的治疗并不能给关节置换患者带来明显收益 一项研究将患有无症状菌尿的女性随机分为治疗组和非治疗组,治疗组在随访过程中有症状的尿路感染发病率并没有改善,同时,治疗的不良反应,如抗生素抵抗、艰难梭菌感染等显著增多[32-33]。有文献指出,等到尿路感染的症状出现时,有足够的时间开始有针对性的抗生素治疗以避免尿路脓毒症和血源性传播导致的假体周围感染[34]。Ollivere等[17]虽然对所有术前患无症状菌尿的患者进行了有效的抗生素治疗,但切口不愈合和浅表感染的发生率仍然要明显高于无菌尿患者,因此并不能证明这一措施的有效性。Sousa等[16]研究者非随机地将术前患无症状菌尿的患者分为治疗组(154例)和非治疗组(149例),结果显示对术前无症状菌尿的治疗也不能降低术后假体周围感染的发生率(OR=0.82,95% CI:0.27-2.51)。 虽然尿培养的费用并不昂贵,但如果常规对患者进行筛查和治疗,考虑到中国每年巨大的关节置换数量,总的费用也将是巨大的[35]。美国一项1989年的调查显示,常规对膝关节置换术前的患者进行尿培养,每预防1例因尿路感染引起的关节置换术后切口感染,约需花费150万美元用于术前的尿培养和治疗[36]。而且,对菌尿的筛查和治疗会推迟手术的进行,延长治疗时间,增加患者的痛苦。 2.8 纳入文献质量和本研究存在的不足 必须承认,本研究仍然存在着许多不足。首先,纳入研究的质量较低。关于本课题仅有一项小规模的随机对照试验[21],其他均为观察性研究。同时,仅一项试验纳入患者总数超过 1 000[16],然而该研究的分配并不是随机的,且同时纳入了行不同部位关节置换的患者和行围手术期导尿的患者,这均会给结果带来偏倚。Ollivere等[17]的研究指出了术前无症状菌尿和术区浅表感染的关系,然而他们仅采取单因素方差分析的方法,未考虑到其他可能的危险因素,且未对术前尿培养和术后皮肤拭子的培养结果进行说明,因此术前无症状菌尿是否是术区浅表事件的独立危险因素尚待进一步研究。其次,目前关于关节置换术前无症状菌尿的研究是非常有限的,而且大多数都存在病例数量较少,说服力差等缺陷,无法进行有效的统计学分析和归纳。第三,不同研究之间的异质性很大,包括实验设计方案、纳入的人群特征、抗生素治疗方案的选择以及报道的无症状菌尿的患病率等。最后,纳入的研究在进行针对无症状菌尿的治疗后,大都未再次行尿培养评估治疗的效果。"

| [1] Cordero-Ampuero J, de Dios M. What are the risk factors for infection in hemiarthroplasties and total hip arthroplasties? Clin Orthop Relat Res. 2010; 468:3268-3277.[2] Salvati EA, Gonzalez DVA, Masri BA, et al. The infected total hip arthroplasty. Instr Course Lect. 2003; 52:223-245.[3] Cruess RL, Bickel WS, VonKessler KL. Infections in total hips secondary to a primary source elsewhere. Clin Orthop Relat Res. 1975;106:99-101.[4] Hall AJ. Late infection about a total knee prosthesis. Report of a case secondary to urinary tract infection. J Bone Joint Surg Br. 1974;1:144-147.[5] Aizen E, Shifrin B, Shugaev I, et al. Clinical and microbiological outcomes of asymptomatic bacteriuria in elderly stroke patients. Isr Med Assoc J. 2017;19(3):147-151.[6] Ramos JA, Lemos EV, Ruano-Ravina A. Duration of surgical antibiotic prophylaxis in patients with asymptomatic bacteriuria. Lancet Infect Dis. 2017;4:370.[7] Nicolle LE, Bradley S, Colgan R, et al. Infectious Diseases Society of America Guidelines for the Diagnosis and Treatment of Asymptomatic Bacteriuria in Adults. Clin Infect Dis.2005;5:643-654.[8] Gleckman R, Esposito A, Crowley M, et al. Reliability of a single urine culture in establishing diagnosis of asymptomatic bacteriuria in adult males. J Clin Microbiol. 1979;5:596-597.[9] Nicolle LE. Asymptomatic Bacteriuria: When to screen and when to treat. Infect Dis Clin North Am. 2003;2:367-394.[10] Bengtsson C, Bengtsson U, Bjorkelund C, et al. Bacteriuria in a population sample of women: 24-year follow-up study. Results from the prospective population-based study of women in Gothenburg, Sweden. Scand J Urol Nephrol. 1998; 32(4):284-289.[11] David TS, Vrahas MS. Perioperative lower urinary tract infections and deep sepsis in patients undergoing total joint arthroplasty. J Am Acad Orthop Surg. 2000;1:66-74.[12] Rajamanickam A, Noor S, Usmani A. Should an asymptomatic patient with an abnormal urinalysis (Bacteriuria or Pyuria) be treated with antibiotics prior to major joint replacement surgery? Cleve Clin J Med. 2007:S17-S18.[13] Otermin I, Rivero M, Hidalgo A. Is it necessary to delay or to put off surgery in the case of possible asymptomatic bacteriuria and orthopaedic surgery with implants? Enferm Infecc Microbiol Clin. 2009;4:252-253.[14] Finnigan TKP, Bhutta MA, Shepard GJ. Asymptomatic bacteriuria prior to arthroplasty: how do you treat yours?[C]//Orthopaedic Proceedings. Orthop Proc. 2012; 94(SUPP XXIX): 58-58[15] Leis JA, Rebick GW, Daneman N, et al. Reducing antimicrobial therapy for asymptomatic bacteriuria among noncatheterized inpatients: a proof-of-concept study. Clin Infect Dis. 2014;7:980-983.[16] Sousa R, Munoz-Mahamud E, Quayle J, et al. Is Asymptomatic Bacteriuria a Risk Factor for Prosthetic Joint Infection? Clin Infect Dis. 2014;1:41-47.[17] Ollivere BJ, Ellahee N, Logan K, et al. Asymptomatic Urinary Tract Colonisation Predisposes to Superficial Wound Infection in Elective Orthopaedic Surgery. Int Orthop. 2009;3:847-850.[18] Martinez-Velez D, Gonzalez-Fernandez E, Esteban J, et al. Prevalence of asymptomatic bacteriuria in knee arthroplasty patients and subsequent risk of prosthesis infection. Eur J Orthop Surg Traumatol. 2016;2:209-214.[19] Glynn MK, Sheehan JM. The significance of asymptomatic bacteriuria in patients undergoing hip/knee arthroplasty. Clin Orthop Relat Res. 1984;(185):151-154.[20] Bouvet C, Lubbeke A, Bandi C, et al. Is there any benefit in pre-operative urinary analysis before elective total joint replacement? Bone Joint J. 2014;3:390-394.[21] Cordero-Ampuero J, Gonzalez-Fernandez E, Martinez-Velez D, et al. Are antibiotics necessary in hip arthroplasty with asymptomatic bacteriuria? Seeding Risk With/Without Treatment. Clin Orthop Relat Res. 2013;12:3822-3829.[22] Ritter MA, Fechtman RW. Urinary tract sequelae: possible influence on joint infections following total joint replacement. Orthopedics. 1987;3:467-469.[23] Flury D, Behrend H, Sendi P, et al. Brucella melitensis prosthetic joint infection. J Bone Jt Infect. 2017;3:136-142.[24] Marang-van DMP, Bragan TE, Liew S, et al. Variation in prosthetic joint infection and treatment strategies during 4.5 years of follow-up after primary joint arthroplasty using administrative data of 41397 patients across Australian, European and United States Hospitals. BMC Musculoskelet Disord. 2017;1:207.[25] Wouthuyzen-Bakker M, Nijman JM, Kampinga GA, et al. Efficacy of antibiotic suppressive therapy in patients with a prosthetic joint infection. J Bone Jt Infect. 2017;2:77-83.[26] Kurtz SM, Lau E, Watson H, et al. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012;27(8 Suppl):61-65.e1. [27] Kurtz SM, Lau E, Schmier J, et al. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty. 2008;7:984-991.[28] Maderazo EG, Judson S, Pasternak H. Late infections of total joint prostheses. A review and recommendations for prevention. Clin Orthop Relat Res. 1988;229:131-142.[29] Primary total hip replacement: a guide to good practice. 3rd ed.British Orthopaedic Association,2012.[30] Scottish Intercollegiate Guidelines Network (SIGN).SIGN guideline 88. Management of suspected bacterial urinary tract infection in adults.http://www.sign.ac.uk/guidelines/fulltext/88/ recommendations.html[31] Parvizi J, Gehrke T, Chen AF. Proceedings of the international consensus on periprosthetic joint infection. Bone Joint J. 2013; 11:1450-1452.[32] Rotjanapan P, Dosa D, Thomas KS. Potentially inappropriate treatment of urinary tract infections in two rhode island nursing homes. Arch Intern Med. 2011;5:438-443.[33] Nicolle LE, Mayhew WJ, Bryan L. Prospective randomized comparison of therapy and no therapy for asymptomatic bacteriuria in institutionalized elderly women. Am J Med. 1987;1:27-33.[34] Pulido L, Ghanem E, Joshi A, et al. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res. 2008;7:1710-1715.[35] Lourenco T, Pickard R, Vale L, et al. Minimally invasive treatments for benign prostatic enlargement: systematic review of randomized controlled trials. BMJ. 2008;337:a1662. [36] Lawrence VA, Gafni A, Gross M. The unproven utility of the preoperative urinalysis: economic evaluation. J Clin Epidemiol.1989;12:1185-1192. |
| [1] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [2] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [3] | Li Dadi, Zhu Liang, Zheng Li, Zhao Fengchao. Correlation of total knee arthroplasty efficacy with satisfaction and personality characteristics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1346-1350. |
| [4] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [5] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [6] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [7] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [8] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [9] | Yuan Jiawei, Zhang Haitao, Jie Ke, Cao Houran, Zeng Yirong. Underlying targets and mechanism of Taohong Siwu Decoction in prosthetic joint infection on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1428-1433. |
| [10] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [11] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [12] | Zhao Zhongyi, Li Yongzhen, Chen Feng, Ji Aiyu. Comparison of total knee arthroplasty and unicompartmental knee arthroplasty in treatment of traumatic osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 854-859. |
| [13] | Liu Shaohua, Zhou Guanming, Chen Xicong, Xiao Keming, Cai Jian, Liu Xiaofang. Influence of anterior cruciate ligament defect on the mid-term outcome of fixed-bearing unicompartmental knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 860-865. |
| [14] | Zhang Nianjun, Chen Ru. Analgesic effect of cocktail therapy combined with femoral nerve block on total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 866-872. |
| [15] | Yuan Jun, Yang Jiafu. Hemostatic effect of topical tranexamic acid infiltration in cementless total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 873-877. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||