Chinese Journal of Tissue Engineering Research ›› 2013, Vol. 17 ›› Issue (9): 1703-1710.doi: 10.3969/j.issn.2095-4344.2013.09.027
Internal fixation with different implants for the treatment of old pelvic fractures
Zhang Li-cheng, Lan Xia, Zhang Li-hai, Tao Sheng, Zhang Qun, Liang Xiang-dang, Guo Yi-zhu, Tang Pei-fu
- Department of Orthopedics, General Hospital of Chinese PLA, Beijing 100853, China
-
Received:2012-09-10Revised:2012-11-15Online:2013-02-26Published:2013-02-26 -
Contact:Tang Pei-fu, Doctor, Chief physician, Department of Orthopedics, General Hospital of Chinese PLA, Beijing 100853, China pftang301@126.com -
About author:Zhang Li-cheng☆, Studying for doctorate, Physician, Department of Orthopedics, General Hospital of Chinese PLA, Beijing 100853, China zhanglcheng218@126.com
CLC Number:
Cite this article
Zhang Li-cheng, Lan Xia, Zhang Li-hai, Tao Sheng, Zhang Qun, Liang Xiang-dang, Guo Yi-zhu, Tang Pei-fu. Internal fixation with different implants for the treatment of old pelvic fractures[J]. Chinese Journal of Tissue Engineering Research, 2013, 17(9): 1703-1710.
share this article

2.1 陈旧性骨盆骨折不同植入物置入内固定治疗的临床病例 病例来源:2008年1月至2011年1月解放军总医院骨科共内固定治疗9例严重畸形愈合陈旧性骨盆骨折患者,其中男8例,女1例,平均年龄33.9岁(22-45岁)。内固定治疗时间为伤后87-165 d,平均 116.7 d。 致伤原因:有高坠伤3例,车祸撞击伤4例,车祸碾压伤1例,被轿车撞击后又被车轮碾压1例。8例因需先救治危及生命的内脏损伤而贻误了骨盆骨折的早期手术治疗,1例C2.1型骨盆骨折采用骨盆外固定支架固定。 骨折类型:采用Tile分型,C1.1型3例,C1.2型3例,C1.3型1例,C2.1型2例,9例患者骨折分类详细情况见表1。"

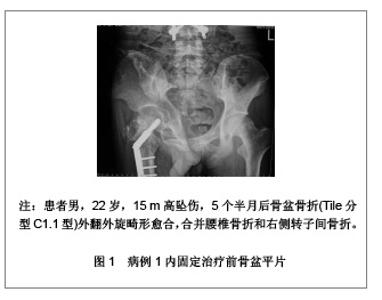
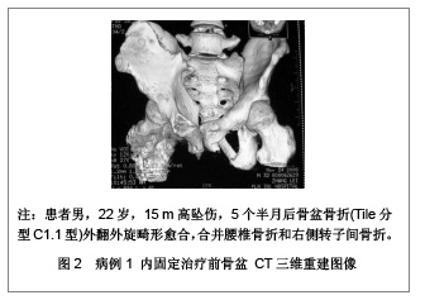
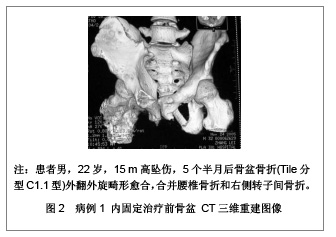
8例为完全稳定的畸形愈合,骨折线完全消失;1例为部分稳定的畸形愈合,骨折断端有骨痂形成,但骨折线未完全消失。早期合并损伤包括合并脑挫裂伤3例,膀胱破裂1例,尿道损伤2例,肠道破裂5例,脾破裂5例,肝破裂1例,血气胸4例,肺挫伤4例,多根肋骨骨折3例,腰椎骨折4例。 2.2 内固定治疗前临床症状评估 疼痛严重程度评估:9例患者中,8例为畸形愈合后骨盆的特定畸形引起的疼痛,1例为部分不稳引起的疼痛。内固定治疗前行走时持续性疼痛5例,严重疼痛不能行走2例,轻度间歇疼痛2例。 行走能力的评估:行走能力分为正常行走;跛行,但无需扶拐;须扶拐行走;扶拐有限行走;不能行走。9例患者内固定治疗前不能行走4例,扶拐有限行走5例。 其它临床症状评估:因双侧坐骨结节不对称引起坐姿不平衡4例;因骨盆旋转畸形引起平卧困难3例;双下肢不等长4例,患侧短缩分别为1.5 cm、2.0 cm、2.5 cm、3.0 cm,平均短缩2.25 cm。 2.3 内固定治疗前影像学评估 骨盆畸形的影像学评估主要依据标准前后位骨盆平片、入口和出口位片以及骨盆CT扫描和三维重建。文章研究中9例患者内、外旋畸形均大于30°。左侧内旋畸形愈合2例,左侧外旋畸形愈合2例,右侧外旋畸形愈合3例,右侧外旋畸形愈合合并左侧后环部分垂直不稳1例,左侧外旋畸形愈合合并右侧后环部分垂直不稳1例。典型病例见图1和图2。"
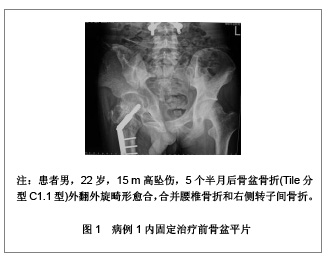
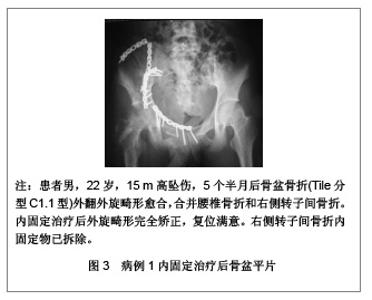
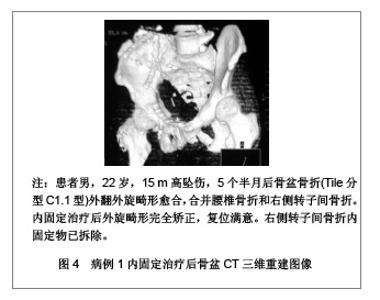
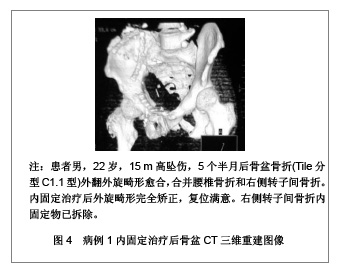
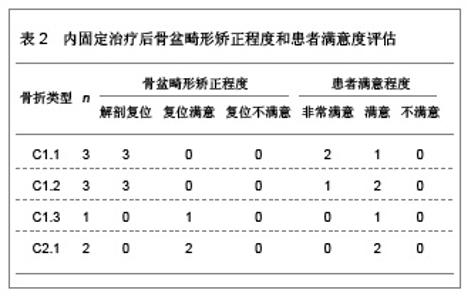
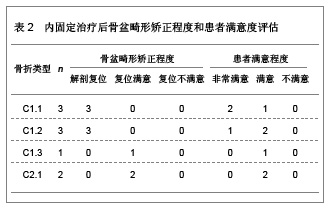
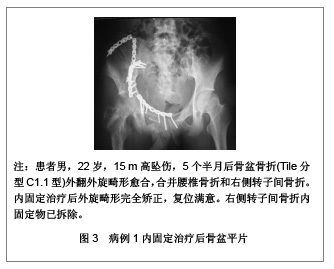
2.4 治疗方法 9例患者内固定治疗均在球囊导管临时完全阻断髂总动脉下进行。治疗前先在数字减影血管造影机监控下行患侧髂总动脉造影,采用Seldinger技术行健侧股动脉穿刺,于患侧髂总动脉分叉处的近端安置双腔球囊导管,在开始行骨盆截骨操作时,准确地在预定部位充盈球囊,实施患侧髂总动脉阻断。 治疗路径采用扩大的髂腹股沟入路。治疗过程主要包括:①截骨:首先显露骨盆前环,矫正前环畸形。9例患者中,8例患者耻骨上支骨折已畸形愈合,1例断端可见大量纤维骨痂形成。在原位截骨后,用髓核钳小心清除关节间隙的瘢痕组织,松解周围挛缩的软组织,用Cobb骨膜剥离器撬松关节后予纱布填塞,暂不固定,再显露骨盆后环,截骨复位固定后再固定前环。骨盆后环畸形的处理包括经髂骨截骨5例,骶骨外缘(1.5 cm内)截骨1例,骶髂关节切开3例。②复位:根据骨折和脱位的情况,通过患侧下肢牵引、复位钳提拉半骨盆、旋转耻骨联合及耻骨上支等使骨折获得复位。当骨折复位困难时,使用外固定支架等协助复位。在操作过程中,要注意保护坐骨神经,以免复位时过度牵拉。③内固定:耻骨联合、髂骨翼骨折均采用重建钢板固定5例,骶髂关节骨折和脱位采用重建钢板固定3例,合并骶骨骨折的骶髂复合体损伤采用重建钢板联合经皮骶髂空心拉力螺钉固定1例。④植骨:畸形矫正后,截骨断端会残留间隙,9例患者均于骨盆后环截骨处填充植骨,耻骨联合间植骨3例,骶髂关节切开翻转植骨融合3例。其中应用自体骨6例,同种异体骨2例,重组人骨形成蛋白复合骨替代材料1例。 术后于髂窝和方形区以及耻骨后间隙放置两三根引流管,平卧,股动脉穿刺部位压迫24 h。术后第1天开始主动背伸和跖屈踝关节,股四头肌主动等长收缩,促进下肢静脉血液回流,预防深静脉血栓。术后两三天24 h切口引流量少于50 mL即可拔出引流管,常规行双下肢以及髂总动脉血管超声检查,排除髂总动脉和深静脉血栓形成。所有患者均于术后4周、12周、24周、1年进行临床和放射学随访评估。 2.5 治疗结果 一般情况:手术时间为210-367 min,平均 290 min。球囊阻断持续时间45-90 min,平均 65 min。术中出血量700-2 800 mL,平均1 833 mL。切口引流量170-460 mL,平均260 mL,手术切口均甲级愈合。 随访效果:全部患者均获得随访12-48个月,平均随访24.8个月。 骨折愈合:骨折愈合时间为16-24周,平均20.6周,所有骨折都牢固愈合,无移位以及内固定的松动及断裂。 并发症:9例患者术后均未发生迟发性神经损伤,均未发生髂总动脉、下肢深静脉血栓形成以及肢体远端缺血性坏死。 内固定治疗后临床症状评估:治疗前行走时持续性疼痛5例,治疗后4例(4/5,80%)没有疼痛,1例(1/5,20%)残留轻度间歇疼痛,不需服用镇痛药物。治疗前严重疼痛不能行走的2例残留间歇疼痛,其中1例需服用镇痛药物。治疗前轻度间歇疼痛的2例,治疗后均没有疼痛。 治疗前不能行走4例,治疗后2例(2/4,50%)正常行走,1例(1/4,25%)轻度跛行,无需扶拐,1例(1/4,25%)因坐骨神经嵌压时间长,损伤重,腓总神经麻痹部分恢复,遗留踝关节僵硬,足跟不能着地,步态异常。治疗前扶拐有限行走5例,治疗后2例(2/5,40%)正常行走,1例(1/5,20%)轻度跛行,无需扶拐,1例(1/5,20%)因合并粗隆间骨折,遗留髋关节僵硬,跛行但无需扶拐,1例(1/5,20%)因股骨髁间粉碎骨折,遗留膝关节部分僵硬,轻度跛行但无需扶拐。 坐姿不平衡4例中3例完全矫正,1例残存轻度坐姿不平衡。因骨盆旋转畸形引起严重平卧困难的3例于术后均明显矫正。双下肢不等长4例矫正满意。 内固定治疗后影像学评估:治疗后拍摄标准前后位骨盆平片、入口和出口位片,根据Mears DC[11]报道的标准,骨盆畸形矫正的程度分为:①解剖复位。在标准前后位骨盆平片、入口和出口位片上均无残存移位。②复位满意。骨折垂直或向后移位的残存畸形小于1 cm,或在任何平面的旋转畸形角度小于15°。③复位不满意。骨折垂直或向后移位的残存畸形大于1 cm,或在任何平面的旋转畸形角度大于15°。文章研究9例患者中6例C1型骨折(6/9,67%)解剖复位,2例C2.1型骨折(2/9,22%)和1例C1.3型骨折(1/9,11%)复位满意。典型病例见图3和图4。"
| [1] Tile M. Fractures of the pelvis and acetabulum. 2nd cd. Baltimore: Williams and Wilkins, 2004:66-101.[2] Giannoudis PV, Grotz MR, Tzioupis C, et al. Prevalence of pelvic fractures, associated injuries, and mortality: the United Kingdom perspective. J Trauma. 2007;63(4):875-883. [3] Giannoudis PV, van Griensven M, Tsiridis E, et al. The genetic predisposition to adverse outcome after trauma. J Bone Joint Surg Br. 2007;89(10):1273-1279. [4] Archdeacon MT, Kuhlman G, Kazemi N. Fellow's Corner: Grand rounds from the University of Cincinnati Medical Center--painful superior and inferiorpubic rami nonunion. J Orthop Trauma. 2010;24(11):e109-112. [5] Jang DH, Byun SH, Jeon JY, et al. The relationship between lumbosacral plexopathy and pelvic fractures. Am J Phys Med Rehabil. 2011;90(9):707-712. [6] 程开明,侯波.不稳定骨盆骨折的手术治疗[J].中国实用医药, 2008, 3(13):124-125.[7] Shlamovitz GZ, Mower WR, Bergman J, et al. How (un)useful is the pelvic ring stability examination in diagnosing mechanically unstable pelvic fractures in blunt trauma patients? J Trauma. 2009;66(3):815-820. [8] Gruen GS, Leit ME, Gruen RJ, et al. The acute management of hemodynamically unstable multiple trauma patients with pelvic ring fractures. J Trauma. 1994;36(5):706-11; discussion 711-733. [9] 张军,郭克斌,熊元波,等.内固定加外固定架在不稳定型骨盆骨折治疗中的应用[J].中国实用医刊,2011,38(13):34-37.[10] 戴冲华,马斌.经皮骶髂螺钉固定治疗不稳定骨盆骨折28例疗效观察[J].亚太传统医药,2012,8(1):76-77.[11] Mears DC, Velyvis J. Surgical reconstruction of late pelvic post-traumatic nonunion and malalignment. J Bone Joint Surg Br. 2003;85(1):21-30. [12] Dickson KF, Matta JM. Skeletal deformity after anterior external fixation of the pelvis. J Orthop Trauma. 2009;23(5): 327-332. [13] Lindahl J, Hirvensalo E, Böstman O, et al. Failure of reduction with an external fixator in the management of injuries of the pelvic ring. Long-term evaluation of 110 patients. J Bone Joint Surg Br. 1999;81(6):955-962. [14] Kanakaris NK, Angoules AG, Nikolaou VS, et al. Treatment and outcomes of pelvic malunions and nonunions: a systematic review. Clin Orthop Relat Res. 2009; 467(8): 2112-2124. [15] 林志金,曹烈虎,沈锋,等.不稳定型骨盆骨折的金属植入物治疗[J].中国组织工程研究与临床康复,2010,14(9):1665-1668.[16] Pavelka T, Dzupa V, Stulík J, et al. Our results of surgical management of unstable pelvic ring injuries. Acta Chir Orthop Traumatol Cech. 2007;74(1):19-28. [17] Rommens PM. Is there a role for percutaneous pelvic and acetabular reconstruction? Injury. 2007;38(4):463-477. [18] 何文奇,李成山.重建钢板治疗不稳定骨盆骨折合并髋臼骨折[J].中国社区医师:医学专业,2010,12(15):113.[19] 吕涛,吕元杰,胡春明.骨盆骨折的临床治疗进展与展望[J].吉林医学,2005,26(1):97-99.[20] 张前法,庞清江,葛志斌,等.骨盆后环损伤内固定重建方法的选择[J].中国修复重建外科杂志,2006,20(12):1214-1216.[21] 卢珂恩,陈航,吴少科,等.不稳定型骨盆骨折的手术治疗[J].黑龙江医学,2012,36(6):452-454.[22] 马梦昆,李伟强,陈鸿.骨盆骨折CT扫描的临床价值[J].临床骨科杂志,1999,2(1):27-28.[23] 谢胜利,杨红梅.螺旋CT三维重建遮盖技术在骨盆骨折中的应用[J].实用医技杂志,2004,11(1):26-27.[24] Giannoudis PV, Pape HC. Damage control orthopaedics in unstable pelvic ring injuries. Injury. 2004;35(7):671-677. |
| [1] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [2] | Xu Feng, Kang Hui, Wei Tanjun, Xi Jintao. Biomechanical analysis of different fixation methods of pedicle screws for thoracolumbar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1313-1317. |
| [3] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [4] | Li Dadi, Zhu Liang, Zheng Li, Zhao Fengchao. Correlation of total knee arthroplasty efficacy with satisfaction and personality characteristics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1346-1350. |
| [5] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [6] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [7] | Yao Rubin, Wang Shiyong, Yang Kaishun. Minimally invasive transforaminal lumbar interbody fusion for treatment of single-segment lumbar spinal stenosis improves lumbar-pelvic balance [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1387-1392. |
| [8] | Lü Zhen, Bai Jinzhu. A prospective study on the application of staged lumbar motion chain rehabilitation based on McKenzie’s technique after lumbar percutaneous transforaminal endoscopic discectomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1398-1403. |
| [9] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [10] | Du Xiupeng, Yang Zhaohui. Effect of degree of initial deformity of impacted femoral neck fractures under 65 years of age on femoral neck shortening [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1410-1416. |
| [11] | Zhang Shangpu, Ju Xiaodong, Song Hengyi, Dong Zhi, Wang Chen, Sun Guodong. Arthroscopic suture bridge technique with suture anchor in the treatment of acromioclavicular dislocation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1417-1422. |
| [12] | Zhang Chao, Lü Xin. Heterotopic ossification after acetabular fracture fixation: risk factors, prevention and treatment progress [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1434-1439. |
| [13] | Zhou Jihui, Li Xinzhi, Zhou You, Huang Wei, Chen Wenyao. Multiple problems in the selection of implants for patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1440-1445. |
| [14] | Wang Debin, Bi Zhenggang. Related problems in anatomy mechanics, injury characteristics, fixed repair and three-dimensional technology application for olecranon fracture-dislocations [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1446-1451. |
| [15] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||