Chinese Journal of Tissue Engineering Research ›› 2020, Vol. 24 ›› Issue (29): 4643-4649.doi: 10.3969/j.issn.2095-4344.2814
Previous Articles Next Articles
Platelet-rich plasma plays a protective role in chondrocytes by regulating synovitis
Chen Wei1, Zhang Guoru1, He Jiandong2, Huo Shaochuan3
1Department of Joint Surgery, Third People’s Hospital of Hainan Province, Sanya 572000, Hainan Province, China; 2Department of Joint Surgery, Guangzhou Orthopedic Hospital, Guangzhou 510000, Guangdong Province, China; 3Shenzhen Hospital, Guangzhou University of Chinese Medicine, Shenzhen 518034, Guangdong Province, China
-
Received:2019-09-16Revised:2019-09-18Accepted:2020-02-24Online:2020-10-18Published:2020-09-14 -
Contact:Huo Shaochuan, MD, Attending physician, Shenzhen Hospital, Guangzhou University of Chinese Medicine, Shenzhen 518034, Guangdong Province, China -
About author:Chen Wei, Master, Department of Joint Surgery, Third People’s Hospital of Hainan Province, Sanya 572000, Hainan Province, China -
Supported by:the China Postdoctoral Foundation (General Project), No. 2018M633088
CLC Number:
Cite this article
Chen Wei, Zhang Guoru, He Jiandong, Huo Shaochuan. Platelet-rich plasma plays a protective role in chondrocytes by regulating synovitis[J]. Chinese Journal of Tissue Engineering Research, 2020, 24(29): 4643-4649.
share this article
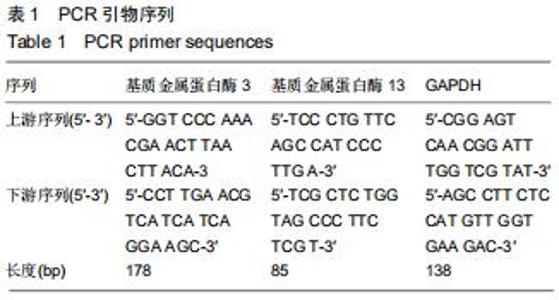
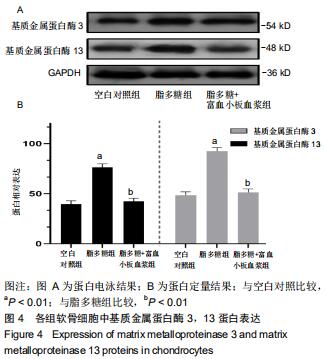
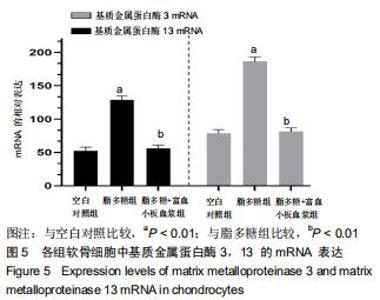
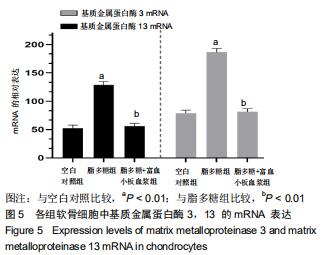
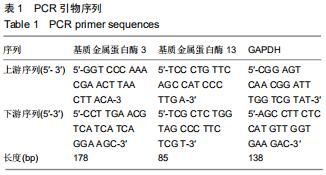
1.4.7 PCR检测基质金属蛋白酶3/13 mRNA的表达水平 Trizol法提取各组软骨细胞中总RNA,Nano Drop 2000测定RNA纯度和浓度。按照反转录试剂盒说明反转录cDNA,反应体系:纯水10 μL,1×Buffer缓冲液10 μL,dNTP Mix 1 mL,上游引物50 pmol,下游引物50 pmol(序列见表1),25 mmol/L MgSO4 2 μL,AMV Reverse Transcriptase 1 μL,Tfl DNA Polymerase 1 μL。95 ℃ Tag酶活化2 min,95 ℃变性15 s,60 ℃退火,循环40次。2-??Ct法计算基质金属蛋白酶3和13的mRNA相对表达量。 "
|
[1] SIT RWS, WU RWK, LAW SW, et al. Intra-articular and extra-articular platelet-rich plasma injections for knee osteoarthritis:A 26-week, single-arm, pilot feasibility study. Knee.2019;160(19)30159-30170.
[2] CROSS M, SMITH E, HOY D, et al.The global burden of hip and knee osteoarthritis: estimates from the global burden of disease2010 study. Ann Rheum Dis. 2014;73(7):1323-1330.
[3] HOY DG, SMITH E, CROSS M, et al. The global burden of musculoskeletal conditions for 2010: an overview of methods. Ann Rheum Dis. 2014;(6):982-989.
[4] BRICCA A, JUHL CB, STEULTJENS M,et al.Impact of exercise on articular cartilage in people at risk of, or with established, knee osteoarthritis: a systematic review of randomised controlled trials.2019;53(15):940-947.
[5] BOSCHETTI F, PERETTI GM. Tensile and compressive properties of healthy and osteoarthritic human articular cartilage. Biorheology. 2008;45(3-4):337-344.
[6] BOUGAULT C1, CUERU L, BARILLER J,et al.Alteration of cartilage mechanical properties in absence of β1 integrins revealed by rheometry and FRAP analyses.J Biomech. 2013; 46(10):1633-1640.
[7] SIEBELT M, VAN DER WINDT AE, GROEN HC,et al. FK506 protects against articular cartilage colla-genous extra-cellular matrix degradation. Osteoarthritis Cartilage. 2014;22(4): 591-600.
[8] SMITH MD. The normal synovium. Open Rheumatol J. 2011;5:100-106.
[9] DELIGNE C, CASULLI S, PIGENET A,et al. Differential expression of interleukin-17 and interleukin -22 in inflamed and non-inflamed synovium from osteoarthritis patients. Osteoarthritis Cartilage.2015;23(11):1843-1852.
[10] SAULNIER N, VIGUIER E, PERRIER-GROULT E,et al. Intra-articular administration of xenogeneic neon-atal Mesenchymal Stromal Cells early aftermeniscal injury down-regulates metalloproteinase gene expression in synovium and preventscartilage degradation in a rabbit model of osteoarth-ritis. Osteoarthritis Cartilage.2015;23(1):122-33.
[11] AYRAL X, PICKERING EH, WOODWORTH TG,et al. Synovitis: a potential predictive factor of structur-ral progression of medial tibiofemoral kneeosteoarthritis-results of a 1 year longitudinal arthroscopic study in 422 patients. Osteoarthritis Cartilage.2005;13(5):361-367.
[12] GILBERTIE JM, LONG JM, SCHUBERT AG, et al.Pooled Platelet-Rich Plasma Lysate Therapy Increases Synoviocyte Proliferation and Hyaluronic Acid Production While Protecting Chondrocytes From Synoviocyte-Derived Inflammatory Mediators.Front Vet Sci. 2018;4(5):150.
[13] DILLON CF, RASCH EK, GU Q, et al. Prevalence of bone osteoarthritis in the United States: arthri-tis data from the Third National Health and Nutrition Examination Survey 1991-94.J Rheu-matol. 2006;33(11):2271-2279.
[14] VOS T, BARBER RM, BELL B, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013.Lancet.2015;386(9995): 743-800.
[15] MURPHY L, HELMICK CG. The impact of osteoarthritis in the United States: a population-health perspective.Am J Nurs. 2012,112(3 Suppl 1):S13-19.
[16] KURTZ S, ONG K, LAU E, et al.Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030.J Bone Joint Surg Am. 2007;89(4):780-785.
[17] LOESER RF, GOLDRING SR, SCANZELLO CR, et al. Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum. 2012;64(6):1697-1707.
[18] LOESER RF, SHANKER G, CARLSON CS, et al.Reduction in the chondrocyte response to insulin-like growth factor 1 in aging and osteoarthritis: studies in a non-human primate model of naturally occurring disease. Arthritis Rheum. 2000; 43(9):2110-2120.
[19] MATHIESSEN A, CONAGHAN PG.Synovitis in osteoarthritis: current understanding with therapeutic implications.Arthritis Res Ther. 2017;19(1):18.
[20] RAHMATI M, MOBASHERI A, MOZAFARI M.Inflammatory mediators in osteoarthritis: A critical review of the state-of-the-art, current prospects, and future challenges. Bone.2016;85:81-90. [21] SARMANOVA A, HALL M, FERNANDES GS, et al. Association between ultrasound-detected synovitis and knee pain: a population-based case-control study with both cross-sectional and follow-up data.Arthritis Res Ther. 2017; 19(1):281.
[22] LAVER L, MAROM N, DNYANESH L, et al. PRP for Degenerative Cartilage Disease: A Systematic Review of Clinical Studies.Cartilage. 2017;8(4):341-364.
[23] JOTANOVIC Z, MIHELIC R, SESTAN B, et al. Role of interleukin-1 inhibitors in osteoarthritis: an evidence-based review.Drugs Aging. 2012;29(5):343-358.
[24] KARDEL R, ULFGREN AK, REINHOLT FP, et al.Inflammatory cell and cytokine patterns in patients with painful clicking and osteoarthritis in the temporomandibular joint.Int J Oral Maxillofac Surg. 2003;32(4):390-396.
[25] KIM JH, JEON J, SHIN M, et al. Regulation of the catabolic cascade in osteoarthritis by the zinc-ZIP8-MTF1 axis.Cell. 2014;156(4):730-743.
[26] PELLETIER JP, KAPOOR M, FAHMI H, et al. Strontium ranelate reduces the progression of experimental dog osteoarthritis by inhibiting the expression of key proteases in cartilage and of IL-1β in the synovium.Ann Rheum Dis. 2013; 72(2):250-257.
[27] TANAKA T, NARAZAKI M, KISHIMOTO T. Therapeutic targeting of the interleukin-6 receptor. Annu Rev Pharmacol Toxicol.2012;52:199–219.
[28] DANDONA P, ALJADA A, BANDYOPADHYAY A. Inflammation: the link between insulin resistance, obesity and diabetes. Trends Immunol.2004;25:4-7.
[29] LEGENDRE F, BOGDANOWICZ P, BOUMEDIENE K, et al. Role of interleukin 6(IL-6)/IL-6R-induced signal tranducers and activators of transcription and mitogen-activated protein kinase/extr-acellular. J Rheumatol.2005;32:1307-1316.
[30] ZHAO B.TNF and Bone Remodeling.Curr Osteoporos Rep. 2017;15(3):126-134.
[31] MAYER U,BENDITZ A,GRÄSSEL S.miR-29b regulates expression of collagens I and III in chondro-genically differentiating BMSC in an osteoarthritic environment.Sci Rep. 2017;7(1):13297.
[32] EYRE D. Collagen of articular cartilage. Arthritis Res.2002; 4(1):30-35.
[33] LEYH M, SEITZ A, DÜRSELEN L,et al.Subchondral bone influences chondrogenic differentiation and collagen production of human bone marrow-derived mesenchymal stem cells and articular chondrocytes.Arthritis Res Ther. 2014;16(5):453.
[34] TAKAHASHI M, FUJIKAWA K, ANGAMMANA R, et al.An in situ hybridization study of MMP-2, -9, -13, -14, TIMP-1, and -2 mRNA in fetal mouse mandibular condylar cartilage as compared with limb bud cartilage.Gene Expr Patterns. 2019; 32:1-11.
[35] XIANG X, ZHOU Y, SUN H,et al. Ivabradine abrogates TNF-α-induced degradation of articular cartilage matrix.Int Immunopharmacol.2019;66:347-353.
[36] AMĂLINEI C, CĂRUNTU ID, BĂLAN RA. Biology of metalloproteinases. Rom J Morphol Embryol. 2007;48(4): 323-334. |
| [1] | Pu Rui, Chen Ziyang, Yuan Lingyan. Characteristics and effects of exosomes from different cell sources in cardioprotection [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(在线): 1-. |
| [2] | Lin Qingfan, Xie Yixin, Chen Wanqing, Ye Zhenzhong, Chen Youfang. Human placenta-derived mesenchymal stem cell conditioned medium can upregulate BeWo cell viability and zonula occludens expression under hypoxia [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(在线): 4970-4975. |
| [3] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [4] | Peng Zhihao, Feng Zongquan, Zou Yonggen, Niu Guoqing, Wu Feng. Relationship of lower limb force line and the progression of lateral compartment arthritis after unicompartmental knee arthroplasty with mobile bearing [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1368-1374. |
| [5] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [6] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [7] | Gu Xia, Zhao Min, Wang Pingyi, Li Yimei, Li Wenhua. Relationship between hypoxia inducible factor 1 alpha and hypoxia signaling pathway [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1284-1289. |
| [8] | Jiang Hongying, Zhu Liang, Yu Xi, Huang Jing, Xiang Xiaona, Lan Zhengyan, He Hongchen. Effect of platelet-rich plasma on pressure ulcers after spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1149-1153. |
| [9] | Wu Xun, Meng Juanhong, Zhang Jianyun, Wang Liang. Concentrated growth factors in the repair of a full-thickness condylar cartilage defect in a rabbit [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1166-1171. |
| [10] | Liu Zhichao, Zhang Fan, Sun Qi, Kang Xiaole, Yuan Qiaomei, Liu Genzhe, Chen Jiang. Morphology and activity of human nucleus pulposus cells under different hydrostatic pressures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1172-1176. |
| [11] | Li Jiacheng, Liang Xuezhen, Liu Jinbao, Xu Bo, Li Gang. Differential mRNA expression profile and competitive endogenous RNA regulatory network in osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1212-1217. |
| [12] | Geng Qiudong, Ge Haiya, Wang Heming, Li Nan. Role and mechanism of Guilu Erxianjiao in treatment of osteoarthritis based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1229-1236. |
| [13] | Liu Xiangxiang, Huang Yunmei, Chen Wenlie, Lin Ruhui, Lu Xiaodong, Li Zuanfang, Xu Yaye, Huang Meiya, Li Xihai. Ultrastructural changes of the white zone cells of the meniscus in a rat model of early osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1237-1242. |
| [14] | Zhang Xiumei, Zhai Yunkai, Zhao Jie, Zhao Meng. Research hotspots of organoid models in recent 10 years: a search in domestic and foreign databases [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1249-1255. |
| [15] | Wang Zhengdong, Huang Na, Chen Jingxian, Zheng Zuobing, Hu Xinyu, Li Mei, Su Xiao, Su Xuesen, Yan Nan. Inhibitory effects of sodium butyrate on microglial activation and expression of inflammatory factors induced by fluorosis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1075-1080. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||