Chinese Journal of Tissue Engineering Research ›› 2013, Vol. 17 ›› Issue (39): 6867-6874.doi: 10.3969/j.issn.2095-4344.2013.39.002
Previous Articles Next Articles
Meloxicam versus indomethacin in the prevention of heterotopic ossification after total hip arthroplasty
Zeng Yi-rong, Jian Lin-yang, Feng Wen-jun, Li Jie, Li Fei-long, He Sheng
- Department of Orthopedics, the First Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine, Guangzhou 510405, Guangdong Province, China
-
Online:2013-09-24Published:2013-09-24 -
Contact:Zeng Yi-rong, Department of Orthopedics, the First Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine, Guangzhou 510405, Guangdong Province, China Zeng6612@139.com -
About author:Zeng Yi-rong☆, M.D., Professor, Department of Orthopedics, the First Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine, Guangzhou 510405, Guangdong Province, China
CLC Number:
Cite this article
share this article
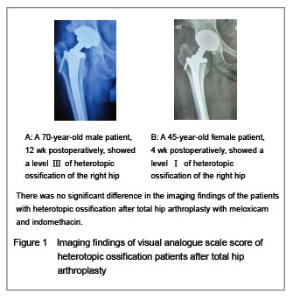
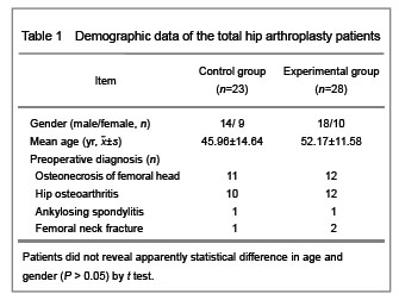
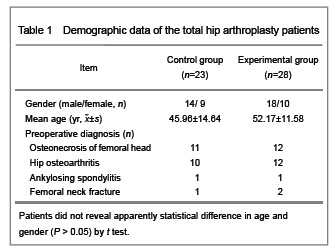
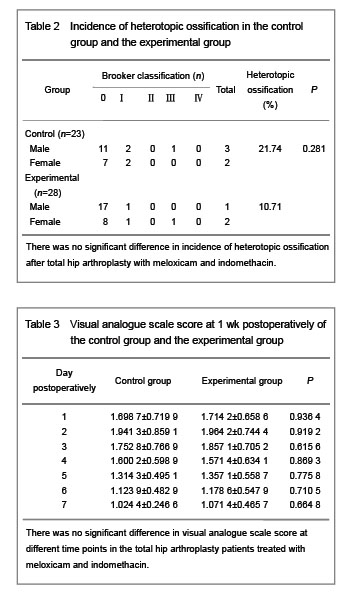
In the control group, there were 23 patients (28 hips), 14 males and nine females, whose ages ranged from 26 years to 70 years, mean age (45.96±11.64) years. Besides, the follow-up time was ranged from 3 months to 9 months, mean (5.5±1.8) months. Among those 23 patients, one hip had synovial inflammation, one hip had ankylosing spondylitis involving double hips, nine hips had osteoarthritis, and 12 patients had avascular necrosis of the femoral head. However, the study group consisted of 28 patients (30 hips), 18 males and 10 females, whose ages ranged from 31 years to 77 years, mean age (52.17±11.58) years. And the follow-up time also ranged from 3 months to 9 months, mean (5.6±2.0) months. The preoperative diagnosis contained 11 cases of hip osteoarthritis, 16 cases of avascular necrosis of the femoral head and one case of ankylosing spondylitis involving double hips. Incidence of heterotopic ossification and visual analogue scale score variation in the total hip arthroplasty patients treated with meloxicam and indomethacin With the respect to the incidence of heterotopic ossification qualified with Brooker classfication, in the control group, 18 cases in level 0, four cases in level Ⅰ, no case in level Ⅱ, one case in level Ⅲ, and no case in level Ⅳ, and the incidence of heterotopic ossification reached 21.74%. While in the experimental group, the 25 cases in level 0, one case in level Ⅰ, one case in level Ⅱ, one case in level Ⅲ, and no case in level Ⅳ, and the incidence rate was 10.71% (Figure 1)."

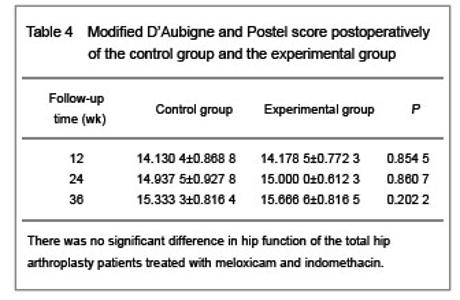
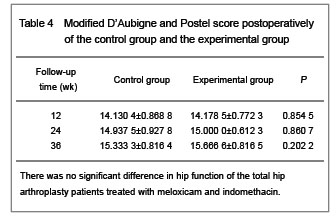
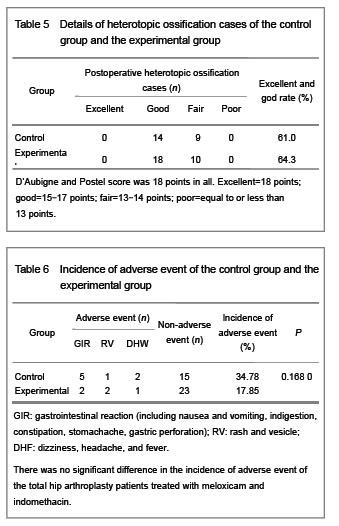
Hip function was assessed with the modified D’Aubigne and Postel score. In the control group, there were no excellent case, 14 good cases, nine fair cases, and no poor case postoperatively. In the experimental group, there were no excellent case, 18 good cases, 10 fair cases, and no poor case respectively. The excellent and good rate was 61% and 64% respectively (P > 0.05, Tables 4 and 5). The main adverse reaction in the control group was gastrointestinal disorder (37.84%), and one patient was not suggested to take the indomethacin sustained- release tablet because of severe irritation reaction. However, one patient suffered rash disease apart from gastrointestinal disorder (17.85%). There was no statistical significance (P > 0.05, Table 6)."
| [1]Riegler HF, Harris CM. Heterotopic bone formation after total hip arthroplasty. Clin Orthop Relat Res. 1976;(117):209-216. [2]Regis D, Sandri A, Sambugaro E. Incidence of heterotopic ossification after surface and conventional total hip arthroplasty: A comparative study using anterolateral approach and indomethacin prophylaxis. Biomed Res Int. 2013;2013:293528. [3]Pavlou G, Salhab M, Murugesan L, et al. Risk factors for heterotopic ossification in primary total hip arthroplasty. Hip Int. 2012;22(1):50-55. [4]Cohn RM, Schwarzkopf R, Jaffe F. Heterotopic ossification after total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2011;40(11):E232-235. [5]Kwapisz A, Koz?owski P, Szemraj J, et al. Correlations between BMP-4 gene expression, heterotopic ossification and function after uncemented total hip replacement. Ortop Traumatol Rehabil. 2013;15(2):117-124. [6]Fang Z, Sun T, Yadav SK. Research progress of bone morphogenetic protein and liability of ossification of posterior longitudinal ligament. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2012;26(10):1255-1258. [7]Katagiri T. BMP signaling and bone formation. Clin Calcium. 2012;22(11):1677-1683. [8]Medici D, Olsen BR. The role of endothelial-mesenchymal transition in heterotopic ossification. J Bone Miner Res. 2012; 27(8):1619-1622. [9]Pakos EE, Pitouli EJ, Tsekeris PG, et al. Prevention of heterotopic ossification in high-risk patients with total hip arthroplasty: the experience of a combined therapeutic protocol. Int Orthop. 2006;30(2):79-83. [10]Cella JP, Salvati EA, Sculco TP. Indomethacin for the prevention of heterotopic ossification following total hip arthroplasty. Effectiveness, contraindications, and adverse effects. J Arthroplasty. 1988;3(3):229-234. [11]Schmidt SA, Kjaersgaard-Andersen P, Pedersen NW, et al. The use of indomethacin to prevent the formation of heterotopic bone after total hip replacement. A randomized, double-blind clinical trial. J Bone Joint Surg Am. 1988; 70(6): 834-838. [12]Vasileiadis GI, Sioutis IC, Mavrogenis AF, et al. COX-2 inhibitors for the prevention of heterotopic ossification after THA. Orthopedics. 2011;34(6):467. [13]Hoff P, Rakow A, Gaber T, et al. Preoperative irradiation for the prevention of heterotopic ossification induces local inflammation in humans. Bone. 2013;55(1):93-101. [14]Pakos EE, Tsekeris PG, Paschos NK, et al. The role of radiation dose in a combined therapeutic protocol for the prevention of heterotopic ossification after total hip replacement. J BUON. 2010;15(1):74-78. [15]Cipriano C, Pill SG, Rosenstock J, et al. Radiation therapy for preventing recurrence of neurogenic heterotopic ossification. Orthopedics. 2009;32(9). [16]Fransen M, Neal B. Withdrawn: Non-steroidal anti-inflammatory drugs for preventing heterotopic bone formation after hip arthroplasty. Cochrane Database Syst Rev. 2013;3:CD001160. [17]Aspenberg P. Avoid cox inhibitors after skeletal surgery! Acta Orthop Scand. 2002;73(5):489-490. [18]Tsailas PG, Babis GC, Nikolopoulos K, et al. The effectiveness of two COX-2 inhibitors in the prophylaxis against heterotopic new bone formation: an experimental study in rabbits. J Surg Res. 2009;151(1):108-114. [19]van der Heide HJ, Spruit M, Slappendel R, et al. Prophylaxis for heterotopic ossification after primary total hip arthroplasty. A cohort study between indomethacin and meloxicam. Acta Orthop Belg. 2004;70(3):240-246. [20]Legenstein R, Bösch P, Ungersböck A. Indomethacin versus meloxicam for prevention of heterotopic ossification after total hip arthroplasty. Arch Orthop Trauma Surg. 2003; 123(2-3):91-94. [21]Barthel T, Baumann B, Nöth U, et al. Prophylaxis of heterotopic ossification after total hip arthroplasty: a prospective randomized study comparing indomethacin and meloxicam. Acta Orthop Scand. 2002;73(6):611-614. [22]Dahners LE, Mullis BH. Effects of nonsteroidal anti-inflammatory drugs on bone formation and soft-tissue healing. J Am Acad Orthop Surg. 2004;12(3): 139-143. [23]Brooker AF, Bowerman JW, Robinson RA, et al. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55(8): 1629-1632. [24]D'aubigne RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36-A(3):451-475. [25]Kocic M, Lazovic M, Mitkovic M, et al. Clinical significance of the heterotopic ossification after total hip arthroplasty. Orthopedics. 2010;33(1):16. [26]Pohl F, Seufert J, Tauscher A, et al. The influence of heterotopic ossification on functional status of hip joint following total hip arthroplasty. Strahlenther Onkol. 2005; 181(8):529-533. [27]Chalmers J, Gray DH, Rush J. Observations on the induction of bone in soft tissues. J Bone Joint Surg Br. 1975;57(1):36-45. [28]Scharstuhl A, Glansbeek HL, van Beuningen HM, et al. Inhibition of endogenous TGF-beta during experimental osteoarthritis prevents osteophyte formation and impairs cartilage repair. J Immunol. 2002;169(1):507-514. [29]Chauveau C, Devedjian JC, Blary MC, et al. Gene expression in human osteoblastic cells from normal and heterotopic ossification. Exp Mol Pathol. 2004;76(1):37-43. [30]Pavlou G, Salhab M, Murugesan L, et al. Risk factors for heterotopic ossification in primary total hip arthroplasty. Hip Int. 2012;22(1):50-55. [31]Okano K, Aoyagi K, Osaki M, et al. Bone mineral density is not related to heterotopic ossification after total hip arthroplasty. Int Orthop. 2012;36(6):1163-1166. [32]Schwarzkopf R, Cohn RM, Skoda EC, et al. The predictive power of preoperative hip range of motion for the development of heterotopic ossification. Orthopedics. 2011;34(3):169. [33]Spinarelli A, Patella V, Petrera M, et al. Heterotopic ossification after total hip arthroplasty: our experience. Musculoskelet Surg. 2011;95(1):1-5. [34]Metzner G, Lindner B, Neumann D, et al. Incidence of anterior intertrochanteric ossifications after total hip arthroplasty—a retrospective long-term follow-up study. Z Orthop Unfall. 2010;148(2):174-179. [35]Gordon A, Southam L, Loughlin J, et al. Variation in the secreted frizzled-related protein-3 gene and risk of osteolysis and heterotopic ossification after total hip arthroplasty. J Orthop Res. 2007;25(12):1665-1670. [36]Nayak KN, Mulliken B, Rorabeck CH, et al. Prevalence of heterotopic ossification in cemented versus noncemented total hip joint replacement in patients with osteoarthrosis: a randomized clinical trial. Can J Surg. 1997;40(5):368-374. [37]Huang WM, Yu XC, Fu ZH, et al. Comparison of incidence of heterotopic ossification in combination versus biotype total hip arthroplasty. Zhongguo Gu yu Guanjie Sunshang Zazhi. 2011;26(10):875-877. [38]Xue D, Zheng Q, Li H, et al. Selective COX-2 inhibitor versus nonselective COX-1 and COX-2 inhibitor in the prevention of heterotopic ossification after total hip arthroplasty: A meta-analysis of randomised trials. Int Orthop. 2011;35(1):3-8. [39]Vavken P, Castellani L, Sculco TP. Prophylaxis of heterotopic ossification of the hip: systematic review and meta-analysis. Clin Orthop Relat Res. 2009;467(12):3283-3289. [40]van der Heide HJ, Koorevaar RT, Schreurs BW, et al. Indomethacin for 3 days is not effective as prophylaxis for heterotopic ossification after primary total hip arthroplasty. J Arthroplasty. 1999;14(7):796-799. [41]Bremen-Kühne R, Stock D, Franke C. Indomethacin—short-term therapy vs. single low dosage radiation for prevention of periarticular ossifications after total hip endoprosthesis. Z Orthop Ihre Grenzgeb. 1997;135(5): 422-429. [42]Fijn R, Koorevaar RT, Brouwers JR. Prevention of heterotopic ossification after total hip replacement with NSAIDs. Pharm World Sci. 2003;25(4):138-145. [43]Bombardier C, Laine L, Reicin A, et al. Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. VIGOR Study Group. N Engl J Med. 2000;343(21):1520-1528. [44]Romanò CL, Duci D, Romanò D, et al. Celecoxib versus indomethacin in the prevention of heterotopic ossification after total hip arthroplasty. J Arthroplasty. 2004;19(1):14-18. [45]Pairet M, van Ryn J, Schierok H, et al. Differential inhibition of cyclooxygenases-1 and -2 by meloxicam and its 4'-isomer. Inflamm Res. 1998;47(6):270-276. [46]Barthel T, Baumann B, Nöth U, et al. Prophylaxis of heterotopic ossification after total hip arthroplasty: a prospective randomized study comparing indomethacin and meloxicam. Acta Orthop Scand. 2002;73(6):611-614. [47]Persson PE, Nilsson OS, Berggren AM. Do non-steroidal anti-inflammatory drugs cause endoprosthetic loosening? A 10-year follow-up of a randomized trial on ibuprofen for prevention of heterotopic ossification after hip arthroplasty. Acta Orthop. 2005;76(6):735-740. [48]Gibbons JJ, Lennon RL, Rose SH, et al. Axillary block of the brachial plexus: "you can't get there from here...". Anesthesiology. 1988;68(2):314-315. |
| [1] | Liu Jianyou, Jia Zhongwei, Niu Jiawei, Cao Xinjie, Zhang Dong, Wei Jie. A new method for measuring the anteversion angle of the femoral neck by constructing the three-dimensional digital model of the femur [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3779-3783. |
| [2] | Shi Junheng, Zhong Degui, Fan Zhirong, Huang Yongquan. Posterior cruciate-retaining versus posterior cruciate-stabilized prostheses for total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(8): 1282-1290. |
| [3] | Hao Liang, Zhang Zhonglin, Wang Baodong, Bi Zhenggang. Intertrochanteric fracture of the femur: improvement of internal fixation device, surgical changes and related disputes [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(18): 2927-2935. |
| [4] | Gong Zhibing, Wu Zhaoke, Zhang Huantang, Xu Zhiqing, Zhuang Zhikun, Zhang Qianjin. Allogeneic cortical bone plate combined with locking plate for Vancouver type B1 and C osteoporotic periprosthetic femoral fractures after hip arthroplasty in older adults [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(12): 1812-1817. |
| [5] | Gu Jianhua, Shi Zhicai . Placement position of artificial vertebral pedicle screws based on the anatomical structure of lumbar nerve roots [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(12): 1829-1833. |
| [6] | Gao Yi, Qu Yu-xing, Zhou Qi, Wang Bin, Zheng Chong, Luo Li-li. Comparison of the stability of direct anterior approach versus posterolateral approach in minimally invasive total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2018, 22(7): 997-1002. |
| [7] | Li Gang, Wang Yue. Short-term outcomes of displaced femoral neck fractures treated with hemiarthroplasty using direct anterior approach [J]. Chinese Journal of Tissue Engineering Research, 2018, 22(7): 1014-1019. |
| [8] | Zhou Chi, He Wei, Liu Yuhao, Guo Hai, Tang Hongyu, Zhang Gangyu, Wang Haibin. Factors related to the fragmentation of ceramic components after fourth-generation ceramic-on-ceramic total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2018, 22(35): 5577-5582. |
| [9] | Zhao Min-chao, Huang Yan, Yuan Wei-jian, Chi Yu-fei, Li Zu-hao, Wu Han. Application of three-dimensional printing metal implants in orthopedics [J]. Chinese Journal of Tissue Engineering Research, 2018, 22(31): 5027-5033. |
| [10] | Yu Qiang, Tian Jing. Application of antibiotic-loaded cement spacers in two-stage revision for periprosthetic joint infection after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2018, 22(31): 5048-5055. |
| [11] | Chen Guan-hong, Qin Lei, Huang Hui, Wang Zhan, Ma Jia-chao, Xu Ying, Zhai Xi-cheng. Intravenous versus articular injection of tranexamic acid for reducing hemorrhage after unilateral total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2018, 22(3): 350-355. |
| [12] | Hu Wen-hao. Efficacy of intravenous versus topical administration of tranexanmic acid in primary total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2018, 22(3): 356-361. |
| [13] | Xu Jun, Xie Lin. Artificial ankle arthroplasty versus ankle joint fusion for traumatic ankle arthritis: efficacy and safety [J]. Chinese Journal of Tissue Engineering Research, 2018, 22(3): 368-373. |
| [14] | Wang Gang, Li Xin-ying, Zhang Shu-quan, Li Ya-jun. Stress relaxation mechanics characteristics of femoral prosthesis after simulating hip replacement [J]. Chinese Journal of Tissue Engineering Research, 2018, 22(3): 385-391. |
| [15] | Zhang Lei, Lian Kai, Peng Hao, Chen Sen. Tibial anteroposterior axis measured by CT scan in optimizing tibial prosthesis rotation during total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2018, 22(3): 426-431. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||