Chinese Journal of Tissue Engineering Research ›› 2013, Vol. 17 ›› Issue (17): 3132-3139.doi: 10.3969/j.issn.2095-4344.2013.17.013
Previous Articles Next Articles
Systematic review on non-cement prosthesis and bone cement prosthesis in total knee arthroplasty
Chen Yue-ping1, Chen Liang1, Gao Hui1, Luo Dong-fang1, Yin Qing-shui2
- 1 Department of Orthopedics, Affiliated Ruikang Hospital of Guangxi University of Chinese Medicine, Nanning 530011, Guangxi Zhuang Autonomous Region, China
2 Department of Orthopedics, General Hospital of Guangzhou Military Command of PLA, Guangzhou 510010, Guangdong Province, China
-
Received:2012-07-27Revised:2012-10-15Online:2013-04-23Published:2013-04-23 -
Contact:Chen Liang, Master, Attending physician, Department of Orthopedics, Affiliated Ruikang Hospital of Guangxi University of Chinese Medicine, Nanning 530011, Guangxi Zhuang Autonomous Region, China chenliang266@126.com -
About author:Chen Yue-ping★, Master, Chief physician, Department of Orthopedics, Affiliated Ruikang Hospital of Guangxi University of Chinese Medicine, Nanning 530011, Guangxi Zhuang Autonomous Region, China chenyueping007@126.com
CLC Number:
Cite this article
Chen Yue-ping, Chen Liang, Gao Hui, Luo Dong-fang, Yin Qing-shui. Systematic review on non-cement prosthesis and bone cement prosthesis in total knee arthroplasty[J]. Chinese Journal of Tissue Engineering Research, 2013, 17(17): 3132-3139.
share this article
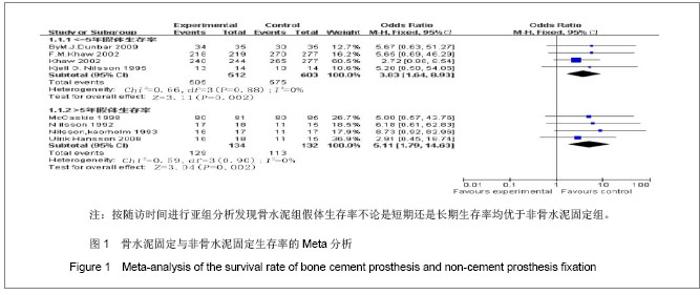
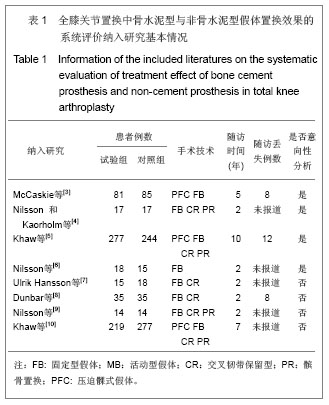
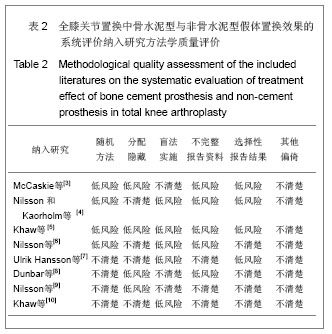
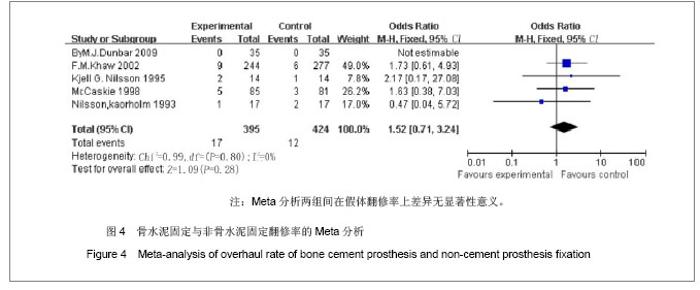
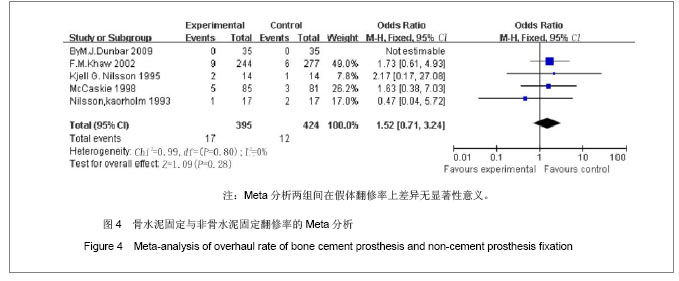
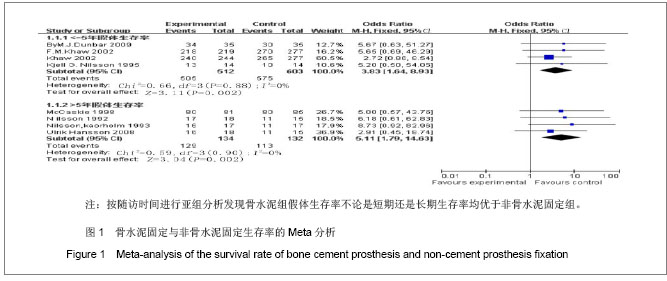
2.4 Meta分析结果 2.4.1 骨水泥型假体与非骨水泥型假体置换后生存率的比较 假体生存率的Meta分析结果:4个研究比较了置换后≤5年随访时的膝关节生存率,4个研究比较了置换后大于5年的膝关节生存率[2-9],置换后≤5年的膝关节生存率,无统计学异质性(P=0.88,I2=0%),运用固定效应模型,组间比较差异有显著性意义(OR=3.38,95%CI 1.64-8.93,P=0.002),说明置换后≤5年骨水泥组生存率高。置换后大于5年患者中的膝关节生存率,无统计学异质性(P=0.90,I2=0%),运用固定效应模型,组间比较差异有显著性意义(OR=5.11,95%CI 1.79-14.63,P=0.002),说明置换后大于5年患者中骨水泥假体组生存率高。见图1。按随访时间进行亚组分析发现骨水泥组假体生存率不论是短期还是长期生存率均优于非骨水泥固定组,分析其中原因,可能是非骨水泥假体主要用于年龄偏轻的患者,年轻人活动量大,活动要求高,磨损相对快,因此生存率低。另外,也可能与观察性研究中容易出现发表偏倚有关。"
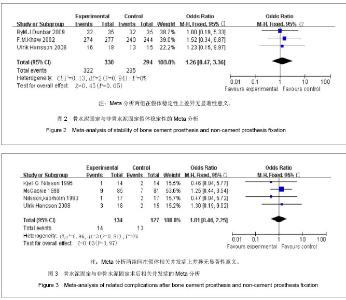
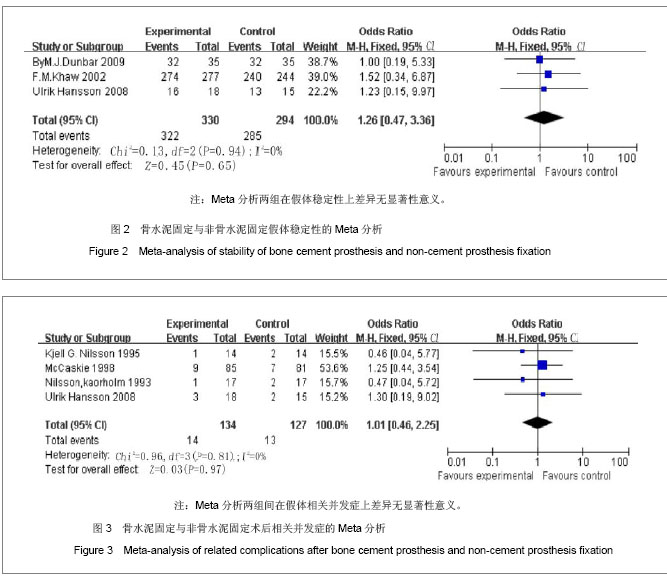
2.4.2 骨水泥型假体与非骨水泥型假体术后稳定性的比较 3个研究在不同随访时间比较了置换后假体稳定性[6-7,9],无统计学异质性(P=0.94,I2=0%),采用固定效应模型,两组间在假体稳定性上无统计学差异(OR=1.26,95%CI 0.47-3.36,P=0.65)。见图2。骨水泥组可以获得早期的稳固固定,Dunbar等[8]认为,骨水泥型固定组的假体松动多发生在置换后6个月内,如果6月内没有松动则可以获得稳定的固定。但随访发现,骨水泥型仍然在以后几年中出现了松动和溶解现象乃至翻修,提示还与其他因素(如手术方式等)有关。非骨水泥固定中假体和骨组织之间的间隙较大,两者间的纤维组织较多,不利于假体与骨组织之间紧密接触和骨组织长入。此外,非骨水泥组假体引起的应力分布不均导致骨吸收大于骨生成引起骨溶解发生增多。 2.4.3 骨水泥型假体与非骨水泥型假体术后相关并发症的比较 4个研究在不同随访时间比较了术后假体相关的并发症[2-3,6,8],无统计学异质性(P=0.81,I2=0%),采用固定效应模型,两组间在假体相关并发症上差异无显著性意义(OR=1.01,95%CI 0.46-2.25,P=0.97)。见图3。深静脉血栓形成是置换后最严重的并发症之一,Ulrik Hansson等[7]文献报道中,年龄超过55岁的女性患者,有吸烟及糖尿病,冠心病的更易术后发生,如术后未进行任何形式的机械性或药物预防,总发病率高达40%-88%。"
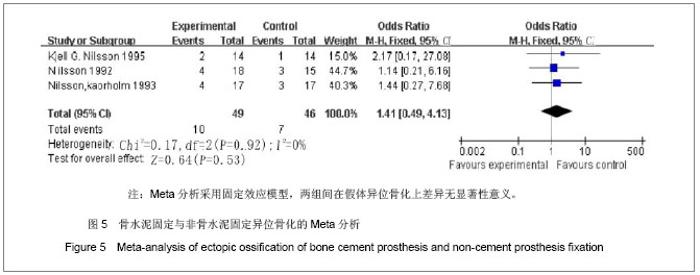
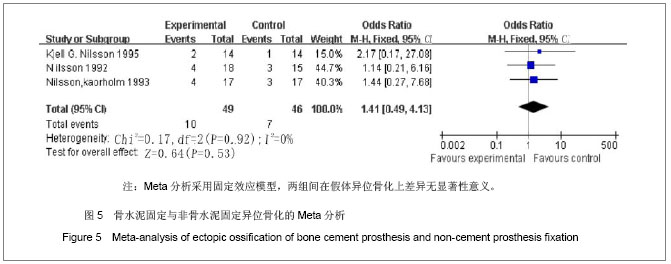
在文献评价研究中,发现假体失败发生翻修的主要原因是假体松动,尤其是胫骨假体的松动。Khaw等[10]报道29例返修病例中,有18例是因为假体无菌性松动,其中有13例是因为胫骨假体无菌性松动,胫骨假体松动发生率达95.6%。Dunbar等[8]报道其返修原因中最常见原因也是假体无菌性松动,但他们研究的患者人群相对集中于年轻人。Khaw等[5]报道14例非骨水泥假体翻修病例中有3例是因为假体无菌性松动,12例骨水泥返修中有1例是假体松动。除了假体松动之外,假体返修的另一个常见原因是假体感染。McCaskie等[3]报道的29例返修病例中有5例是因为假体感染,平均发生时间是术后46 个月。Nilsson等[4]报道14例非骨水泥假体返修病例中有1例感染,12例骨水泥翻修中有5例感染。除本文纳入的研究外,很多作者也有类似报道。 2.4.5 骨水泥型假体与非骨水泥型假体术后异位骨化的比较 3个研究在不同随访时间比较了术后相关的并发症[3,5,8],无统计学异质性(P=0.92,I2=0%),采用固定效应模型,两组间在假体异位骨化上差异无显著性意义(OR=1.41,95%CI 0.49-4.13,P=0.53)。见图5。本系统评价结果显示异位骨化发生率两组之间没有明显差异。异位骨化发生与手术的操作和术中的损伤情况等因素有关。不同的固定方式可能出现骨水泥碎屑落入肌肉或者骨水泥的化学效应等因素引起的异位骨化。说明仍然需要更多的大样本高质量的随机对照试验来对此提出更强有力的证据。"
| [1] Felson DT, Lawrence RC, Dieppe PA,et al. Osteoarthritis: newinsights. Part 1: the disease and its risk factors. Ann Intern Med.2000;133:635-646.[2] Pagani CH, Böhle C, Potthast W, et al. BruggemannShort-termeffects of a dedicated knee orthosis on knee adduction moment,pain,and function in patients with osteoarthritis. Arch Phys MedRehabil.2010;91:1936-1941.[3] Mccaskie AW, Deehan DJ, GreenTP, et al Randomised, prospect ivestudy com paring cemented and cementless total knee rep lacement: results of press-fit condylar total knee rep lacem ent at f ive years.Bone Joint Surg Br.1998;6: 971- 975.[4] Nilsson KG, Karrholm J.Increased varusvalgus tilting of screw fixated knee p rostheses Stereorad iographic study of uncemented versus cementedtib ial compon ents JA rthroplas ty.1993;5:529-540.[5] Khaw FM, Kirk LM, Morris RW, et al. Arandomised, controlled trial of cemented versus cementless press fitcondylar tota knee replacement Ten yearsurvival an alysis.Bone Joint Surg Br.2002;5:658- 666.[6] Nilsson KG, Bjornebrink J, HietalaSO,et al. Scintimetry aftertotal knee arthroplasty Prospect iveyear study of 18 cases of arthrosisand 15 cases of rh eum atoid arthrit is.Acta Orthop Scand.1992;2:159-165.[7] Ulrik Hansson, Leif Ryd, Sören Toksvig-Larsen, et al. A randomised RSA study of Peri-Apatite™ HA coating of a total knee prosthesis. Knee. 2008;15(3):211-216. [8] Dunbar MJ, Wilson DA, Hennigar AW,et al. Fixation of a Trabecular Metal Knee Arthroplasty Component A Prospective Randomized Study.JBJS.2009;,91-A,1578-1586.[9] Nilsson KG, Kärrholm J, Linder L,et al.Femoral Component Migration in Total Knee Arthroplasty: Randomized Study Comparing Cemented and Uncemented Fixation of the Miller-Galante I Design. J Orthop Res.1995;13347-356[10] Khaw FM, Kirk LM, Morris RW, et al. A randomised, controlled trial of cemented versus cementless press-fit condylar total knee replacement. J Bone Joint Surg [Br] 2002;84-B:658-66.[11] Bertsch C, Holz U, Konrad G, et al.[Early clinical outcome after navigated total knee arthroplasty. Comparison with conventional implantation in TKA: a controlled and prospective analysis.Orthopade.2007;36:739-745.[12] Skwara A, Figiel J, Knott T, et al.Primary stability of tibial components in TKA: in vitro comparison of two cementing techniques. Knee Surg Sports Traumatol Arthrosc. 2009;17: 1199-1205[13] Phillips AM, Goddard NJ, Tomlinson JE.Current techniques in total knee replacement: results of a national survey. Ann R Coll Surg Engl.1996;78: 515-520.[14] Ola E Dahl.Cardiorespiratory and vascular dysfunction related tomajor reconstructive orthopedic surgery Acta Orthop scand.1997;68(6):607-614.[15] Clarke MT, Green JS, Harper WM, et al. Cement as a risk factor for deep-vein thrombosis. Comparison of cemented TKR,uncemented TKR and cemented THR. J Bone Joint Surg Br.1998;80:611-613.[16] Sorrells RB, Murphy JA, Sheridan KC, et al.The effect of varus and valgus deformity on results of cementless mobile bearing TKA. Knee. 2007;14:284-288.[17] Whiteside LA, Viganò R.. Vigano Young and heavy patients with a cementless TKA doas well as older and lightweight patients.Clin Orthop Relat Res.2007;464:93-98.[18] Toksvig-Larsen S, Ryd L, Lindstrand A. Early Inducible Displacement of Tibial Components in Total Knee Prostheses Inserted with and without Cement. A Randomized Study with Roentgen Stereophotogrammetric Analysis. J Bone Joint Surg.1998;80-A: 83-89.[19] Gao F, Henricson A, Nilsson KG. NilssonCemented versus uncemented fixation of the femoral component of the NexGen CR total knee replacement in patients younger than 60 years: a prospective randomised controlled RSA study. Knee.2009; 16:200-206.[20] Callaghan JJ, Liu SS. Cementless tibial fixation in TKA: a secondcoming. Orthopedics. 2010;33:655.[21] Naudie DD, Ammeen D J, Engh GA, et al Wear and os teolysis aroundtotal knee arth rop lasty.J Am Acad Orthop Surg.2007;1: 53- 64.[22] Guyatt G,Oxman AD,Akl EA,et al.GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol.2011;64(4):383-394.[23] Schrøder HM, Kristensen PW, Petersen MB,et al.Patient survival after total knee arthroplasty. 5-year data in 926 patients. Acta Orthop Scand.1998;69:35-38. |
| [1] | Chen Zehua, Ye Xiangling, Chen Weijian, Du Jianping, Liu Wengang, Xu Xuemeng. Effect of pronated foot posture on proprioception and postural stability based on foot posture index [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1324-1328. |
| [2] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [3] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [4] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [5] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [6] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [7] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [8] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [9] | Yuan Jiawei, Zhang Haitao, Jie Ke, Cao Houran, Zeng Yirong. Underlying targets and mechanism of Taohong Siwu Decoction in prosthetic joint infection on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1428-1433. |
| [10] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [11] | Xu Yulin, Shen Shi, Zhuo Naiqiang, Yang Huilin, Yang Chao, Li Yang, Zhao Heng, Zhao Lu. Biomechanical comparison of three different plate fixation methods for acetabular posterior column fractures in standing and sitting positions [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 826-830. |
| [12] | Wang Jiangna, Zheng Huifen, Sun Wei. Changes in dynamic stability, motor coordination and joint mechanics of the lower extremity during stair descent and performing phone task [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 837-843. |
| [13] | Zhao Zhongyi, Li Yongzhen, Chen Feng, Ji Aiyu. Comparison of total knee arthroplasty and unicompartmental knee arthroplasty in treatment of traumatic osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 854-859. |
| [14] | Liu Shaohua, Zhou Guanming, Chen Xicong, Xiao Keming, Cai Jian, Liu Xiaofang. Influence of anterior cruciate ligament defect on the mid-term outcome of fixed-bearing unicompartmental knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 860-865. |
| [15] | Zhang Nianjun, Chen Ru. Analgesic effect of cocktail therapy combined with femoral nerve block on total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 866-872. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||