Chinese Journal of Tissue Engineering Research ›› 2013, Vol. 17 ›› Issue (17): 3081-3088.doi: 10.3969/j.issn.2095-4344.2013.17.006
Previous Articles Next Articles
Pedicle screw fixation augmented with bone cement benefits osteoporosis patients
Yue Wen-feng1, Xia Hong2, Wang Jian-hua2
- 1 Postgraduates School of Southern Medical University, Guangzhou 510515, Guangdong Province, China 2 Department of Spine Surgery, Orthopedic Hospital, Guangzhou General Hospital of Guangzhou Military Command of Chinese PLA, Guangzhou 510010, Guangdong Province, China
-
Received:2012-11-01Revised:2012-11-21Online:2013-04-23Published:2013-04-23 -
Contact:Xia Hong, M.D., Chief physician, Department of Spine Surgery, Orthopedic Hospital, Guangzhou General Hospital of Guangzhou Military Command of Chinese PLA, Guangzhou 510010, Guangdong Province, China gzxiahong@hotmail.com -
About author:Yue Wen-feng★, Studying for master’s degree, Physician, Postgraduates School of Southern Medical University, Guangzhou 510515, Guangdong Province, China ywf8201050@163.com
CLC Number:
Cite this article
Yue Wen-feng, Xia Hong, Wang Jian-hua. Pedicle screw fixation augmented with bone cement benefits osteoporosis patients[J]. Chinese Journal of Tissue Engineering Research, 2013, 17(17): 3081-3088.
share this article

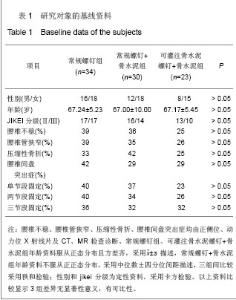
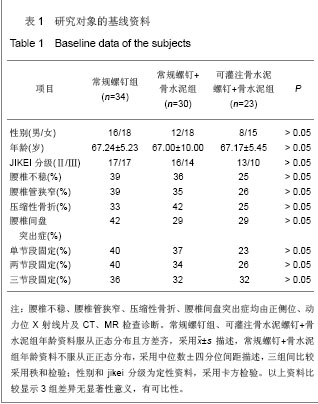
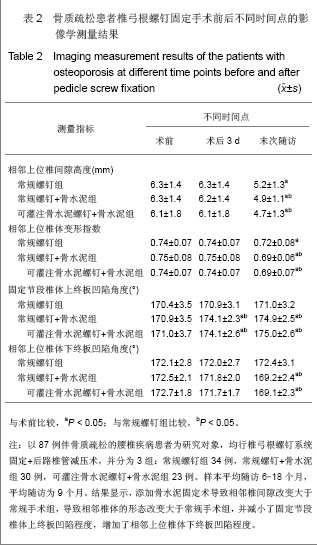
2.6 椎体终板凹陷角度测量结果 见表2。 常规螺钉+骨水泥组和可灌注骨水泥螺钉+骨水泥组组内术后3天和末次随访的固定节段椎体上终板凹陷角度均较术前明显增大(P < 0.05),常规螺钉+骨水泥组和可灌注骨水泥螺钉+骨水泥组组内末次随访的相邻上位椎体下终板凹陷角度均较术前明显减小(P < 0.05),常规螺钉组术前术后终板凹陷角度均无明显变化(P > 0.05)。常规螺钉+骨水泥组、可灌注骨水泥螺钉+骨水泥组2组末次随访的固定节段椎体上终板凹陷角度大于常规螺钉组(P < 0.05),常规螺钉+骨水泥组、可灌注骨水泥螺钉+骨水泥组2组末次随访的相邻上位椎体下终板凹陷角度小于常规螺钉组(P < 0.05),常规螺钉+骨水泥组和可灌注骨水泥螺钉+骨水泥组组间差异无显著意义。表明添加骨水泥固定术后减小了固定节段椎体上终板凹陷程度,增加了相邻上位椎体下终板凹陷程度。 2.7 固定节段Cobb角测量结果 常规螺钉组、常规螺钉+骨水泥组、可灌注骨水泥螺钉+骨水泥组末次随访与术后3 d的Cobb角度的变化值分别为(5.5±1.6) °,(2.1± 0.9)°,(2.3±0.9) °。常规螺钉+骨水泥组、可灌注骨水泥螺钉+骨水泥组2组末次随访与术后3 d Cobb角度的变化值均小于常规螺钉组(P < 0.05),常规螺钉+骨水泥组和可灌注骨水泥螺钉+骨水泥组组间差异无显著性意义(P > 0.05)。 2.8 手术及不良反应 常规螺钉组、常规螺钉+骨水泥组、可灌注骨水泥螺钉+骨水泥组平均手术时间分别为288,292,296 min,平均术中失血量分别为575,561,540 mL,单椎体平均骨水泥用量分别为0,3.4,3.8 mL,平均住院时间分别为18,22,21 d。 所有患者均未出现骨水泥渗漏、放热效应引起的神经功能损伤、毒性反应等严重并发症,末次随访时均达到骨性融合。"
| [1] Anderson GF, Hussey PS. Population aging: a comparison among industrialized countries. Health Aff(Millwood). 2000; 19(3):19l-203.[2] Reitman CA, Nguyen L, Fogel GR. Biomechanical evaluation of relationship of screw pullout strength, insertional torque, and bone mineral density in the cervical spine. J Spinal Disord Tech. 2004;17(4):306-311.[3] Halvorson TL, Kelley LA, Thomas KA, et al. Effects of bone mineral density on pedicle screw fixation. Spine (Phila Pa 1976). 1994;19(21):2415-2420.[4] Weinstein JN, Spratt KF, Spengler D, et al. Spinal pedicle fixation: reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine (Phila Pa 1976). 1988;13(9):1012-1018.[5] Polly DW Jr, Orchowski JR, Ellenbogen RG. Revision pedicle screws. Bigger, longer shims--what is best? Spine (Phila Pa 1976). 1998;23(12):1374-1379.[6] Fan SC, Jin DD, Zhang ZM, et al. Zhongguo Jizhu Jisui Zazhi. 2010;20(9):741-744.[7] Wu YG, Shi ZC, Zhang Y, et al. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2010;14(42):7951-7954.吴云刚,石志才,张晔,等.骨水泥强化椎体提高椎弓根螺钉置入后的稳定性[J].中国组织工程研究与临床康复,2010,14(42): 7951-7954.[8] Zhu QA, Li JY, Zhao WD, et al. Zhonghua Guke Zazhi. 2000; 20(5):283-286.朱青安,李鉴轶,赵卫东,等.聚甲基丙烯酸甲酯强化和修复椎弓根螺钉的生物力学研究[J].中华骨科杂志,2000,20(5):283-286.[9] Ibiwoye MO, Powell KA, Grabiner MD, et al. Bone mass is preserved in a critical-sized osteotomy by low energy pulsed electromagnetic fields as quantitated by in vivo micro-computed tomography. J Orthop Res. 2004;22(5): 1086-1093.[10] Fan SC, Liu SX, Deng YX, et al. Zhongguo Xiufu Chongjian Waike Zazhi. 2004;18(3):168-170.樊仕才,刘世学,邓月兴,等.强化骨质疏松椎弓根螺钉对脊柱稳定性影响的生物力学研究[J].中国修复重建外科杂志,2004,18(3): 168-170.[11] Shono Y, Kaneda K, Abumi K, et al. Stability of posterior spinal instrumentation and its effects on adjacent motion segments in the lumbosacral spine. Spine (Phila Pa 1976). 1998;23(14):1550-1558.[12] Weinhoffer SL, Guyer RD, Herbert M, et al. Intradiscal pressure measurements above an instrumented fusion. A cadaveric study. Spine (Phila Pa 1976). 1995;20(5): 526-531.[13] Miyakoshi N, Abe E, Shimada Y, et al. Outcome of one-level posterior lumbar interbody fusion for spondylolisthesis and postoperative intervertebral disc degeneration adjacent to the fusion. Spine (Phila Pa 1976). 2000;25(14):1837-1842.[14] Lee CK, Langrana NA. Lumbosacral spinal fusion. A biomechanical study. Spine (Phila Pa 1976). 1984;9(6): 574-581.[15] Boucher M, Bhandari M, Kwok D. Health-related quality of life after short segment instrumentation of lumbar burst fractures. J Spinal Disord. 2001;14(5):417-426.[16] Baroud G, Nemes J, Heini P, el al. Load shift of the intervertebral disc after a vertebroplasty:a finite-element study. Eur Spine J. 2003;12(4):421-426.[17] Polikeit A, Nolte LP, Ferguson SJ. The effect of cement augmentation on the load transfer in an osteoporotic functional spinal unit: finite-element analysis. Spine (Phila Pa 1976). 2003;28(10):991-996.[18] Fairbank JC, Pynsent PB. The Oswestry disability index. Spine. 2000;25:2940-2952.[19] Liu Z, Qiu Y. Zhongguo Jizhu Jisui Zazhi. 2008;18:550-553.刘臻,邱勇.Oswestry功能障碍指数在腰痛患者中的国际化应用现状[J].中国脊柱脊髓杂志,2008,18:550-553.[20] Liu Q, Ma C, Wu SL, et al. Zhongguo Kangfu Yixue Zazhi. 2010;25(3):228-231.刘绮,马超,伍少玲,等.Oswestry功能障碍指数评定慢性腰痛患者的效度分析[J].中国康复医学杂志,2010,25(3):228-231.[21] Dabbs VM, Dabbs LG. Correlation between disc height narrowing and low-back pain. Spine (Phila Pa 1976). 1990; 15(12):1366-1369.[22] Chen ZQ, Chen QX. Zhongguo Jizhu Jisui Zazhi. 2003;13(7): 398-401.陈之青,陈其昕.腰椎间盘退变时椎体的形态变化及其临床意义[J].中国脊柱脊髓杂志,2003,13(7):398-401.[23] Evans SF, Nicholson PH, Haddaway MJ, et al. Vertebral morphometry in women aged 50-81 years. Bone Miner. 1993; 21(1):29-40.[24] Miao S, Sha GZ, Wang YD, et al. Zhongguo Gushang. 2008; 21(6):414-417.苗胜,沙广钊,王永东,等.不同程度退变的软骨终板的影像学变化及其临床意义[J].中国骨伤,2008,21(6):414-417.[25] Ryniewicz AM, Skrzat J, Ryniewicz A, et al. Geometry of the articular facets of the lateral atlanto-axial joints in the case of occipitalization. Folia Morphol (Warsz). 2010;69(3):147-153.[26] Becker R, Gatscher S, Sure U, et al. The punctate midline myelotomy concept for visceral cancer pain control--case report and review of the literature. Acta Neurochir Suppl. 2002; 79:77-78.[27] Zencica P, Chaloupka R, Hladíková J, et al. Adjacent segment degeneration after lumbosacral fusion in spondylolisthesis: a retrospective radiological and clinical analysis. Acta Chir Orthop Traumatol Cech. 2010;77(2):124-130.[28] Sempere AP, Mola S, Martin-Medina P, et al. Response to Immunotherapy in CLIPPERS: Clinical, MRI, and MRS Follow-Up. J Neuroimaging. 2011.[29] Zhang GA, Chen JT, Wang LX, et al. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2008;12(22): 4225-4228.张亘瑷,陈建庭,王灵秀,等.定向灌注椎弓根螺钉的生物力学分析[J].中国组织工程研究与临床康复,2008,12(22):4225-4228.[30] Nauta HJ, Soukup VM, Fabian RH, et al. Punctate midline myelotomy for the relief of visceral cancer pain. J Neurosurg. 2000;92(2 Suppl):125-130.[31] Becker R, Sure U, Bertalanffy H. Punctate midline myelotomy. A new approach in the management of visceral pain. Acta Neurochir (Wien). 1999;141(8):881-883.[32] van der Houwen EB, Baron P, Veldhuizen AG, et al. Geometry of the intervertebral volume and vertebral endplates of the human spine. Ann Biomed Eng. 2010;38(1):33-40.[33] Mahato NK. Dorsal iliac dimensions in elderly females: anatomical considerations in two bolt iliac foundation construct. Surg Radiol Anat. 2012;34(2):145-149. [34] He X, Liang A, Gao W, et al. The relationship between concave angle of vertebral endplate and lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2012;37(17): E1068-1073.[35] Erasmus MA, Turner PV, Nykamp SG, et al. Brain and skull lesions resulting from use of percussive bolt, cervical dislocation by stretching, cervical dislocation by crushing and blunt trauma in turkeys. Vet Rec. 2010;167(22):850-858.[36] Tan J, Wang MP, Wan WP, et al. Zhongguo Linchuang Jiepouxue Zazhi. 1997;15(1):59-62.谭军,王鸣鹏,万卫平,等.正常人腰椎椎体解剖结构的QCT研究及其生物力学意义[J].中国临床解剖学杂志,1997,15(1):59-62.[37] Cao J, Shen Y, Yang D, et al. Contrastive analysis of neck axial symptoms after Bryan cervical disc arthroplasty or traditional anterior cervical discectomy and fusion. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2008;22(10):1200-1204. |
| [1] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [2] | Tang Hui, Yao Zhihao, Luo Daowen, Peng Shuanglin, Yang Shuanglin, Wang Lang, Xiao Jingang. High fat and high sugar diet combined with streptozotocin to establish a rat model of type 2 diabetic osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1207-1211. |
| [3] | Li Zhongfeng, Chen Minghai, Fan Yinuo, Wei Qiushi, He Wei, Chen Zhenqiu. Mechanism of Yougui Yin for steroid-induced femoral head necrosis based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1256-1263. |
| [4] | Yuan Jun, Yang Jiafu. Hemostatic effect of topical tranexamic acid infiltration in cementless total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 873-877. |
| [5] | Hou Guangyuan, Zhang Jixue, Zhang Zhijun, Meng Xianghui, Duan Wen, Gao Weilu. Bone cement pedicle screw fixation and fusion in the treatment of degenerative spinal disease with osteoporosis: one-year follow-up [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 878-883. |
| [6] | Li Shibin, Lai Yu, Zhou Yi, Liao Jianzhao, Zhang Xiaoyun, Zhang Xuan. Pathogenesis of hormonal osteonecrosis of the femoral head and the target effect of related signaling pathways [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 935-941. |
| [7] | Xiao Fangjun, Chen Shudong, Luan Jiyao, Hou Yu, He Kun, Lin Dingkun. An insight into the mechanism of Salvia miltiorrhiza intervention on osteoporosis based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 772-778. |
| [8] | Liu Bo, Chen Xianghe, Yang Kang, Yu Huilin, Lu Pengcheng. Mechanism of DNA methylation in exercise intervention for osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 791-797. |
| [9] | Liu Fei, Cui Yutao, Liu He. Advantages and problems of local antibiotic delivery system in the treatment of osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 614-620. |
| [10] | Zhong Yuanming, Wan Tong, Zhong Xifeng, Wu Zhuotan, He Bingkun, Wu Sixian. Meta-analysis of the efficacy and safety of percutaneous curved vertebroplasty and unilateral pedicle approach percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 456-462. |
| [11] | Nie Shaobo, Li Jiantao, Sun Jien, Zhao Zhe, Zhao Yanpeng, Zhang Licheng, Tang Peifu. Mechanical stability of medial support nail in treatment of severe osteoporotic intertrochanteric fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 329-333. |
| [12] | Feng Guancheng, Fang Jianming, Lü Haoran, Zhang Dongsheng, Wei Jiadong, Yu Bingbing. How does bone cement dispersion affect the early outcome of percutaneous vertebroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3450-3457. |
| [13] | Liu Chang, Li Datong, Liu Yuan, Kong Lingbo, Guo Rui, Yang Lixue, Hao Dingjun, He Baorong. Poor efficacy after vertebral augmentation surgery of acute symptomatic thoracolumbar osteoporotic compression fracture: relationship with bone cement, bone mineral density, and adjacent fractures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3510-3516. |
| [14] | Cai Qunbin, Yang Lijuan, Li Qiumin, Chen Xinmin, Zheng Liqin, Huang Peizhen, Lin Ziling, Jiang Ziwei . Feasibility of internal fixation removal of intertrochanteric fractures in elderly patients based on fracture mechanics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3313-3318. |
| [15] | Zhao Hongshun, A Jiancuo, Wang Deyuan, Xu Zhihua, Gao Shunhong. Factors affecting the height of early intervertebral space after lumbar interbody fusion via lateral approach [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3332-3336. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||