Chinese Journal of Tissue Engineering Research ›› 2021, Vol. 25 ›› Issue (30): 4851-4856.doi: 10.12307/2021.273
Previous Articles Next Articles
Locking plate fixation combined with different bone grafts for Neer 3- and 4-part fractures of proximal humerus in the elderly
Liu Wenjie1, Yu Lijuan1, Xu Bin2
- 1Shanxi Medical University, Taiyuan 030001, Shanxi Province, China; 2Department of Orthopedics, The First Affiliated Hospital of Shanxi Medical University, Taiyuan 030001, Shanxi Province, China
-
Received:2020-12-02Revised:2020-12-05Accepted:2021-01-23Online:2021-10-28Published:2021-07-29 -
Contact:Xu Bin, Chief physician, Master’s supervisor, Department of Orthopedics, The First Affiliated Hospital of Shanxi Medical University, Taiyuan 030001, Shanxi Province, China -
About author:Liu Wenjie, Master candidate, Shanxi Medical University, Taiyuan 030001, Shanxi Province, China
CLC Number:
Cite this article
Liu Wenjie, Yu Lijuan, Xu Bin. Locking plate fixation combined with different bone grafts for Neer 3- and 4-part fractures of proximal humerus in the elderly[J]. Chinese Journal of Tissue Engineering Research, 2021, 25(30): 4851-4856.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
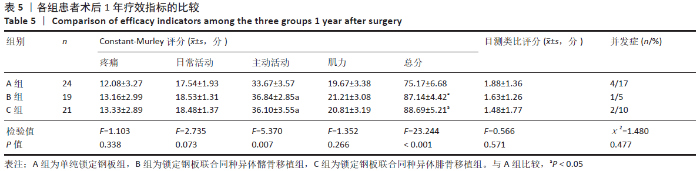
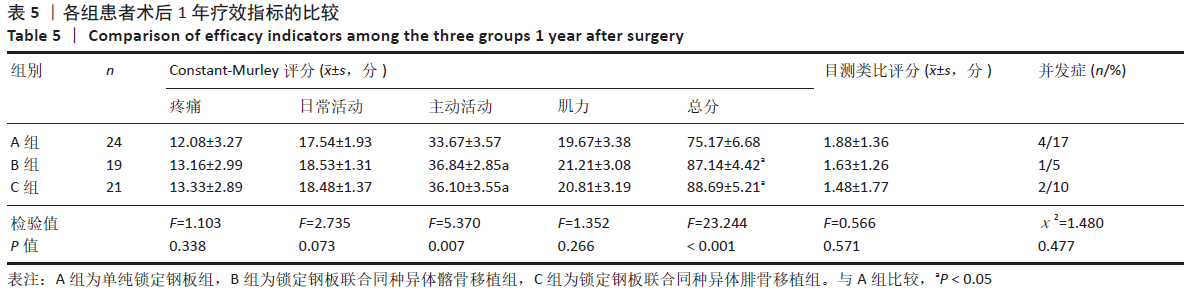
2.6 疗效指标 ①3组患者术后1年时A组Constant-Murley评分总分及主动活动项目得分显著低于B组和C组,差异有显著性意义(P < 0.05),而B、C两组之间差异比较无显著性意义(P > 0.05),其余项目3组得分差异均无显著性意义(P > 0.05);②3组患者在术后1年时目测类比评分比较差异无显著性意义(P > 0.05);③至术后1年时,A组有4例(17%)患者出现并发症,包括螺钉切出1例(4.17%),肱骨头坏死1例(4.17%),关节僵硬2例(8.33%);B组出现1例(5%)肩峰撞击综合征;C组出现2例(10%),其中螺钉切出1例(5%),肱骨头坏死1例(5%);均未出现钢板断裂、骨不连及畸形愈合等严重并发症,3组并发症发生率相比差异无显著性意义(P > 0.05)。见表5。"
| [1] ROUX A, DECROOCQ L, EL BATTI S, et al. Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res. 2012;98(6):715‐719. [2] WARRINER AH, PATKAR NM, CURTIS JR, et al. Which fractures are most attributable to osteoporosis? J Clin Epidemiol. 2011;64(1):46‐53. [3] HOWARD L, BERDUSCO R, MOMOLI F, et al. Open reduction internal fixation vs non-operative management in proximal humerus fractures: a prospective, randomized controlled trial protocol. BMC Musculoskelet Disord. 2018;19(1):299. [4] ANTONIOS T, BAKTI N, NZEAKO O, et al. Outcomes following fixation for proximal humeral fractures. J Clin Orthop Trauma. 2019;10(3):468‐473. [5] 王林祥,王兵,赵滨,等.肱骨近端骨折的治疗进展[J].中国老年学杂志, 2017,37(2):489-491. [6] CAMPOCHIARO G, REBUZZI M, BAUDI P, et al. Complex proximal humerus fractures: Hertel’s criteria reliability to predict head necrosis. Musculoskelet Surg. 2015;99 Suppl 1:S9-S15. [7] JABRAN A, PEACH C, REN L. Biomechanical analysis of plate systems for proximal humerus fractures: a systematic literature review. Biomed Eng Online. 2018;17(1):47. [8] BIERMANN N, PRALL WC, BÖCKER W, et al. Augmentation of plate osteosynthesis for proximal humeral fractures: a systematic review of current biomechanical and clinical studies. Arch Orthop Trauma Surg. 2019;139(8):1075‐1099. [9] LEE SJ, HYUN YS, BAEK SH. Strut Support with Tricortical Iliac Allografts in Unstable Proximal Humerus Fractures: Surgical Indication and New Definition of Poor Medial Column Support. Clin Shoulder Elb. 2019;22(1):29-36. [10] ZHAO L, QI YM, YANG L, et al. Comparison of the Effects of Proximal Humeral Internal Locking System (PHILOS) Alone and PHILOS Combined with Fibular Allograft in the Treatment of Neer Three- or Four-part Proximal Humerus Fractures in the Elderly. Orthop Surg. 2019;11(6):1003‐1012. [11] 张军,庄云强,李东贞,等.锁定钢板结合异体腓骨支撑治疗老年肱骨近端Neer三、四部分骨折[J]. 中华创伤骨科杂志,2018,20(11):946-952. [12] 邢飞,段鑫,刘明,等.同种异体腓骨移植联合锁定钢板治疗肱骨近端骨折的研究进展[J]. 中国修复重建外科杂志,2020,34(2):260-265. [13] NEER CS 2ND. Displaced proximal humeral fractures.I. Classification and evaluation.J Bone Joint Surg(Am). 1970;52(6):1077-1089. [14] CONSTANT CR, MURLEY AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):160-164. [15] HELLER GZ, MANUGUERRA M, CHOW R. How to analyze the Visual Analogue Scale: Myths, truths and clinical relevance. Scand J Pain. 2016;13:67-75. [16] 章宁杰,蒋凌,周祖彬,等.锁定钢板治疗Neer3、4部分肱骨近端骨折的病例对照研究[J].中国骨伤,2014,27(1):38-40. [17] JABRAN A, PEACH C, REN L. Biomechanical analysis of plate systems for proximal humerus fractures: a systematic literature review. Biomed Eng Online. 2018; 17(1):47. [18] STONE MA, NAMDARI S. Surgical Considerations in the Treatment of Osteoporotic Proximal Humerus Fractures. Orthop Clin North Am. 2019;50(2):223-231. [19] CARBONE S, PAPALIA M. The amount of impaction and loss of reduction in osteoporotic proximal humeral fractures after surgical fixation. Osteoporos Int. 2016;27(2):627-633. [20] 李建文,杨永博,万蕾,等.3D技术辅助下半肩置换治疗中老年肱骨近端粉碎性Neer Ⅳ型骨折[J].中国骨伤,2019,32(9):810-814. [21] 王炳,朱诚,王平,等.术后初次颈干角对锁定钢板治疗肱骨近端骨折疗效的影响[J].中国骨伤,2018,31(9):794-798 [22] BARLOW JD, LOGLI AL, STEINMANN SP, et al. Locking plate fixation of proximal humerus fractures in patients older than 60 years continues to be associated with a high complication rate. J Shoulder Elbow Surg. 2020;29(8):1689-1694. [23] ROBINSON CM, STIRLING PHC, GOUDIE EB, et al. Complications and Long-Term Outcomes of Open Reduction and Plate Fixation of Proximal Humeral Fractures. J Bone Joint Surg Am. 2019;101(23):2129-2139. [24] 向成浩,王诗波,明玉祥.内侧柱支撑重建结合锁定钢板内固定治疗老年肱骨近端骨折的临床疗效[J].中国矫形外科杂志,2015,23(4):289-294. [25] LEE SH, HAN SS, YOO BM, et al. Outcomes of locking plate fixation with fibular allograft augmentation for proximal humeral fractures in osteoporotic patients: comparison with locking plate fixation alone. Bone Joint J. 2019;101-B(3): 260-265. [26] CUI X, CHEN H, MA B, et al. Fibular strut allograft influences reduction and outcomes after locking plate fixation of comminuted proximal humeral fractures in elderly patients: a retrospective study. BMC Musculoskelet Disord. 2019;20(1):511. [27] CHEN H, YIN P, WANG S, et al. The Augment of the Stability in Locking Compression Plate with Intramedullary Fibular Allograft for Proximal Humerus Fractures in Elderly People. Biomed Res Int. 2018;2018:3130625. [28] MYERS DM, TRIPLET JJ, WARMOTH PJ, et al. Improved Outcomes Using a Fibular Strut in Proximal Humerus Fracture Fixation. Orthopedics. 2020;43(5):262-268. [29] RUSIMOV L, ZDERIC I, CIRIC D, et al. Does Supplemental Intramedullary Grafting Increase Stability of Plated Proximal Humerus Fractures?. J Orthop Trauma. 2019;33(4):196-202. [30] HSIAO CK, TSAI YJ, YEN CY, et al. Intramedullary cortical bone strut improves the cyclic stability of osteoporotic proximal humeral fractures. BMC Musculoskelet Disord. 2017;18(1):64. [31] TUERXUN M, TUXUN A, ZENG L, et al. Locking Plate Combined With Endosteal Fibular Allograft Augmentation for Medial Column Comminuted Proximal Humeral Fracture. Orthopedics. 2020;43(6):367-372. [32] 杜辉,付勤.同种异体骨移植与自体骨移植修复四肢粉碎性骨折:骨性愈合及骨活性比较[J].中国组织工程研究,2015,19(8):1206-1210. [33] WANG W, YEUNG KWK. Bone grafts and biomaterials substitutes for bone defect repair: A review. Bioact Mater. 2017;2(4):224-247. [34] 王传舜,李豪青,伍凯,等.肱骨近端锁定接骨板结合异体骨植骨治疗外翻嵌插型四部分肱骨近端骨折[J].中华创伤骨科杂志,2013,15(10):909-911. [35] PANCHAL K, JEONG JJ, PARK SE, et al. Clinical and radiological outcomes of unstable proximal humeral fractures treated with a locking plate and fibular strut allograft. Int Orthop. 2016;40(3):569-577. [36] ROBERTS TT, ROSENBAUM AJ. Bone grafts, bone substitutes and orthobiologics: the bridge between basic science and clinical advancements in fracture healing. Organogenesis. 2012;8(4):114-124. |
| [1] | Ouyang Beiping, Ma Xiangyang, Luo Chunshan, Zou Xiaobao, Lu Tingsheng, Chen Qiling. Three-dimensional finite element analysis of a new horizontal screw-screw crosslink in posterior atlantoaxial internal fixation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1320-1324. |
| [2] | Niu Hegang, Yang Kun, Zhang Jingjing, Yan Yizhu, Zhang Yinshun. Design of a new posterior atlas fracture reduction and internal fixation system [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1399-1402. |
| [3] | Wang Menghan, Qi Han, Zhang Yuan, Chen Yanzhi. Three kinds of 3D printed models assisted in treatment of Robinson type II B2 clavicle fracture [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1403-1408. |
| [4] | Yang Cekai, Cai Zhuoyan, Chen Ming, Liu Hao, Weng Rui, Cui Jianchao, Zhang Shuncong, Yao Zhensong. Relationship between degeneration of paraspinal muscle and refractures in postmenopausal women treated by percutaneous vertebroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1414-1419. |
| [5] | Chen Kaijia, Liu Jingyun, Cao Ning, Sun Jianbo, Zhou Yan, Mei Jianguo, Ren Qiang. Application and prospect of tissue engineering in treatment of osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1450-1456. |
| [6] | Dai Yuexing, Zheng Liqin, Wu Minhui, Li Zhihong, Li Shaobin, Zheng Desheng, Lin Ziling. Effect of vessel number on computational fluid dynamics in vascular networks [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1206-1210. |
| [7] | Tong Yibo, Li Minghui. Influencing factors of adjacent vertebral re-fracture in patients with osteoporotic vertebral fractures after percutaneous vertebroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1241-1246. |
| [8] | Wang Qiang, Li Shiyun, Xiong Ying, Li Tiantian. Biomechanical changes of the cervical spine in internal fixation with different anterior cervical interbody fusion systems [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 821-826. |
| [9] | Xue Xiaofeng, Wei Yongkang, Qiao Xiaohong, Du Yuyong, Niu Jianjun, Ren Lixin, Yang Huifeng, Zhang Zhimin, Guo Yuan, Chen Weiyi. Finite element analysis of osteoporosis in proximal femur after cannulated screw fixation for femoral neck fracture [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 862-867. |
| [10] | Huang Peizhen, Dong Hang, Cai Qunbin, Lin Ziling, Huang Feng. Finite element analysis of anterograde and retrograde intramedullary nail for different areas of femoral shaft fractures [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 868-872. |
| [11] | Tan Nengxian, Wu Wenzheng, Zheng Churong, Luo Lieliang, Gu Peng, Ouyang Chongzhi, Zheng Xiaohui. Finite element analysis of different fixation methods of partially threaded cannulated screws for treating vertical femoral neck fractures [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 873-878. |
| [12] | Wang Mingming, Zhang Zhong, Sun Jianhua, Zhao Gang, Song Hua, Yan Huadong, Lyu Bin. Finite element analysis of three different minimally invasive fixation methods for distal tibial fractures with soft tissue injury [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 879-885. |
| [13] | Wu Zhonghan, Wang Jingkun, Li Tao, Xu Xinzhong, Yu Shuisheng, Cheng Li, Tian Dasheng, Tang Jian, Jing Juehua. Proximal femoral nail antirotation for femoral intertrochanteric fractures with lateral wall integrity and lateral wall risk [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 911-916. |
| [14] | Zheng Jiafa, Song Xiufeng, Li Hongzhi, Zhou Jinming, Guan Shengyi, Yu He. Open reduction and internal fixation via the para-Achilles tendon approach for the treatment of posterior malleolus sandwich fractures [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 934-938. |
| [15] | Yu Zhaoyu, Tan Lixin, Sun Kai, Lu Yao, Li Yong. Meta-analysis of cement-augmented pedicle screw for thoracolumbar degenerative diseases with osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 813-820. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||