[1] ELI I, LERNER DP, GHOGAWALA Z. Acute Traumatic Spinal Cord Injury. Neurol Clin. 2021;39(2):471-488.
[2] SZYMONIUK M, LITAK J, SAKWA L, et al. Molecular Mechanisms and Clinical Application of Multipotent Stem Cells for Spinal Cord Injury. Cells. 2022;12(1):120.
[3] PAREDES-ESPINOSA MB, PALUH JL. Human stem cell-derived neurons and neural circuitry therapeutics: Next frontier in spinal cord injury repair. Exp Biol Med (Maywood). 2022;247(23):2142-2151.
[4] LERMAN LO. Cell-based regenerative medicine for renovascular disease. Trends Mol Med. 2021;27(9):882-894.
[5] SHANG Z, WANG M, ZHANG B, et al. Clinical translation of stem cell therapy for spinal cord injury still premature: results from a single-arm meta-analysis based on 62 clinical trials. BMC Med. 2022; 20(1):284.
[6] ZHANG Y, HE Y, DENG R, et al. Multifaceted Characterization of Human Embryonic Stem Cell-Derived Mesenchymal Stem/Stromal Cells Revealed Amelioration of Acute Liver Injury in NOD-SCID Mice. Cell Transplant. 2024;33:9636897231218383.
[7] ANDRZEJEWSKA A, DABROWSKA S, LUKOMSKA B, et al. Mesenchymal Stem Cells for Neurological Disorders. Adv Sci (Weinh). 2021;8(7): 2002944.
[8] MORSY S, MANSOUR MF, ABDO M, et al. Can mobilization of bone marrow stem cells be an alternative regenerative therapy to stem cell injection in a rat model of chronic kidney disease? Physiol Rep. 2022;10(17):e15448.
[9] 程建文,赵劲民,李晓峰,等.芒果苷对缺氧损伤骨髓间充质干细胞的保护作用[J].中国组织工程研究,2014,18(32):5091-5096.
[10] 李晓峰,罗世兴,赵劲民,等.芒果苷对缺氧损伤骨髓间充质干细胞凋亡的保护[J].中国组织工程研究,2013,17(49): 8481-8487.
[11] 李晓峰,赵劲民,苏伟,等.大鼠骨髓间充质干细胞的培养与鉴定[J].中国组织工程研究与临床康复,2011,15(10):1721-1725.
[12] LV B, ZHANG X, YUAN J, et al. Biomaterial-supported MSC transplantation enhances cell-cell communication for spinal cord injury. Stem Cell Res Ther. 2021;12(1):36.
[13] NAM SH, LEE Y, KIM CH, et al. The complex of miRNA2861 and cell-penetrating, dimeric α-helical peptide accelerates the osteogenesis of mesenchymal stem cells. Biomater Res. 2022;26(1):90.
[14] LI B, LIU S, HE Z, et al. The role of zinc finger proteins in the fate determination of mesenchymal stem cells during osteogenic and adipogenic differentiation. Int J Biochem Cell Biol. 2024;167: 106507.
[15] ZUNCHEDDU D, DELLA BELLA E, PETTA D, et al. Effect of glucose depletion and fructose administration during chondrogenic commitment in human bone marrow-derived stem cells. Stem Cell Res Ther. 2022;13(1):533.
[16] LIU W, LUO F, WU H, et al. Noggin Protein can Induce the Differentiation of Rat Bone Marrow Mesenchymal Stem Cells to Neurons and Repair Spinal Cord Injury. Discov Med. 2023;35(179):956-964.
[17] WANG LT, LIU KJ, SYTWU HK, et al. Advances in mesenchymal stem cell therapy for immune and inflammatory diseases: Use of cell-free products and human pluripotent stem cell-derived mesenchymal stem cells. Stem Cells Transl Med. 2021;10(9):1288-1303.
[18] RAGHAVAN S, MALAYAPERUMAL S, MOHAN V, et al. A comparative study on the cellular stressors in mesenchymal stem cells (MSCs) and pancreatic β-cells under hyperglycemic milieu. Mol Cell Biochem. 2021;476(1):457-469.
[19] ZHAO M, LIU S, WANG C, et al. Mesenchymal Stem Cell-Derived Extracellular Vesicles Attenuate Mitochondrial Damage and Inflammation by Stabilizing Mitochondrial DNA. ACS Nano. 2021;15(1): 1519-1538.
[20] TANG LX, WEI B, JIANG LY, et al. Intercellular mitochondrial transfer as a means of revitalizing injured glomerular endothelial cells. World J Stem Cells. 2022;14(9):729-743.
[21] TANG F, TANG J, ZHAO Y, et al. Long-term clinical observation of patients with acute and chronic complete spinal cord injury after transplantation of NeuroRegen scaffold. Sci China Life Sci. 2022;65(5):909-926.
[22] LI M, CHEN H, ZHU M. Mesenchymal stem cells for regenerative medicine in central nervous system. Front Neurosci. 2022;16:1068114.
[23] AFSARTALA Z, HADJIGHASSEM M, SHIRIAN S, et al. Advances in Management of Spinal Cord Injury Using Stem Cell-derived Extracellular Vesicles: A Review Study. Basic Clin Neurosci. 2023;14(4):443-451.
[24] QIN H, ZHAO A. Mesenchymal stem cell therapy for acute respiratory distress syndrome: from basic to clinics. Protein Cell. 2020;11(10): 707-722.
[25] PRAKASH R, FAUZIA E, SIDDIQUI AJ, et al. Oxidative Stress-induced Autophagy Compromises Stem Cell Viability. Stem Cells. 2022;40(5): 468-478.
[26] LI H, XIANG D, GONG C, et al. Naturally derived injectable hydrogels with ROS-scavenging property to protect transplanted stem cell bioactivity for osteoarthritic cartilage repair. Front Bioeng Biotechnol. 2023;10:1109074.
[27] DENG H, CHEN Y, LIU H, et al. Study of the effect of keap1 on oxidative stress in human umbilical cord mesenchymal stem cells. Mol Biol Rep. 2024;51(1):67.
[28] VATNER SF, ZHANG J, OYDANICH M, et al. Healthful aging mediated by inhibition of oxidative stress. Ageing Res Rev. 2020;64:101194.
[29] WENG Z, WANG Y, OUCHI T, et al. Mesenchymal Stem/Stromal Cell Senescence: Hallmarks, Mechanisms, and Combating Strategies. Stem Cells Transl Med. 2022;11(4):356-371.
[30] DENU RA, HEMATTI P. Optimization of oxidative stress for mesenchymal stromal/stem cell engraftment, function and longevity. Free Radic Biol Med. 2021;167:193-200.
[31] HAJAM YA, RANI R, GANIE SY, et al. Oxidative Stress in Human Pathology and Aging: Molecular Mechanisms and Perspectives. Cells. 2022;11(3):552.
[32] AKKI R, SIRACUSA R, CORDARO M, et al. Adaptation to oxidative stress at cellular and tissue level. Arch Physiol Biochem. 2022;128(2): 521-531.
[33] LI X, SU Z, SHEN K, et al. Eugenol-Preconditioned Mesenchymal Stem Cell-Derived Extracellular Vesicles Promote Antioxidant Capacity of Tendon Stem Cells In Vitro and In Vivo. Oxid Med Cell Longev. 2022; 2022:3945195.
[34] XIA C, DAI Z, JIN Y, et al. Emerging Antioxidant Paradigm of Mesenchymal Stem Cell-Derived Exosome Therapy. Front Endocrinol (Lausanne). 2021;12:727272.
[35] HU C, WU Z, LI L. Pre-treatments enhance the therapeutic effects of mesenchymal stem cells in liver diseases. J Cell Mol Med. 2020; 24(1):40-49.
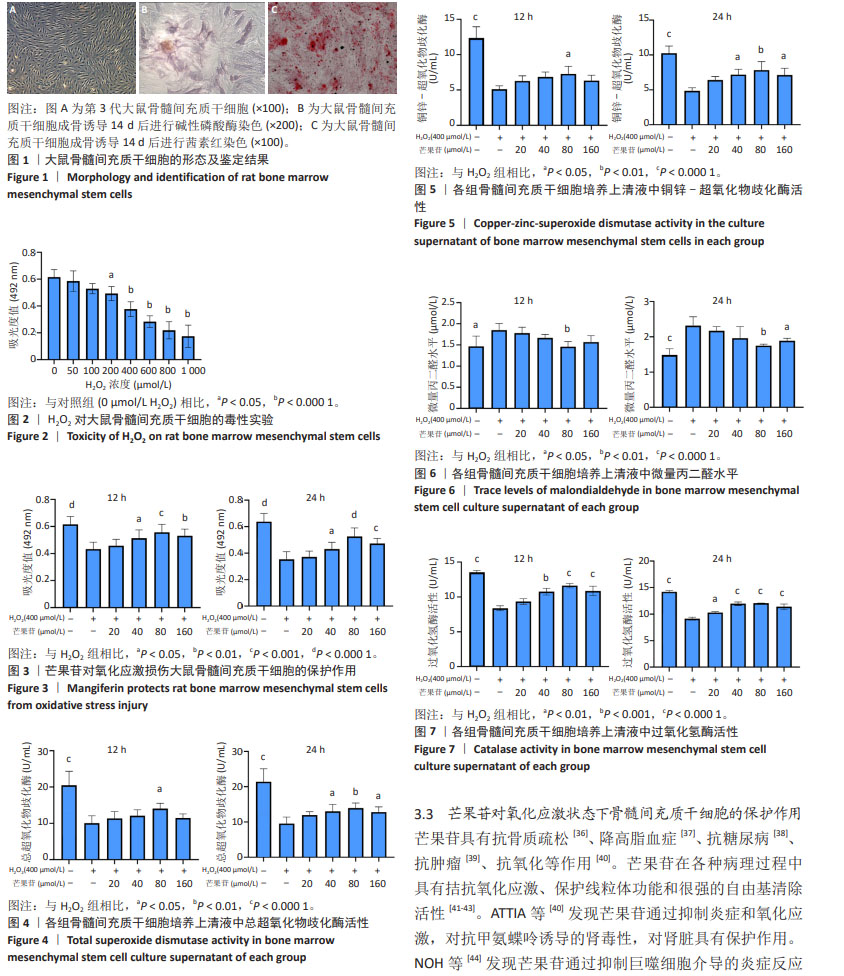
[36] DENG X, LIN B, WANG F, et al. Mangiferin attenuates osteoporosis by inhibiting osteoblastic ferroptosis through Keap1/Nrf2/SLC7A11/GPX4 pathway. Phytomedicine. 2024;124:155282.
[37] MINNITI G, LAURINDO LF, MACHADO NM, et al. Mangifera indica L., By-Products, and Mangiferin on Cardio-Metabolic and Other Health Conditions: A Systematic Review. Life (Basel). 2023;13(12):2270.
[38] YOOPUM S, WONGMANEE N, ROJANAVERAWONG W, et al. Mango (Mangifera indica L.) seed kernel extract suppresses hyperglycemia by modulating pancreatic β cell apoptosis and dysfunction and hepatic glucose metabolism in diabetic rats. Environ Sci Pollut Res Int. 2023;30(59):123286-123308.
[39] RAHMANI AH, ALMATROUDI A, ALLEMAILEM KS, et al. Role of Mangiferin in Management of Cancers through Modulation of Signal Transduction Pathways. Biomedicines. 2023;11(12):3205.
[40] ATTIA SH, ELSHAZLY SM, ABDELAAL MM, et al. Reno-protective effect of mangiferin against methotrexate-induced kidney damage in male rats: PPARγ-mediated antioxidant activity. Saudi Pharm J. 2022;30(9): 1252-1261.
[41] CHANG CC, TSAI KL, CHENG HC, et al. Mangiferin Protects against Angiotensin-II-Enhanced Hypertrophic Markers and Apoptosis in H9c2 Cardiomyocytes. Am J Chin Med. 2023;51(7):1865-1878.
[42] AIN QU, IQBAL MO, KHAN IA, et al. Phytochemical, antioxidant, antipyretic and anti-inflammatory activities of aqueous-methanolic leaf extract of Mangifera indica. Am J Transl Res. 2023;15(7):4533-4543.
[43] WU Y, WANG Y, LONG L, et al. A spatiotemporal release platform based on pH/ROS stimuli-responsive hydrogel in wound repairing. J Control Release. 2022;341:147-165.
[44] NOH JW, LEE HY, LEE BC. Mangiferin Ameliorates Obesity-Associated Inflammation and Autophagy in High-Fat-Diet-Fed Mice: In Silico and In Vivo Approaches. Int J Mol Sci. 2022;23(23):15329.
[45] LUM PT, SEKAR M, SEOW LJ, et al. Neuroprotective potency of mangiferin against 3-nitropropionic acid induced Huntington’s disease-like symptoms in rats: possible antioxidant and anti-inflammatory mechanisms. Front Pharmacol. 2023;14:1189957.
[46] WANG Y, GUO X, FAN X, et al. The protective effect of mangiferin on osteoarthritis: An in vitro and in vivo study. Physiol Res. 2022;71(1): 135-145.
[47] TSATURYAN V, POGHOSYAN A, TOCZYŁOWSKI M, et al. Evaluation of Malondialdehyde Levels, Oxidative Stress and Host-Bacteria Interactions: Escherichia coli and Salmonella Derby. Cells. 2022; 11(19):2989. |