Chinese Journal of Tissue Engineering Research ›› 2015, Vol. 19 ›› Issue (15): 2415-2419.doi: 10.3969/j.issn.2095-4344.2015.15.023
Previous Articles Next Articles
Chronic ankle instability: an analysis based on anatomical structure and biomechanical characteristics of the ankle joint
Su Ying-jun, Tong Xin-yan, Hu Li
- New Church Hospital Affiliated to Guangzhou University of Chinese Medicine, Jiangmen 529100, Guangdong Province, China
-
Revised:2015-03-11Online:2015-04-09Published:2015-04-09 -
About author:Su Ying-jun, Associate chief physician, New Church Hospital Affiliated to Guangzhou University of Chinese Medicine, Jiangmen 529100, Guangdong Province, China
CLC Number:
Cite this article
Su Ying-jun, Tong Xin-yan, Hu Li. Chronic ankle instability: an analysis based on anatomical structure and biomechanical characteristics of the ankle joint[J]. Chinese Journal of Tissue Engineering Research, 2015, 19(15): 2415-2419.
share this article
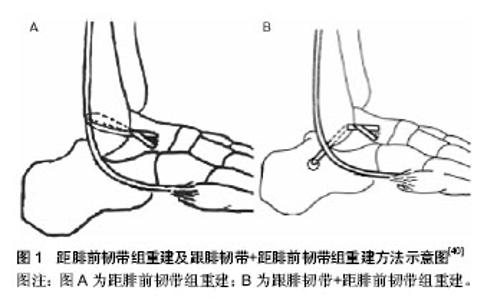
2.1 踝关节解剖学结构 人体踝部由踝关节、距舟关节、距下关节组成。踝关节重要的作用为趾屈41°-43°,背伸26°-27°,总的活动范围在70°。距下关节由距骨下关节面和跟骨上关节面组成,主管足的外翻与内翻。距舟关节由距骨舟骨关节面和舟骨后关节面组成,辅助外翻与内翻功能。踝关节主要由踝外侧韧带、踝内侧韧带、下胫腓联合韧带保持踝关节稳定性。 2.2 踝关节外侧不稳的机制及分级 踝关节韧带损伤有90%为外侧韧带损伤,治疗不及时或处理不当,约30%的患者发展为慢性踝关节外侧不稳[10]。踝关节外侧副韧带主要包括距腓前韧带、距腓后韧带、跟腓韧带,是外踝的主要平衡结构,是维持踝关节稳定的重要组成部分。其中距腓后韧带承担着60%踝关节外侧韧带的稳定作用,跟腓韧带承受着越30%的稳定作用,距腓韧带承担着约10%的稳定作用[11]。 距腓后韧带属于踝关节内侧三角韧带的后束,由外踝窝由距骨外后面直到距骨外侧结节和距跟骨骨面。距腓后韧带具有坚强的外踝附着点,仅有较大的内翻力才能使其撕脱、分离。当足遭受极度内翻或背伸暴力时刻直接导致距腓后韧带断裂跟腓韧带属于踝关节内侧三角韧带的中束,自外踝尖向后下生长直达跟骨外侧中上部。跟腓韧带在足内翻或踝关节背伸时才出现紧张,由于跟腓韧带内翻伤中,应力为最大,更容易发生断裂或撕裂,有时还可能伴有胫腓远侧和前韧带一同撕裂,所以踝关节可能出现胫腓远端分离、半脱位、脱位。 距腓前韧带属于踝关节内侧三角韧带的前束,自外踝前缘向前内方直到距骨颈外侧面,是三束中最薄弱的韧带。但距腓前韧带是防止外翻的重要韧带。当发生足内翻时易损伤深面趾短肌。20%左右的踝关节外侧副韧带损伤若治疗不及时或处理不当,可出现创伤性关节炎或慢性踝关节外侧不稳。踝关节外侧不稳的机制为本体感受器受损[12]。 踝关节外侧副韧带损伤按解剖学可分为:Ⅰ级,距腓前韧带拉长伴有韧带纤维撕裂,临床主要表现为外踝中度肿胀、距腓前韧带有压痛点、踝关节外侧有瘀斑、无关节松弛、完全负重困难、踝关节活动受限;Ⅱ级,距腓前韧带完全撕裂伴有跟腓韧带部分撕裂,临床主要表现为外踝前外侧压缩、局部肿胀、皮下瘀斑出血、活动受限、中度关节松弛等;Ⅲ级,距腓前韧带及跟腓韧带均完全撕裂伴有距腓后韧带和关节囊撕裂,临床主要表现为足部弥漫性肿胀、压痛感强烈、距腓前韧带及跟腓韧带有压痛、皮下瘀斑出血等[13-15]。临床踝关节外侧副韧带超过Ⅰ级,均采用手术治疗方式。 2.3 慢性踝关节不稳的诊断 踝关节损伤未及时有效的诊治、稳定加固踝关节韧带和肌腱损伤或断裂为造成踝关节不稳的主要因素。并且通常踝关节不稳患者有不同程度的踝关节损伤史,慢性踝关节不稳主要通过检测患者肌肉力量(特别是足内翻外翻肌肉力量)、关节活动度、机体感受能力,观察患者站立时或步态时踝关节稳定性[16-17]。临床诊断有以下方法踝关节内翻应力试验、前抽屉试验及超声影像学检测。 2.3.1 踝关节内翻应力试验[18] 患者取坐位,踝趾屈10°-20°,检测人员一只手握住患者内踝上方以固定小腿远端,另一只手缓慢内翻患者足后部,并触诊距骨外侧。超过对侧8°-10°,提示为外侧韧带损伤;内翻15°,提示为距腓前韧带损伤;内翻15°-30°,提示为跟腓韧带和距腓前韧带损伤;内翻超过30°,提示为外侧3条韧带损伤。 2.3.2 踝关节前抽屉试验[19] 前抽屉试验就是距骨相对于胫骨向前移位试验,是由Anderson和Dehne创立,用于检测距腓前韧带松弛情况。在趾屈10°时,前抽屉试验效果最显著。跟腓韧带损伤前抽屉试验结果为阴性,而距腓前韧带断裂前抽屉试验结果为阳性。前抽屉试验在X射线透视机下进行,试验方法:患者取仰卧位或坐位,踝趾屈10°,膝关节屈曲。检测人员一只手握住患者内踝上方以固定患者小腿远端,一只手缓慢向前推患者足跟,使足部距骨于胫骨下方向前移动。另外一种方式为,检测人员一只手将患者足固定于检测床,另一只手于患者小腿远端缓慢向后推胫骨,使胫骨于距骨上方向后移位。在X射线透视机下,前抽屉试验移位超过3 mm,显示为阳性,提示为距腓前韧带损伤。 2.3.3 超声检测 超声可对韧带损伤作为直接的诊断。通常损伤可分为挫伤、部分撕裂、完全撕裂,与病理诊断相关,可进行动态检测。其中对完全撕裂的准确性很高。超声检测对急性损伤的诊断敏感性较好,可诊断出韧带损伤的类型、范围、程度。但超声检测无法直接量化慢性关节Ⅱ度不稳的韧带损伤状态,需要有临床经验丰富的检测按照双侧对比才能诊断[20-21]。 2.3.4 现代影像学检测 核磁共振成像(MRI)是一种现代更为先进的检查技术,用于判定踝关节外侧副韧带损伤的优势显著强于X射线透视。研究表明,MRI检测踝关节外侧副韧带损伤具有85%的敏感性和100%的特异性[22]。但有也有报道显示,MRI检测结果为阴性并有症状的患者,需进行关节镜检测才能进一步确诊。有专家认为,MRI检测与关节镜联合检测可作为踝关节外侧不稳诊断的金标准[23-25]。 2.4 慢性踝关节不稳的治疗 踝关节韧带损伤根据损伤病理学可分为3型[26-28]。Ⅰ型,轻微踝关节韧带损伤;Ⅱ型,不完全踝关节韧带损伤;Ⅲ型,完全破裂踝关节韧带损伤。韧带属于寡血管组织,主要由周围软组织血供,依靠瘢痕组织自愈,一般纤维组织修复需要6周。轻微踝关节韧带损伤可通过合理的保守治疗后自愈,但韧带撕裂严重、未经保守治疗、保守治疗失败的患者常发展成为慢性踝关节不稳定疾病,就应该采用外壳手术治疗或介入治疗方可治愈。临床常见的治疗方法如下。 2.4.1 保守治疗 临床慢性踝关节不稳通常首先尝试保守治疗。患者规范的进行踝关节肌肉及韧带的力量训练、机体感觉训练,能有效的恢复患者正常生活和运动状态。部分肌肉韧带的力量训练可避免实施重建手术。临床保守治疗无统一的规范标准,主要的治疗方法包括物理康复治疗、绷带包扎、矫形器、支持器械、本体感觉训练、腓骨肌力量训练、平衡训练[29]。有许多研究结果证实,康复训练能显著改善患者功能限制及姿势控制,平衡测试又能监测康复训练踝关节功能改善情况[30-31]。其中腓骨肌可为踝关节受到内翻应力时提供关键动力支持,其中腓骨肌的反应时间与支持效率密切相关。通过测定腓骨肌的反应时间可有效的判断本体感觉功能水平,及评定解剖结构修复后踝关节外侧韧带恢复情况。Clark等[21]对踝关节功能性不稳定患者采用数周平衡板摇摆训练,结果显示腓骨长肌肌肉和后胫前肌反应潜伏期明显缩短,踝关节功能积分显著改善。 2.4.2 手术治疗 临床慢性踝关节不稳通过保守治疗失败后,常改为手术治疗。国内慢性踝关节不稳手术治疗处于起步阶段,与国外手术治疗水平有一定的差距[32]。慢性踝关节不稳手术治疗通过修复断裂韧带及关节囊,重建踝关节机械稳定性。踝外侧韧带是慢性踝关节不稳手术治疗的重点部位。需要修复踝外侧的手术指征为机械性不稳定经过3-6个月保守治疗依然无效[33]。主要的临床症状表现为踝关节反复扭伤、踝关节控制无力、慢性疼痛、地面不平时行走困难等。踝关节长期的不稳定和疼痛,严重影响踝关节功能,必须采用手术治疗。 临床手术治疗有多达50种术式可选择[34-36],总体可将其分为3种类型:①使用自体肌腱的非原位肌腱固定术式;有报道中利用趾肌腱重建距腓前韧带和跟腓韧带,取得满意的疗效。②使用部分或全部腓骨肌;该术式机能重建距腓前韧带,还能重建跟腓韧带,同时手术操作简单,疗效确切,但是其利用腓骨附近的短肌腱,会破坏原有肌腱的功能,可造成腓骨短肌腱的力量减弱,不利于踝关节的远期疗效。③原位韧带起止点解剖缝合。原位韧带起止点解剖缝合不需要利用其他腓骨肌腱,不会减弱足外翻力量,不会造成功能区病理反应,可保留距下关节功能,且切口短符合美观要求;但是使用已损伤的组织重建手术难度较大,不容易达到满意。 临床中慢性踝关节不稳手术治疗方法可分为非解剖学重建和受损韧带解剖修复。受损韧带解剖修复是一种直接修复韧带的解剖学手术,广泛用于足踝外科手术,成功率高达90%,被大多数医师及患者所接受。但有报道研究显示,从事体力劳动、运动员、身体肥胖的患者采用受损韧带解剖修复手术的治疗效果欠佳[37]。有研究认为,若韧带过度松弛或者残留韧带不足,临床治疗不建议受损韧带解剖修复[38],而采用非解剖学重建手术。非解剖学重建是一种将肌腱代替受损韧带的手术方法,重建时对患者创伤较大,需以牺牲肌腱为代价。临床常用Watson-Jones及Chrisman-Snook两种术式[39]。Watson-Jones术以重建距腓前韧带为主,能有效的纠正距骨前移或倾斜,改善踝关节稳定性(图1),但由于改变了踝关节解剖力学机制,常引发一些并发症的发生。Chrisman-Snook术选取部分腓骨短肌腱重建跟腓韧带以及距腓前韧带。有研究表明,Chrisman-Snook术后常出现踝关节内翻受限,且该手术创伤面较大,易出现瘢痕、皮肤坏死、触击痛等并发症。"
| [1] 唐康来.注重慢性踝关节不稳的诊断和治疗[J].中国骨伤, 2012, 25(8):623-626. [2] 马信龙. 踝关节骨折的损伤机制[J].中华骨科杂志, 2013,33(4): 429-432. [3] Meacham BP, Granata JD, Berlet GC.Tenodesisreconstruction for chronic ankle instability: graftconsiderations and structures at risk with tunnel placement. Foot Ankle Spec.2012;5(6):378-381. [4] Maffulli N, Spiezia F, Testa V,et al.Free gracilis tendon graft forreconstruction of chronic tears of the Achilles tendon.J Bone Joint Surg Am.2012;94(10):906-910. [5] 范新宇,徐永清,李军等.慢性踝关节前外侧不稳的诊断与治疗[C].第三届全国创伤骨科学术会暨组织修复与重建新技术研讨会论文集,2010:90-94. [6] Hoch MC, Andreatta RD,Mullineaux DR,et al.Two-week joint mobilization intervention improves self-reported function, range of motion, and dynamic balance in those with chronic ankle instability.J Orthop Res.2012;30(11):1798-1804. [7] 陈钺.对两例踝关节损伤病理和病因及伤后处理的探讨[J].福建师大福清分校学报, 2011,31(5):65-69. [8] Cruz-Díaz D,Hita-Contreras F, Lomas-Vega R,et al.Cross-cultural adaptation and validation of the Spanish version of the Cumberland Ankle Instability Tool (CAIT): An instrument to assess unilateral chronic ankle instability.Clin Rheumatol.2013;32(1):91-98. [9] 钟耿耿,徐向阳.踝关节内侧不稳定诊断与治疗[J].国际骨科学杂志,2009,30(2):112-114. [10] Cho BK, Kim YM, Kim DS, et al.Outcomes of the Modified Brostrom Procedure Using Suture Anchors for Chronic Lateral Ankle Instability-A Prospective, Randomized Comparison between Single and Double Suture Anchors.J Foot Ankle Surg.2013;52(1):9-15. [11] Zhao J, Huangfu X.The biomechanical and clinical applicationof using the anterior half of the peroneus longus tendon as anautograft source.Am J Sports Med. 2012;40(3): 662-671. [12] Cruz-Díaz D, Hita-Contreras F, Lomas-Vega R,et al.Cross-cultural adaptation and validation of the Spanish version of the Cumberland Ankle Instability Tool (CAIT): An instrument to assess unilateral chronic ankle instability. Clinical rheumatology.2013;32(1):91-98. [13] 何伟华,黄昌林,李珂等.前抽屉试验侧位片对慢性外踝关节不稳的诊断意义[J].实用医药杂志,2005,22(9):778-780. [14] Maffulli N, Loppini M, Longo UG, et al.Minimally invasivereconstruction of chronic achilles tendon ruptures using theipsilateral free semitendinosus tendon graft and interferencescrew fixation.Am J Sports Med. 2013;41(5): 1100-1107. [15] Zhang L, Li ZY, Liu JS, et al.Clinical results of anatomicalreconstruction of the lateral ligaments for chronic ankleinstability.Zhongguo Gu Shang. 2012;25(11):886-890. [16] Schaefer JL, Sandrey MA.Effects of a 4-week dynamic- balance-training program supplemented with graston instrument-assisted soft-tissue mobilization for chronic ankle instability.J Sport Rehabil. 2012;21(4):313-326. [17] Hubbard TTRA. Quantitative assessment of mechanical laxityin the functional unstable ankle. Med Sci Sports Exerc. 2004;36(5):760-766. [18] Croy T, Saliba SA, Saliba E, et al.Differences in lateral ankle laxity measured via stress ultrasonography in individuals with chronic ankle instability, ankle sprain copers, and healthy individuals.J Orthop Sports Phys Ther. 2012;42(7):593-600. [19] Beazell JR,Grindstaff TL,Sauer LD,et al.Effects of a proximal or distal tibiofibular joint manipulation on ankle range of motion and functional outcomes in individuals with chronic ankle instability.J Orthop Sports Phys Ther. 2012;42(2): 125-134. [20] Santilli V, Frascarelli MA, Paoloni M, et al. Peroneus longusmuscle activation pattern during gait cycle in athletes affectedby functional ankle instability: a surface electromyographicstudy. Am J Sports Med. 2005;33(8): 1183-1187. [21] Clark VM. A 4-week wobble board exercise programmeimproved muscle onset latency and perceived stability inindividuals with a functionally unstable ankle. Physical Therapy Sport.2005;6(4):181-187. [22] 何伟华,原林,黄昌林,等.慢性外踝关节不稳定的影像学诊断[J].解放军医学杂志,2005,30(5):436-438. [23] Caprio A, Oliva F, Treia F, Maffulli N.Reconstruction of theLateral ankle ligaments with allograft in patients with chronicankle instability. Foot Ankle Clin.2006;11:597-605. [24] Hua Y, Chen S, Jin Y, et al. Anatomical reconstruction of thelateral ligaments of the ankle with semitendinosus allograft. Int Orthop.2012;36(10):2027-2031. [25] Pagenstert GI,Hintermann B,Knupp M.Operativemanagement of chronic ankle instability: Plantaris graft. Foot Ankle Clin. 2006; 3:567-583. [26] Krips R,van Dijk CN,Halasi T,et al.Anatomical reconstructionversus tenodesis for the treatment of chronic anterolateralinstability of the ankle joint: a 2- to 10-year follow-up,multicenter study. Knee Surg Sports Traumatol Arthrosc.2000;8(3):173-179. [27] Trevino SG, Davies P, Hecht PJ. Management of acute andchronic injuries of the ankle. Orthop Clin North Am. 1994; 25:1-16. [28] Kitaoka HB, Alexander IJ, Adelaar RS, et al.Clinical systemsfor the ankle-hindfoot, hallux and lesser toes. Foot Ankle.1994;15(7):349-353. [29] Hale SA. The effect of a 4-week comprehensive rehabilitationprogram on postured control and lower extremity function inindividuals with chronic ankle instability. J Orthop Sports PhysTher. 2007;37(6):303-311. [30] Schmidt R, Gergroü H, Friemert B, et al.The peronealreaction time (PRT)--reference data in a healthy samplepopulation. ot Ankle Int.2005 ;26(5):382-386. [31] Konradsen L, Ravn JB. Prolonged peroneal reaction time inankle instability. Int J Sports Med.1991;12(3):290-292. [32] 杨珍,胡亚哲.慢性踝关节不稳的诊断与修复[J].中国组织工程研究,2014,35(9):1434-1440. [33] Ellis SJ, Williams BR, Pavlov H, et al.Results of anatomiclateral ankle ligament reconstruction with tendon allograft .HSS J.2011;7:134-140. [34] Su S. Reinforced Anatomical Reconstruction of the AnteriorTalofibular Ligament in Chronic Anterolateral Instability Usinga Periosteal Flap.Foot and Ankle. 1991; 12(1): 15-18. [35] 徐琦,张立新.改良Brostrom术式治疗慢性踝关节外侧不稳21例疗效分析[J].中国骨与关节损伤杂志,2011,26(2):164-165. [36] 周建刚.改良Chrisman-Snook手术治疗慢性踝关节不稳定[J].现代医药卫生,2005,21(20):2792-2793. [37] 李仙彤. 踝关节慢性不稳定的手术治疗[J].中国伤残医学, 2008, 16(4):19-20. [38] 唐康来.注重慢性踝关节不稳的诊断和治疗[J].中国骨伤, 2012, 25(8):623-626. [39] Lee J,Hamilton G,Ford L,et al.Associated intra-articular ankle pathologies in patients with chronic lateral ankle instability: arthroscopic findings at the time of lateral ankle reconstruction. Foot Ankle Spec.2011;4(5):284-289. [40] 沙勇,唐辉,丁晶,等. 同种异体肌腱解剖重建修复慢性踝关节不稳[J].中国组织工程研究,2014,18(27):4401-4405. |
| [1] | Wang Debin, Bi Zhenggang. Related problems in anatomy mechanics, injury characteristics, fixed repair and three-dimensional technology application for olecranon fracture-dislocations [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1446-1451. |
| [2] | Yi Meizhi, Luo Guanghua, Xiao Yawen, Hu Rong, Chen Xiaolong, Zhao Heng. MRI findings of anatomical variations of the talus [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3888-3893. |
| [3] | Wang Lei, Qi Rong, Li Jia, Qiu Zhixue, Wang Kai, Suo Nanangxiu. Minimally invasive percutaneous plate osteosynthesis and elastic nail system in the treatment of distal tibiofibular fracture in adults [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1864-1868. |
| [4] | Xu Baoyun, Fu Weili. Posterior cruciate ligament injury: diagnosis, treatments and rehabilitation strategies [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(11): 1766-1772. |
| [5] | Bao Chunyu, Yan Mingming. Biomechanical characteristics of ankle joint in volleyball players during stop-jump [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(5): 662-666. |
| [6] | Zou Xiaobao, Ma Xiangyang, Wang Binbin, Yang Haozhi, Ge Su, Chen Yuyue, Zhang Shuang, Ni Ling, Xia Hong, Wu Zenghui. CT measurement of posterior part of atlantoaxial anatomical structures and design of atlantoaxial interlaminar fusion cage [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(36): 5837-5842. |
| [7] | Weng Shiyang, Wu Kai, Lin Jian, Huang Yinjun, Wang Qiugen, Huang Jianhua. Double-strand suture anchor in the treatment of tibiofibular syndesmosis injury [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(33): 5332-5337. |
| [8] | Wang Zhizhou, Zhang Hailong, Chen Jian, Ye Zheng, Yang Yuanqing, Ying Zhengran. Anatomical characteristics of acromioclavicular joint and joint discs [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(33): 5358-5365. |
| [9] | Liu Junyan, Pan Shinong. Anatomical changes and imaging manifestations of childhood developmental dysplasia of the hip [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(30): 4875-4881. |
| [10] | Gong Yusuo, Zhou Jun, Li Shenghua, Zhu Yanguo. Anatomic progress of pubic symphysis and biomechanical characteristics of internal fixation [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(27): 4371-4375. |
| [11] | Li You, Zheng Bengbeng, Wang Jiaming, Ma Yongsheng. Research and application of artificial cervical disc [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(12): 1941-1948. |
| [12] | Fan Zhirong, Peng Jiajie, Zhong Degui, Zhou Lin, Su Haitao, Huang Yongquan, Wu Jianglin, Liang Yihao. Suture anchor combined with open reduction and internal fixation versus open reduction and internal fixation for ankle fracture combined with deltoid ligament injury: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(8): 1307-1312. |
| [13] | Chen Yinghua, Wei Qingjun, Yao Jun. A study of a safe area and angle for harvesting autogenous hamstring tendons for anterior cruciate ligament reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(30): 4822-4827. |
| [14] | Zhang Bin, Li Zhijun, Ning Pengfei, Liu Ying, Cao Li, Zhang Fengying, Li Xiaohe. Finite element analysis of transoral anterior atlantoaxial plate fixation in a teenager [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(28): 4535-4540. |
| [15] | Wang Guixin, He Jinquan. Diagnosis and treatment of deltoid ligament injury of ankle joint [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(20): 3235-3241. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||