Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (7): 1687-1698.doi: 10.12307/2026.060
Previous Articles Next Articles
Differences in metabolism, proliferation, differentiation of adipose-derived mesenchymal stem cells, and differentiation into vascular smooth muscle cells between male and female rats
Wang Qiuhua1, Du Ziwei1, Wang Wenshuang2, Zhao Dongmei1, Zhang Xiaoqing1
- 1School of Basic Medical Sciences, Binzhou Medical University, Department of Human Anatomy and Histoembryology, Joint Laboratory for International Cooperation in Biomaterials and Tissue Regeneration, Yantai 264003, Shandong Province, China; 2Department of Gynecology, Yantai Yuhuanding Hospital, Yantai 264000, Shandong Province, China
-
Received:2025-01-15Revised:2025-05-09Accepted:2025-05-29Online:2026-03-08Published:2025-08-19 -
Contact:Zhang Xiaoqing, MD, Professor, School of Basic Medical Sciences, Binzhou Medical University, Department of Human Anatomy and Histoembryology, Joint Laboratory for International Cooperation in Biomaterials and Tissue Regeneration, Yantai 264003, Shandong Province, China; Zhao Dongmei, MD, Professor, School of Basic Medical Sciences, Binzhou Medical University, Department of Human Anatomy and Histoembryology, Joint Laboratory for International Cooperation in Biomaterials and Tissue Regeneration, Yantai 264003, Shandong Province, China -
About author:Wang Qiuhua, MS, School of Basic Medical Sciences, Binzhou Medical University, Department of Human Anatomy and Histoembryology, Joint Laboratory for International Cooperation in Biomaterials and Tissue Regeneration, Yantai 264003, Shandong Province, China; Du Ziwei, MS, School of Basic Medical Sciences, Binzhou Medical University, Department of Human Anatomy and Histoembryology, Joint Laboratory for International Cooperation in Biomaterials and Tissue Regeneration, Yantai 264003, Shandong Province, China Wang Qiuhua and Du Ziwei contributed equally to this article. -
Supported by:Taishan Scholar Youth Project, No. tsqn202103111 (to ZXQ); Shandong Natural Science Foundation Youth Fund, No. ZR2021QC034 (to ZXQ); Yantai Province-level Talent Matching Fund, No. 1007-10073802 (to ZXQ); Shandong Overseas High-level Talent Workstation Fund, No. 2023119005 (to ZXQ)
CLC Number:
Cite this article
Wang Qiuhua, Du Ziwei, Wang Wenshuang, Zhao Dongmei, Zhang Xiaoqing. Differences in metabolism, proliferation, differentiation of adipose-derived mesenchymal stem cells, and differentiation into vascular smooth muscle cells between male and female rats [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1687-1698.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

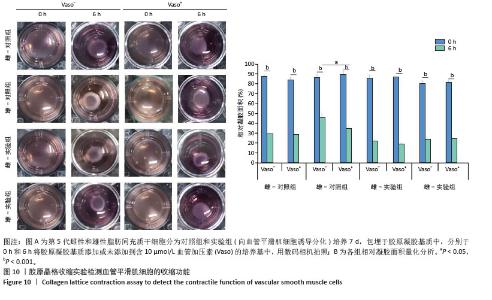
2.1 原代ADSCs的形态 原代培养3 d后,细胞黏附在壁上并开始延伸,细胞形态呈纺锤状,大部分显示成纤维细胞样生长,见图1。 2.2 流式细胞术检测ADSCs表面抗原 第5代ADSCs高表达CD90、CD29,阳性表达率分别为(94.10±0.85)%,(93.80±0.21)%;低表达CD45,阳性表达率为(3.05±0.50)%,见图2。 2.3 雌性和雄性大鼠ADSCs的代谢活性 通过WST-1实验比较雌性和雄性大鼠ADSCs的代谢活性,结果显示与雄性大鼠ADSCs相比,雌性大鼠ADSCs的细胞代谢活性高,见图3。 2.4 雌性和雄性大鼠ADSCs的倍增时间 雌性和雄性大鼠ADSCs的细胞倍增时间分别为(18.047±0.507) h,(18.049±0.428) h,差异无显著性意义(P > 0.05),见图4。 2.5 雌性和雄性大鼠ADSCs集落形成情况 雌性和雄性大鼠ADSCs集落形成率分别为(85.75±2.77)%,(83.01±2.84)%,差异无显著性意义(P > 0.05),见图5。 2.6 雌性和雄性大鼠ADSCs的成脂、成骨、成软骨分化能力 在成脂分化实验中,显微镜下观察到有红色的脂滴形成;在成骨分化实验中,显微镜下观察有深红色的钙结节形成。在成软骨分化实验中,显微镜下观察可见蓝染的软骨球,见图6。"
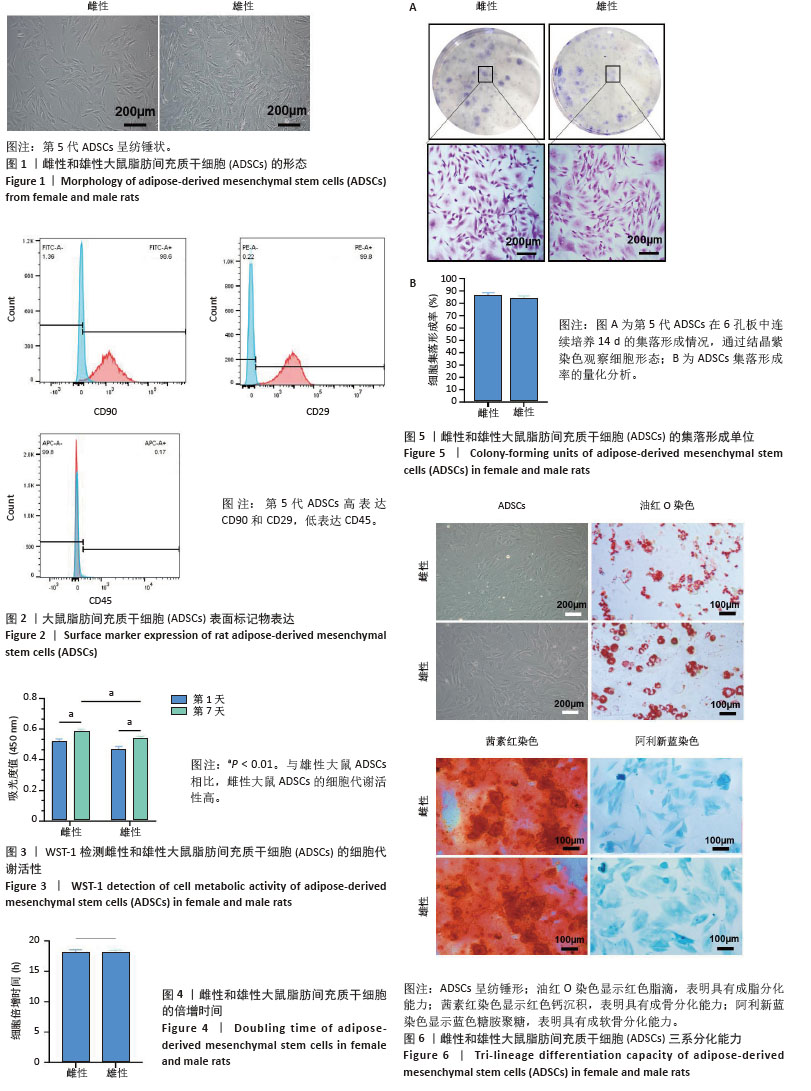

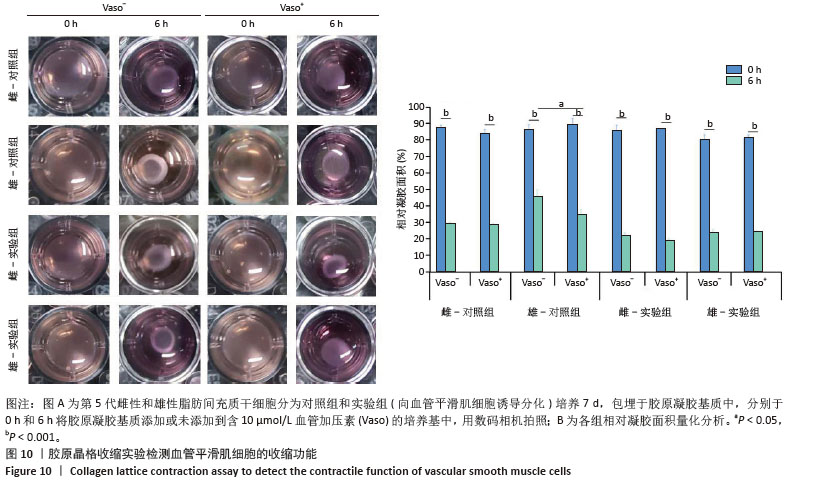
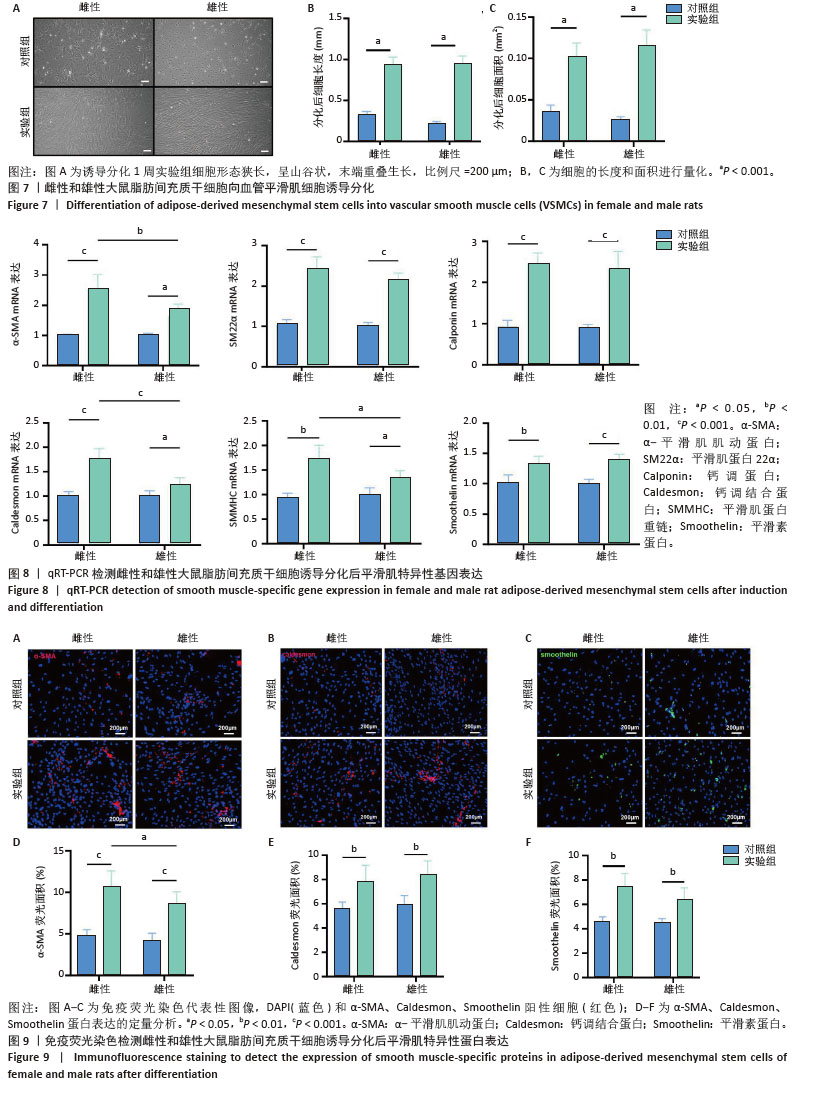
2.7 雌性和雄性大鼠ADSCs向血管平滑肌细胞分化的细胞形态 第5代雌性和雄性大鼠ADSCs诱导分化1周后,细胞形态狭长,以“丘陵和山谷”模式生长,见图7。 2.8 雌性和雄性大鼠ADSCs向血管平滑肌细胞分化后的平滑肌相关基因表达 qRT-PCR检测显示,与对照组相比,实验组平滑肌特异性基因α-SMA、SM22α、Calponin、Caldesmon、SMMHC、Smoothelin表达上调。在实验组中,与雌性大鼠ADSCs相比,雄性大鼠ADSCs α-SMA、Caldesmon、SMMHC表达下调,见图8。 2.9 雌性和雄性大鼠ADSCs向血管平滑肌细胞分化后的平滑肌相关蛋白表达 免疫荧光染色检测显示,与对照组相比,实验组平滑肌特异性蛋白α-SMA、Caldesmon、Smoothelin表达上调。在实验组中,与雌性大鼠ADSCs相比,雄性大鼠ADSCs α-SMA表达下调,见图9。 "
| [1] MCCLELLAN M, BROWN N, CALIFF RM, et al. Call to Action: Urgent Challenges in Cardiovascular Disease: A Presidential Advisory From the American Heart Association. Circulation. 2019;139(9):e44-e54. [2] SMAGUL S, KIM Y, SMAGULOVA A, et al. Biomaterials Loaded with Growth Factors/Cytokines and Stem Cells for Cardiac Tissue Regeneration. Int J Mol Sci. 2020;21(17):5952. [3] MONGUIÓ-TORTAJADA M, PRAT-VIDAL C, MORON-FONT M, et al. Local administration of porcine immunomodulatory, chemotactic and angiogenic extracellular vesicles using engineered cardiac scaffolds for myocardial infarction. Bioact Mater. 2021;6(10):3314-3327. [4] QIN K, WANG F, SIMPSON RML, et al. Hyaluronan promotes the regeneration of vascular smooth muscle with potent contractile function in rapidly biodegradable vascular grafts. Biomaterials. 2020; 257:120226. [5] MI CH, QI XY, ZHOU YW, et al. Advances in medical polyesters for vascular tissue engineering. Discov Nano. 2024;19(1):125. [6] LAU KYC, AMADEI G, ZERNICKA-GOETZ M. Assembly of complete mouse embryo models from embryonic and induced stem cell types in vitro. Nat Protoc. 2023;18(12):3662-3689. [7] ROHRINGER S, GRASL C, EHRMANN K, et al. Biodegradable, Self-Reinforcing Vascular Grafts for In Situ Tissue Engineering Approaches. Adv Healthc Mater. 2023;12(23):e2300520. [8] XIE C, RITCHIE RP, HUANG H, et al. Smooth muscle cell differentiation in vitro: models and underlying molecular mechanisms. Arterioscler Thromb Vasc Biol. 2011;31(7):1485-1494. [9] GU W, HONG X, LE BRAS A, et al. Smooth muscle cells differentiated from mesenchymal stem cells are regulated by microRNAs and suitable for vascular tissue grafts. J Biol Chem. 2018;293(21):8089-8102. [10] LIU M, GOMEZ D. Smooth Muscle Cell Phenotypic Diversity. Arterioscler Thromb Vasc Biol. 2019;39(9):1715-1723. [11] ZHANG J, WANG L, FU W, et al. Smooth muscle cell phenotypic diversity between dissected and unaffected thoracic aortic media. J Cardiovasc Surg (Torino). 2013;54(4):511-521. [12] FRISMANTIENE A, PHILIPPOVA M, ERNE P, et al. Smooth muscle cell-driven vascular diseases and molecular mechanisms of VSMC plasticity. Cell Signal. 2018;52:48-64. [13] NEFF LP, TILLMAN BW, YAZDANI SK, et al. Vascular smooth muscle enhances functionality of tissue-engineered blood vessels in vivo. J Vasc Surg. 2011;53(2):426-434. [14] YIN Z, ZHANG J, SHEN Z, et al. Regulated vascular smooth muscle cell death in vascular diseases. Cell Prolif. 2024;57(11):e13688. [15] SHIMIZU K, SUGIYAMA S, AIKAWA M, et al. Host bone-marrow cells are a source of donor intimal smooth- muscle-like cells in murine aortic transplant arteriopathy. Nat Med. 2001;7(6):738-741. [16] MIZUNO H. The potential for treatment of skeletal muscle disorders with adipose-derived stem cells. Curr Stem Cell Res Ther. 2010;5(2): 133-136. [17] TIAN Z, YU T, LIU J, et al. Introduction to stem cells. Prog Mol Biol Transl Sci. 2023;199:3-32. [18] DE MORREE A, RANDO TA. Regulation of adult stem cell quiescence and its functions in the maintenance of tissue integrity. Nat Rev Mol Cell Biol. 2023;24(5):334-354. [19] LIU B, QU J, ZHANG W, et al. A stem cell aging framework, from mechanisms to interventions. Cell Rep. 2022;41(3):111451. [20] MENS MMJ, GHANBARI M. Cell Cycle Regulation of Stem Cells by MicroRNAs. Stem Cell Rev Rep. 2018;14(3):309-322. [21] PLANAT-BENARD V, SILVESTRE JS, COUSIN B, et al. Plasticity of human adipose lineage cells toward endothelial cells: physiological and therapeutic perspectives. Circulation. 2004; 109(5):656-663. [22] WANG M, LIN S, MEQUANINT K. Electrospun Biodegradable α-Amino Acid-Substituted Poly(organophosphazene) Fiber Mats for Stem Cell Differentiation towards Vascular Smooth Muscle Cells. Polymers (Basel). 2022;14(8):1555. [23] EL-NASEERY NI, ELEWA YHA, EL-BEHERY EI, et al. Human umbilical cord blood-derived mesenchymal stem cells restored hematopoiesis by improving radiation induced bone marrow niche remodeling in rats. Ann Anat. 2023;250:152131. [24] KHORASANI HR, SANCHOULI M, MEHRANI J, et al. Potential of Bone-Marrow-Derived Mesenchymal Stem Cells for Maxillofacial and Periodontal Regeneration: A Narrative Review. Int J Dent. 2021; 2021:4759492. [25] LIEN SC, USAMI S, CHIEN S, et al. Phosphatidylinositol 3-kinase/Akt pathway is involved in transforming growth factor-beta1-induced phenotypic modulation of 10T1/2 cells to smooth muscle cells. Cell Signal. 2006;18(8):1270-1278. [26] IBIKUNLE S, GROSSO D, GERGIS U. The two-step approach to allogeneic hematopoietic stem cell transplantation. Front Immunol. 2023;14:1237782. [27] BURT RK, ALEXANDER T, EBMT AUTOIMMUNE DISEASES WORKING PARTY (ADWP). Hematopoietic stem cell transplantation for multiple sclerosis: no inflammation, no response. Eur J Neurol. 2025;32(1):e16565. [28] MARIOTTINI A, DE MATTEIS E, CENCIONI MT, et al. Haematopoietic Stem Cell Transplantation for the Treatment of Multiple Sclerosis: Recent Advances. Curr Neurol Neurosci Rep. 2023;23(9):507-520. [29] ZHOU R, ZHU L, FU S, et al. Small Diameter Blood Vessels Bioengineered From Human Adipose-derived Stem Cells. Sci Rep. 2016;6:35422. [30] DAVIS JP, SALMON M, POPE NH, et al. Attenuation of aortic aneurysms with stem cells from different genders. J Surg Res. 2015;199(1): 249-258. [31] BARRIGA F, RAMÍREZ P, WIETSTRUCK A, et al. Hematopoietic stem cell transplantation: clinical use and perspectives. Biol Res. 2012;45(3): 307-316. [32] LAROYE C, GAUTHIER M, ANTONOT H, et al. Mesenchymal Stem/Stromal Cell Production Compliant with Good Manufacturing Practice: Comparison between Bone Marrow, the Gold Standard Adult Source, and Wharton’s Jelly, an Extraembryonic Source. J Clin Med. 2019;8(12):2207. [33] DI TRAPANI M, BASSI G, RICCIARDI M, et al. Comparative study of immune regulatory properties of stem cells derived from different tissues. Stem Cells Dev. 2013;22(22):2990-3002. [34] MUNARIN F, KANT RJ, RUPERT CE, et al. Engineered human myocardium with local release of angiogenic proteins improves vascularization and cardiac function in injured rat hearts. Biomaterials. 2020;251:120033. [35] ROY S, SCHMUCK E, RAVAL A. Macrophage Response to Biomaterials in Cardiovascular Applications. Stem Cells. 2021:81-92. doi: 10.1007/978-3-030-77052-5_6 [36] OLINIC M, LAZAR FL, ONEA HL, et al. Peripheral Artery Disease Ultrasound Assessment in Predicting the Severity of Coronary Artery Disease. Life (Basel). 2024;14(3):333. [37] LEE J, GILLILAND TC, DRON J, et al. Integrative Metabolomics Differentiate Coronary Artery Disease, Peripheral Artery Disease, and Venous Thromboembolism Risks. Arterioscler Thromb Vasc Biol. 2024;44(9):2108-2117. [38] ZHANG F, KING MW. Immunomodulation Strategies for the Successful Regeneration of a Tissue-Engineered Vascular Graft. Adv Healthc Mater. 2022;11(12):e2200045. [39] SONG X, FU Y, LI C, et al. Single-cell RNA sequencing atlas of peripheral blood mononuclear cells from subjects with coronary artery disease. Biochim Biophys Acta Mol Cell Res. 2024;1871(1):119593. [40] SONG HG, RUMMA RT, OZAKI CK, et al. Vascular Tissue Engineering: Progress, Challenges, and Clinical Promise. Cell Stem Cell. 2018; 22(3):340-354. [41] SHI J, YANG Y, CHENG A, et al. Metabolism of vascular smooth muscle cells in vascular diseases. Am J Physiol Heart Circ Physiol. 2020;319(3):H613-H631. [42] OWENS GK, KUMAR MS, WAMHOFF BR. Molecular regulation of vascular smooth muscle cell differentiation in development and disease. Physiol Rev. 2004;84(3):767-801. [43] BROZOVICH FV, NICHOLSON CJ, DEGEN CV, et al. Mechanisms of Vascular Smooth Muscle Contraction and the Basis for Pharmacologic Treatment of Smooth Muscle Disorders. Pharmacol Rev. 2016;68(2): 476-532. [44] WANG W, LIU D, LI D, et al. Nanofibrous vascular scaffold prepared from miscible polymer blend with heparin/stromal cell-derived factor-1 alpha for enhancing anticoagulation and endothelialization. Colloids Surf B Biointerfaces. 2019;181:963-972. [45] WANG C, CEN L, YIN S, et al. A small diameter elastic blood vessel wall prepared under pulsatile conditions from polyglycolic acid mesh and smooth muscle cells differentiated from adipose-derived stem cells. Biomaterials. 2010;31(4):621-630. [46] ZHANG X, BATTISTON KG, LABOW RS, et al. Generating favorable growth factor and protease release profiles to enable extracellular matrix accumulation within an in vitro tissue engineering environment. Acta Biomater. 2017;54:81-94. [47] BERNSTEIN SR, KELLEHER C, KHALIL RA. Gender-based research underscores sex differences in biological processes, clinical disorders and pharmacological interventions. Biochem Pharmacol. 2023;215:115737. [48] EDVINSSON JCA, GRUBOR I, MADDAHI A, et al. Male-female comparison of vasomotor effects of circulating hormones in human intracranial arteries. J Headache Pain. 2024;25(1):216. |
| [1] | He Jiale, Huang Xi, Dong Hongfei, Chen Lang, Zhong Fangyu, Li Xianhui. Acellular dermal matrix combined with adipose-derived stem cell exosomes promotes burn wound healing [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1699-1710. |
| [2] | Yuan Weiyuan, Lei Qinhui, Li Xiuqi, Lu Tiezhu, Fu Ziwen, Liang Zhili, Ji Shaoyang, Li Yijia, Ren Yu . Therapeutic effects of adipose-derived mesenchymal stem cells and their exosomes on dexamethasone-induced sarcopenia in mice [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 58-67. |
| [3] | Wan Lingling, Wu Mengying, Zhang Yujiao, Luo Qingqing. Inflammatory factor interferon-gamma affects migration and apoptosis of human vascular smooth muscle cells through pyroptosis pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1422-1428. |
| [4] | Lu Jieming, Li Yajing, Du Peijie, Xu Dongqing. Effects of artificial turf versus natural grass on biomechanical performance of the lower limbs in young females during jump-landing [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1101-1107. |
| [5] | Wen Zixing, Xu Xin, Zhu Shengqun. Correlations between gastrocnemius morphology parameters and physical activity capacity in elderly females under high-frequency ultrasound [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1058-1063. |
| [6] | Xu Fei, Yan Jinqiang, Chai Shoudong. Mechanical stress regulates apoptosis in vascular smooth muscle cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1064-1072. |
| [7] | Wang Kairu, Fu Shizhe, Li Jiahui, Yan Ru, Ma Yuru, Shi Bo, Ye Congyan , Yan Rui, Cong Guangzhi, Jia Shaobin. Spermidine/spermine N1-acetyltransferase 1 participates in vascular smooth muscle cell calcification [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6836-6842. |
| [8] | Dong Youqing, Wei Zixuan, Wu Haiou, Chen Ruixiong, Duan Peng, Chen Nan, Lin Xikai. Biomechanical characteristics of lower limbs in female patients with different types of patellofemoral pain syndrome [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4458-4468. |
| [9] | Chen Jiahui, Dai Xiaoqi, Xu Yangang, Li Yuanchao, Huang Mei, Zhan Yifei, Du Yuxuan, Li Liuqiang, Guo Yaochuan, Bian Jun, Lai Dehui. Isolation, culture and differentiation of human urine-derived stem cells into smooth muscle cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(19): 4076-4082. |
| [10] | Guo Xinfeng, Liang Zhidong, Chen Huiyu, Li Yang. Effects of training modalities and training cycles on visceral and subcutaneous fat in recessively obese individuals [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(11): 2340-2346. |
| [11] | Li Yang, Fu Lili, Yang Jiantang. Adipose mesenchymal stem cell-derived exosome attenuates radiation-induced oral mucositis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(1): 31-37. |
| [12] | Qiu Xiaoyan, Li Bixin, Li Jingdi, Fan Chuiqin, Ma Lian, Wang Hongwu. Differentiation of insulin-producing cells from human umbilical cord mesenchymal stem cells infected by MAFA-PDX1 overexpressed lentivirus [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1000-1006. |
| [13] | Mei Jingyi, Liu Jiang, Xiao Cong, Liu Peng, Zhou Haohao, Lin Zhanyi. Proliferation and metabolic patterns of smooth muscle cells during construction of tissue-engineered blood vessels [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1043-1049. |
| [14] | Wang Tihui, Wang Xu, Wu Jinqing, Chen Jiliang, Wang Xiaolu, Miao Juan. Application of three-dimensional simulated osteotomy of the distal femur in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 905-910. |
| [15] | Wang Xiaopeng, Zhong Rong, Zhong Yan, Lin Feng, Ye Shuxi. Influencing factors of adjacent vertebral refracture in elderly female patients with osteoporotic vertebral compression fracture and construction of a prediction model based on Nomogram [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(36): 5799-5804. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||