Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (24): 5140-5147.doi: 10.12307/2025.728
Previous Articles Next Articles
Mechanism of stachydrine-induced autophagy in improving atherosclerosis in high-fat-fed mice
Yang Jun, Yin Peng, Zheng Zhonghua
- Department of Vascular Surgery, Bijie Hospital, Zhejiang Provincial People’s Hospital, Bijie 551700, Guizhou Province, China
-
Received:2024-06-17Accepted:2024-08-24Online:2025-08-28Published:2025-01-24 -
About author:Yang Jun, Associate chief physician, Department of Vascular Surgery, Bijie Hospital, Zhejiang Provincial People’s Hospital, Bijie 551700, Guizhou Province, China -
Supported by:Guizhou Province Natural Science Basic Research Program, No. 2022JM-580 (to YJ)
CLC Number:
Cite this article
Yang Jun, Yin Peng, Zheng Zhonghua. Mechanism of stachydrine-induced autophagy in improving atherosclerosis in high-fat-fed mice[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5140-5147.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

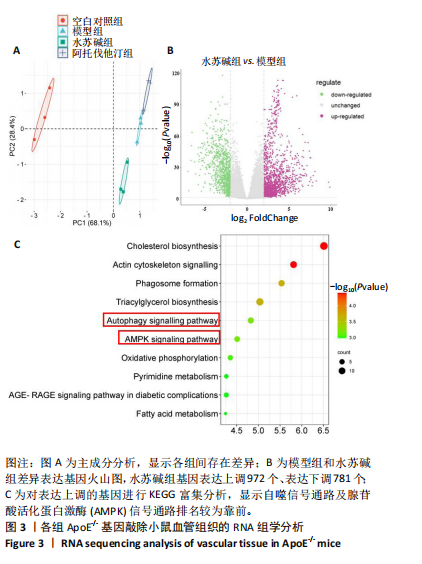
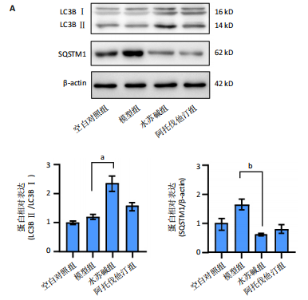
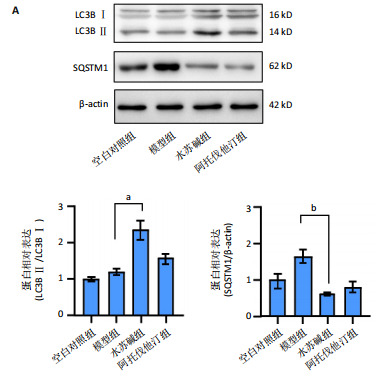
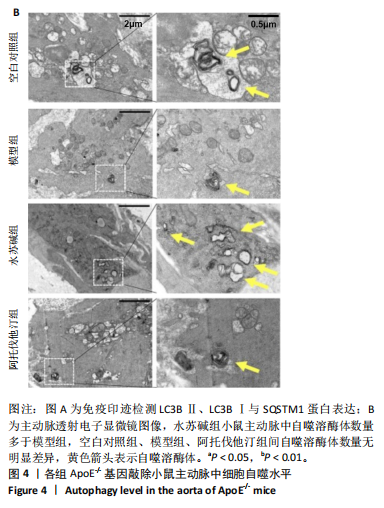
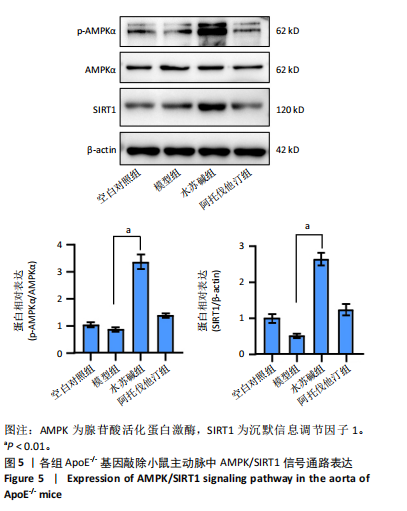
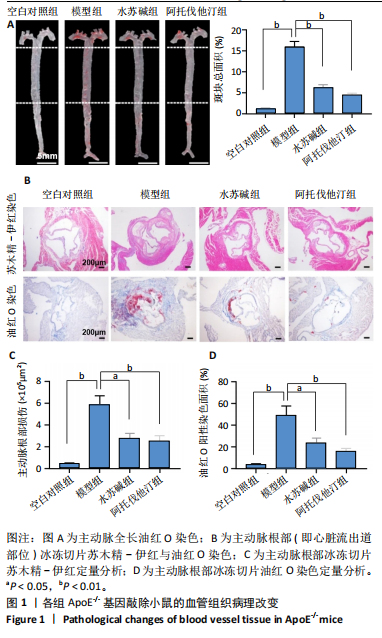
2.1 实验动物数量分析 48只ApoE-/-基因敲除小鼠全部进入结果分析。 2.2 水苏碱减轻动脉粥样硬化小鼠血管组织病理改变 各组ApoE-/-基因敲除小鼠全长主动脉油红O染色,见图1A。与空白对照组相比,模型组小鼠主动脉动脉粥样硬化斑块总面积增多(P < 0.01);与模型组相比,水苏碱组、阿托伐他汀组主动脉动脉粥样硬化斑块总面积减少(P均< 0.01);水苏碱组主动脉动脉粥样硬化斑块总面积与阿托伐他汀组比较差异无显著性意义(P > 0.05)。 各组ApoE-/-基因敲除小鼠主动脉根部苏木精-伊红与油红O染色结果,见图1B。与空白对照组相比,模型组小鼠主动脉根部病变面积及脂质沉积均增多(P < 0.01);与模型组相比,水苏碱组、阿托伐他汀组小鼠主动脉根部病变面积、脂质沉积均减少(P < 0.05或P < 0.01);水苏碱组小鼠主动脉根部病变面积及脂质沉积与阿托伐他汀相比差异无显著性意义(P > 0.05),见图1C,D。提示水苏碱治疗能减轻动脉粥样硬化小鼠的血管损伤。 2.3 水苏碱缓解动脉粥样硬化小鼠血管炎症 RT-qPCR检测各组ApoE-/-基因敲除小鼠主动脉中黏附分子及趋化因子mRNA表达,见图2所示。与空白对照组相比,模型组细胞间黏附分子1、血管细胞黏附分子1、选择素E、CXCL1、CXCL4、单核细胞趋化蛋白1 mRNA表达均升高(P均< 0.01);与模型组相比,水苏碱组、阿托伐他汀组细胞间黏附分子1、血管细胞黏附分子1、选择素E、CXCL1、CXCL4、单核细胞趋化蛋白1 mRNA表达均降低(P < 0.05或P < 0.01);水苏碱组细胞间黏附分子1、血管细胞黏附分子1、选择素E、CXCL1、CXCL4、单核细胞趋化蛋白1 mRNA与阿托伐他汀组比较差异均无显著性意义(P > 0.05)。提示水苏碱治疗能缓解动脉粥样硬化小鼠的血管炎症。"
| [1] LIN J, GU M, WANG X, et al. Huanglian Jiedu decoction inhibits vascular smooth muscle cell-derived foam cell formation by activating autophagy via suppressing P2RY12. J Ethnopharmacol. 2024;328:118125. [2] WANG XP, REN B, WANG QN, et al. Encephaloduroarteriosynangiosis for Symptomatic Intracranial Atherosclerotic Arterial Steno-Occlusive Disease: Clinical and Radiological Outcomes. J Am Heart Assoc. 2024; 13(15):e034707. [3] KNEUER JM, GRAJEK IA, WINKLER M, et al. Novel Long Noncoding RNA HEAT4 Affects Monocyte Subtypes, Reducing Inflammation and Promoting Vascular Healing. Circulation. 2024. doi: 10.1161/CIRCULATIONAHA.124.069315. [4] DONG M, CHEN M, ZHANG Y, et al. Oscillatory shear stress promotes endothelial senescence and atherosclerosis via STING activation. Biochem Biophys Res Commun. 2024;715:149979. [5] KOKAI D, MARKOVIC FILIPOVIC J, OPACIC M, et al. In vitro and in vivo exposure of endothelial cells to dibutyl phthalate promotes monocyte adhesion. Food Chem Toxicol. 2024;188:114663. [6] LI W, BAI P, LI W. UHRF1 inhibition mitigates vascular endothelial cell injury and ameliorates atherosclerosis in mice via regulating the SMAD7/YAP1 axis. Mol Immunol. 2024;170:119-130. [7] CHENG F, ZHOU Y, WANG M, et al. A review of pharmacological and pharmacokinetic properties of stachydrine. Pharmacol Res. 2020;155: 104755. [8] LIAO L, TANG Y, LI B, et al. Stachydrine, a potential drug for the treatment of cardiovascular system and central nervous system diseases. Biomed Pharmacother. 2023;161:114489. [9] MENG J, ZHOU C, ZHANG W, et al. Stachydrine prevents LPS-induced bone loss by inhibiting osteoclastogenesis via NF-kappaB and Akt signalling. J Cell Mol Med. 2019;23(10):6730-6743. [10] LIU FC, YU HP, LEE HC, et al. The Modulation of Phospho-Extracellular Signal-Regulated Kinase and Phospho-Protein Kinase B Signaling Pathways plus Activity of Macrophage-Stimulating Protein Contribute to the Protective Effect of Stachydrine on Acetaminophen-Induced Liver Injury. Int J Mol Sci. 2024;25(3):1484. [11] PAREKH T, TSAI M, SPIRO S. Choline degradation in Paracoccus denitrificans: identification of sources of formaldehyde. J Bacteriol. 2024;206(4):e0008124. [12] ZENG H, XU D, SONG Y, et al. Synthesis, characterization and anti-breast cancer activities of stachydrine derivatives. Eur J Med Chem. 2023;259:115679. [13] XIE X, YANG C, CUI Q, et al. Stachydrine Mediates Rapid Vascular Relaxation: Activation of Endothelial Nitric Oxide Synthase Involving AMP-Activated Protein Kinase and Akt Phosphorylation in Vascular Endothelial Cells. J Agric Food Chem. 2019;67(35):9805-9811. [14] KIM H, APPEL LJ, LICHTENSTEIN AH, et al. Metabolomic Profiles Associated With Blood Pressure Reduction in Response to the DASH and DASH-Sodium Dietary Interventions. Hypertension. 2023; 80(7):1494-1506. [15] NAJEM MY, RYS RN, LAURANCE S, et al. Extracellular RNA Induces Neutrophil Recruitment Via Toll-Like Receptor 3 During Venous Thrombosis After Vascular Injury. J Am Heart Assoc. 2024;13(15): e034492. [16] SHAPIRA KE, SHAPIRA G, SCHMUKLER E, et al. Autophagy is induced and modulated by cholesterol depletion through transcription of autophagy-related genes and attenuation of flux. Cell Death Discov. 2021;7(1):320. [17] OU H, LIU C, FENG W, et al. Role of AMPK in atherosclerosis via autophagy regulation. Sci China Life Sci. 2018;61(10):1212-1221. [18] TIAN Z, NING H, WANG X, et al. Endothelial Autophagy Promotes Atheroprotective Communication Between Endothelial and Smooth Muscle Cells via Exosome-Mediated Delivery of miR-204-5p. Arterioscler Thromb Vasc Biol. 2024;44(8):1813-1832. [19] MANTA CP, LEIBING T, FRIEDRICH M, et al. Targeting of Scavenger Receptors Stabilin-1 and Stabilin-2 Ameliorates Atherosclerosis by a Plasma Proteome Switch Mediating Monocyte/Macrophage Suppression. Circulation. 2022;146(23):1783-1799. [20] JANG E, HO T WW, BRUMELL J, et al. IL-1beta Induces LDL Transcytosis by a Novel Pathway Involving LDLR and Rab27a. Arterioscler Thromb Vasc Biol. 2024;44(9):2053-2068. [21] KANE J, VOS WG, BOSMANS LA, et al. Peritoneal Dialysis Aggravates and Accelerates Atherosclerosis in Uremic ApoE(-/-) Mice. J Am Heart Assoc. 2024;13(14):e034066. [22] TIAN S, MIAO M, BAI M, et al. Effect of stachydrine hydrochloride to the prostate hyperplasia model in mice. Saudi J Biol Sci. 2019;26(4): 782-789. [23] LEOW SS, KHOO JS, LEE WK, et al. RNA-Seq transcriptome profiling of Nile rat livers reveals novel insights on the anti-diabetic mechanisms of Water-Soluble Palm Fruit Extract. J Appl Genet. 2024. doi: 10.1007/s13353-024-00880-1. [24] ZULOAGA R, DETTLEFF P, BASTIAS-MOLINA M, et al. RNA-Seq-Based Analysis of Cortisol-Induced Differential Gene Expression Associated with Piscirickettsia salmonis Infection in Rainbow Trout (Oncorhynchus mykiss) Myotubes. Animals (Basel). 2021;11(8):2399. [25] MA D, LIU S, LIU K, et al. MDFI promotes the proliferation and tolerance to chemotherapy of colorectal cancer cells by binding ITGB4/LAMB3 to activate the AKT signaling pathway. Cancer Biol Ther. 2024;25(1):2314324. [26] XU H, DU Z, LI Z, et al. MUC1-EGFR crosstalk with IL-6 by activating NF-kappaB and MAPK pathways to regulate the stemness and paclitaxel-resistance of lung adenocarcinoma. Ann Med. 2024;56(1):2313671. [27] LU Y, GAO L, ZHANG W, et al. Caffeic acid phenethyl ester restores mitochondrial homeostasis against peritoneal fibrosis induced by peritoneal dialysis through the AMPK/SIRT1 pathway. Ren Fail. 2024; 46(1):2350235. [28] KARLIN H, SOODA M, LARSON M, et al. Plasma Extracellular MicroRNAs Associated With Cardiovascular Disease Risk Factors in Middle-Aged and Older Adults. J Am Heart Assoc. 2024;13(12):e033674. [29] SANTULLI G, VARZIDEH F, FORZANO I, et al. Functional and Clinical Importance of SGLT2-inhibitors in Frailty: From the Kidney to the Heart. Hypertension. 2023;80(9):1800-1809. [30] ZHU X, WU Y, ZHANG X, et al. Stachydrine ameliorates hypoxia reoxygenation injury of cardiomyocyte via enhancing SIRT1-Nrf2 pathway. J Cardiothorac Surg. 2023;18(1):265. [31] LU S, LIANG Y, YANG S, et al. Stachydrine Hydrochloride Regulates the NOX2-ROS-Signaling Axis in Pressure-Overload-Induced Heart Failure. Int J Mol Sci. 2023;24(18):14369. [32] ZHOU F, LIU F, LIU J, et al. Stachydrine promotes angiogenesis by regulating the VEGFR2/MEK/ERK and mitochondrial-mediated apoptosis signaling pathways in human umbilical vein endothelial cells. Biomed Pharmacother. 2020;131:110724. [33] HU Y, HE K, ZHU H. Chinese herbal medicinal ingredients affect secretion of NO, IL-10, ICAM-1 and IL-2 by endothelial cells. Immunopharmacol Immunotoxicol. 2015;37(3):324-328. [34] LI WW, GUO ZM, WANG BC, et al. PCSK9 induces endothelial cell autophagy by regulating the PI3K/ATK pathway in atherosclerotic coronary heart disease. Clin Hemorheol Microcirc. 2024. doi: 10.3233/CH-242172. [35] AKHTAR S, SAGAR K, SINGH A, et al. Inflammation-induced sialin mediates nitrate efflux in dysfunctional endothelium affecting NO bioavailability. Nitric Oxide. 2024;146:37-47. [36] ZHU L, GUO L, XU J, et al. Postprandial Triglyceride-Rich Lipoproteins-Induced Lysosomal Dysfunction and Impaired Autophagic Flux Contribute to Inflammation in White Adipocytes. J Nutr. 2024;154(5): 1619-1630. [37] BARANGI S, HAYES AW, KARIMI G. The role of lncRNAs/miRNAs/Sirt1 axis in myocardial and cerebral injury. Cell Cycle. 2023;22(9):1062-1073. [38] CHENG J, PAN W, ZHENG Y, et al. Piezocatalytic Schottky Junction Treats Atherosclerosis by a Biomimetic Trojan Horse Strategy. Adv Mater. 2024;36(19):e2312102. [39] HUI B, HOU X, LIU R, et al. Gypenoside inhibits ox-LDL uptake and foam cell formation through enhancing Sirt1-FOXO1 mediated autophagy flux restoration. Life Sci. 2021;264:118721. [40] XU H, FU J, TU Q, et al. The SGLT2 inhibitor empagliflozin attenuates atherosclerosis progression by inducing autophagy. J Physiol Biochem. 2024;80(1):27-39. [41] LI D, ZHANG Y, MA J, et al. Adenosine monophosphate activated protein kinase regulates ABCG1-mediated oxysterol efflux from endothelial cells and protects against hypercholesterolemia-induced endothelial dysfunction. Arterioscler Thromb Vasc Biol. 2010;30(7):1354-1362. |
| [1] | Wang Mingqi, Feng Shiya, Han Yinhe, Yu Pengxin, Guo Lina, Jia Zixuan, Wang Xiuli. Construction and evaluation of a neuralized intestinal mucosal tissue engineering model in vitro [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 892-900. |
| [2] | Wang Jie, Huang Rui, Zhang Ye, Shou Zhaoxi, Yao Jie, Liu Chenxi, Liao Jian. Role and mechanism of probiotics in peri-implantitis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 901-907. |
| [3] | Yang Xiao, Bai Yuehui, Zhao Tiantian, Wang Donghao, Zhao Chen, Yuan Shuo. Cartilage degeneration in temporomandibular joint osteoarthritis: mechanisms and regenerative challenges [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 926-935. |
| [4] | Zhang Yibo, Lu Jianqi, Mao Meiling, Pang Yan, Dong Li, Yang Shangbing, Xiao Xiang. Exploring the causal relationship between rheumatoid arthritis and coronary atherosclerosis: a Mendel randomized study involving serum metabolites and inflammatory factors [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [5] | Li Huayuan, Li Chun, Liu Junwei, Wang Ting, Li Long, Wu Yongli. Effect of warm acupuncture on PINK1/Parkin pathway in the skeletal muscle of rats with chronic fatigue syndrome [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1618-1625. |
| [6] | Zhou Panpan, Cui Yinglin, Zhang Wentao, Wang Shurui, Chen Jiahui, Yang Tong . Role of cellular autophagy in cerebral ischemic injury and the regulatory mechanism of traditional Chinese medicine [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1650-1658. |
| [7] | Zhu Hanmin, Wang Song, Xiao Wenlin, Zhang Wenjing, Zhou Xi, He Ye, Li Wei, . Mitophagy regulates bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1676-1683. |
| [8] | Zheng Rongfa, Mo Weibin, Huang Peng, Chen Junji, Liang Ting, Zi Fangyu, Li Guofeng. Effects of electroacupuncture on the expression of metabolic enzymes and autophagy genes in gastrocnemius muscle tissues of exercising rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1127-1136. |
| [9] | Chen Yuning, Jiang Ying, Liao Xiangyu, Chen Qiongjun, Xiong Liang, Liu Yue, Liu Tong. Buqi Huoxue Compounds intervene with the expression of related factors and autophagy related proteins in a rat model of cerebral ischemia/reperfusion [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1152-1158. |
| [10] | He Bo, Chen Wen, Ma Suilu, He Zhijun, Song Yuan, Li Jinpeng, Liu Tao, Wei Xiaotao, Wang Weiwei, Xie Jing . Pathogenesis and treatment progress of flap ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1230-1238. |
| [11] | Gao Yang, Qin Hewei, Liu Dandan. ACSL4 mediates ferroptosis and its potential role in atherosclerotic cardiovascular disease [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1239-1247. |
| [12] | Liu Lingyun, He Guixin, Qin Weibin, Song Hui, Zhang Liwen, Tang Weizhi, Yang Feifei, Zhu Ziyi, Ou Yangbin . Improvement of myocardial injury by traditional Chinese medicine: mitochondrial calcium homeostasis mediates macrophage autophagy and pyroptosis pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1276-1284. |
| [13] | Xu Tianjie, Fan Jiaxin, Guo Xiaoling, Jia Xiang, Zhao Xingwang, Liu kainan, Wang Qian. Metformin exerts a protective effect on articular cartilage in osteoarthritis rats by inhibiting the PI3K/AKT/mTOR pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1003-1012. |
| [14] | Liu Xuan, Ding Yuqing, Xia Ruohan, Wang Xianwang, Hu Shujuan. Exercise prevention and treatment of insulin resistance: role and molecular mechanism of Keap1/nuclear factor erythroid2-related factor 2 signaling pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7578-7588. |
| [15] | Gong Yuehong, Wang Mengjun, Ren Hang, Zheng Hui, Sun Jiajia, Liu Junpeng, Zhang Fei, Yang Jianhua, Hu Junping. Machine learning combined with bioinformatics screening of key genes for pulmonary fibrosis associated with cellular autophagy and experimental validation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7679-7689. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||