Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (20): 4369-4378.doi: 10.12307/2025.689
Previous Articles Next Articles
Relationship between intervertebral disc degeneration and 473 gut microbiotas: what can be learned from big data information in the FinnGen database
Wang Zikun1, Li Shudong2, Gao Shuang1, Fan Shuhao1, Li Cheng3, Meng Chunyang4
- 1Shandong First Medical University (Shandong Academy of Medical Sciences), Jinan 250117, Shandong Province, China; 2First Clinical Medical College, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China; 3College of Clinical Medicine, Jining Medical University, Jining 272067, Shandong Province, China; 4Department of Spine Surgery, Affiliated Hospital of Jining Medical University, Jining 272000, Shandong Province, China
-
Received:2024-08-01Accepted:2024-09-09Online:2025-07-18Published:2024-12-25 -
Contact:Meng Chunyang, MD, Chief physician, Doctoral supervisor, Department of Spine Surgery, Affiliated Hospital of Jining Medical University, Jining 272000, Shandong Province, China -
About author:Wang Zikun, Master’s candidate, Shandong First Medical University (Shandong Academy of Medical Sciences), Jinan 250117, Shandong Province, China -
Supported by:The National Natural Science Foundation of China (General Program), No. 82372477 (to MCY); Shandong Province Natural Science Foundation (Key Project), No. ZR2020KH010 (to MCY)
CLC Number:
Cite this article
Wang Zikun, Li Shudong, Gao Shuang, Fan Shuhao, Li Cheng, Meng Chunyang. Relationship between intervertebral disc degeneration and 473 gut microbiotas: what can be learned from big data information in the FinnGen database[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(20): 4369-4378.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
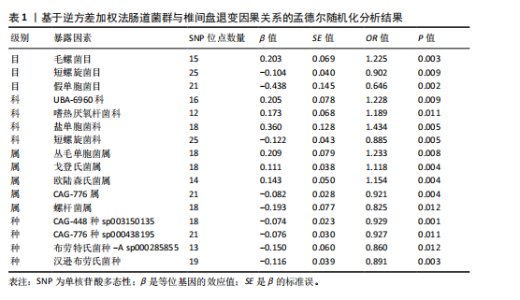
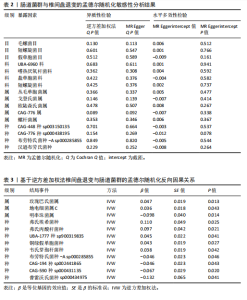
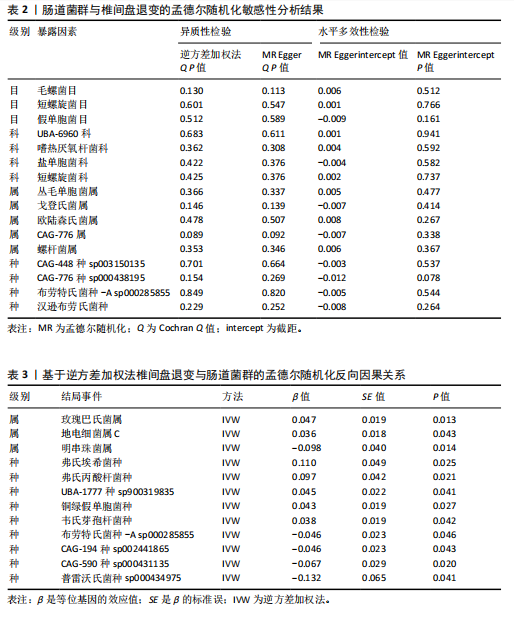
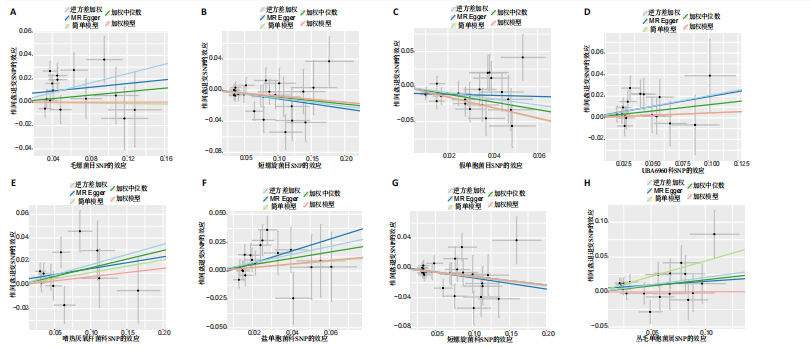
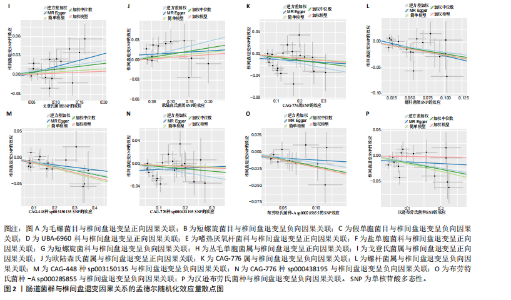
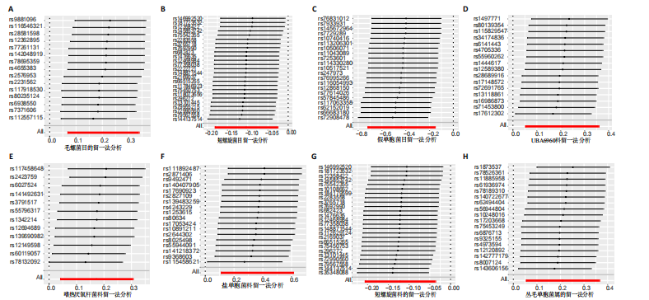
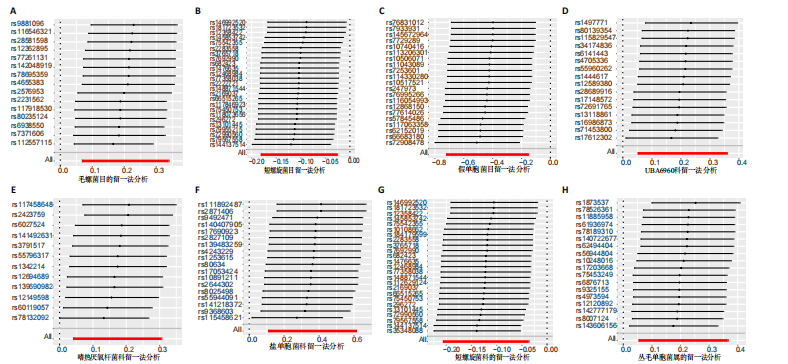
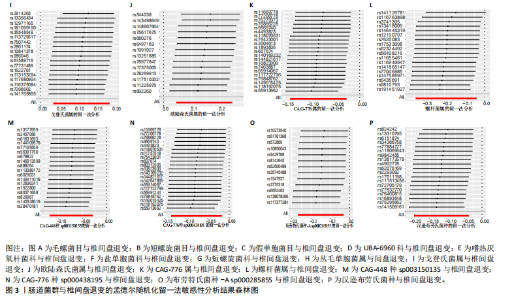
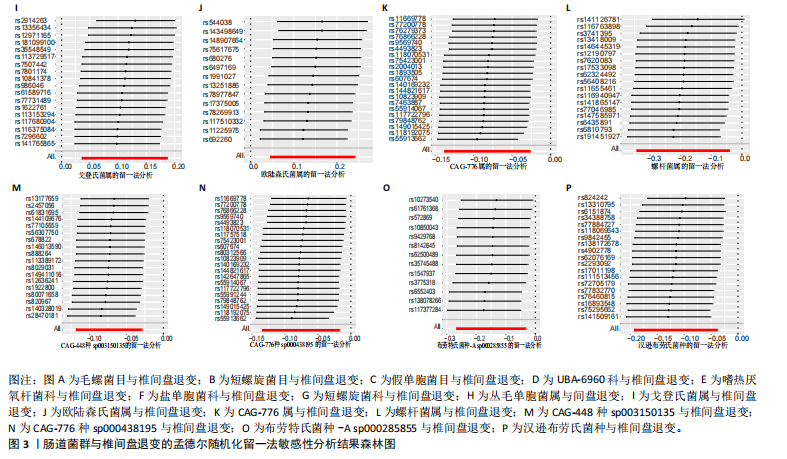
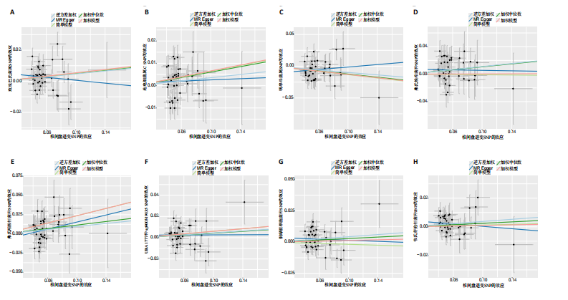
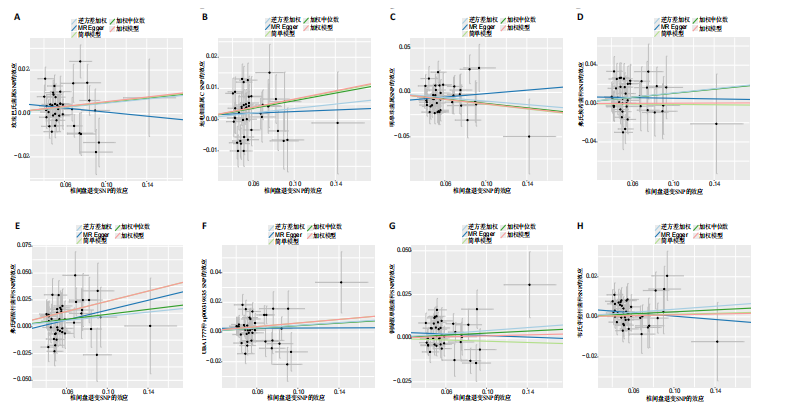
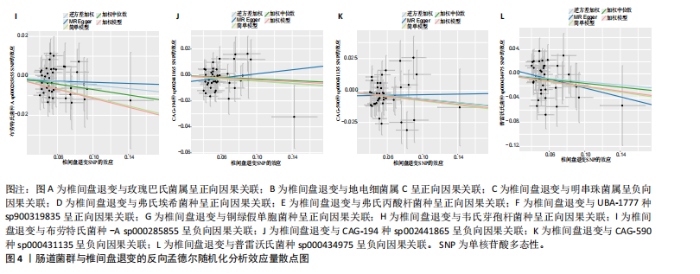
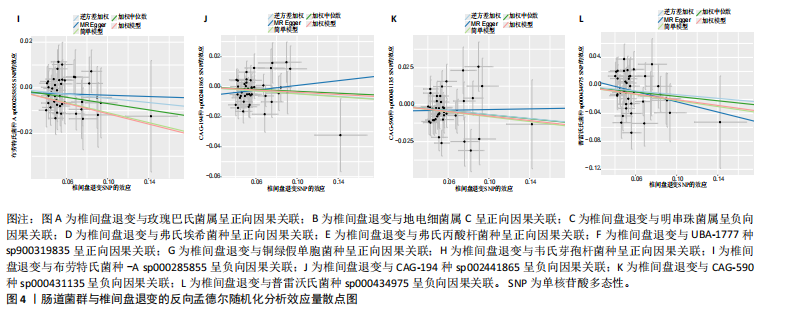
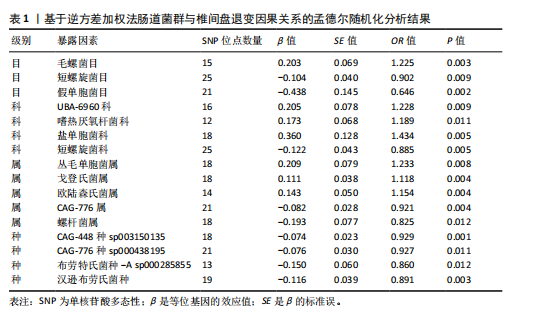
2.1 肠道菌群对椎间盘退变的因果关系 文章基于工具变量的筛选标准,全基因组统计学显著阈值P < 1×10-5 ;以逆方差加权法作为主要参考依据,以P < 0.05为标准,对473个肠道菌群进行孟德尔随机化分析。所纳入单一单核苷酸多态性的 F 统计量均大于10,说明所有单核苷酸多态性均为强工具变量。在正向孟德尔随机化分析过程中,共筛选出41种肠道菌群与椎间盘退变存在因果关系,包含776个单核苷酸多态性。其中18个单核苷酸多态性与CAG-448种sp003150135相关,19个单核苷酸多态性与汉逊布劳氏菌种相关,15个单核苷酸多态性与毛螺菌属相关,21个单核苷酸多态性与CAG-776属相关,18个单核苷酸多态性与戈登氏菌属相关,14个单核苷酸多态性与欧陆森氏菌属-C相关,18个单核苷酸多态性与盐单胞菌科相关,25个单核苷酸多态性与短螺旋菌科相关,18个单核苷酸多态性丛毛单胞菌属相关,16个单核苷酸多态性与UBA-6960科相关,25个单核苷酸多态性与短螺旋菌目相关,12个单核苷酸多态性与嗜热厌氧杆菌科相关,21个单核苷酸多态性与CAG-776种sp000438195相关,13个单核苷酸多态性与布劳特氏菌种-A sp000285855相关,18个单核苷酸多态性与螺杆菌属相关,18个单核苷酸多态性与CAG-448属相关,21个单核苷酸多态性与堆囊菌属相关,12个单核苷酸多态性与卡氏双歧杆菌种相关,11个单核苷酸多态性与嗜氢菌属相关,18个单核苷酸多态性与UBA-3792属相关,23个单核苷酸多态性与大肠杆菌属相关,19个单核苷酸多态性与真杆菌种-F sp000434115相关,18个单核苷酸多态性与多形粪球菌种相关,22个单核苷酸多态性与奇异菌科相关,19个单核苷酸多态性与CAG-433科相关,19个单核苷酸多态性与梭杆菌属-A相关,21个单核苷酸多态性与CAG-1000种sp000434555相关,16个单核苷酸多态性与经黏液真杆菌种sp001304935相关,13个单核苷酸多态性与UBA-11963属相关,14个单核苷酸多态性与发光杆菌属相关,22个单核苷酸多态性与蓝细菌门相关,21个单核苷酸多态性与金黄色葡萄球菌种相关,22个单核苷酸多态性与大肠杆菌属相关,17个单核苷酸多态性与RUG-420种sp900317985相关,28个单核苷酸多态性与鲸杆菌属-A相关,23个单核苷酸多态性与独岛杆菌属相关,26个单核苷酸多态性与劳森氏菌种sp900066645相关,30个单核苷酸多态性与CAG-632属相关,18个单核苷酸多态性与CAG-488种sp000434055相关,13个单核苷酸多态性与费氏弧菌属相关。其中通过水平多效性和异质性检验,发现独岛杆菌属与劳森氏菌种sp900066645具有显著性(P < 0.05),说明这两种肠道菌群不仅与暴露因素有关,还与其他潜在的混杂因素有关,故排除这两种肠道菌群的影响。综上,文章中展示与椎间盘退变具有显著因果关系的16种肠道菌群的孟德尔随机化分析结果,见表1。 逆方差加权法分析的结果显示,毛螺菌目(OR=1.225,95%CI:1.070-1.403,P=0.003),UBA-6960科(OR=1.228,95%CI:1.053-1.431,P=0.009),嗜热厌氧杆菌科(OR=1.189,95%CI:1.041-1.357,P=0.011),盐单胞菌科(OR=1.434,95%CI:1.115-1.843,P=0.005),丛毛单菌属(OR=1.233,95%CI:1.055-1.441,P=0.008),戈登氏菌属(OR=1.118,95%CI:1.036-1.205,P=0.004),欧陆森氏菌属(OR=1.154,95%CI:1.047-1.272,P=0.004),与椎间盘退变呈现正相关。短螺旋菌目(OR= 0.902,95%CI:0.834-0.974,P=0.009),假单胞菌目(OR=0.646,95%CI:0.486-0.857,P=0.002),短螺旋菌科(OR=0.885,95%CI:0.813-0.964,P= 0.005),CAG-776属(OR=0.921,95%CI:0.871-0.973,P=0.004),螺杆菌属(OR=0.825,95%CI:0.709-0.959,P=0.012),CAG-448种sp003150135 (OR=0.929,95%CI:0.888-0.971,P=0.001),CAG-776种sp000438195 (OR=0.927,95%CI:0.874-0.983,P=0.011),布劳特氏菌种-A sp000285855(OR=0.860,95%CI:0.765-0.967,P=0.012),汉逊布劳氏菌种(OR=0.891,95%CI:0.824-0.962,P=0.003),与椎间盘退变呈现负相关,见图2。 根据异质性检验和水平多效性检验结果,通过Cochran’s Q检验结果表明,所选工具变量之间没有明显的异质性,MR-Egger截距检验结果表明,所选工具变量之间没有明显的水平多效性,P 值均大于0.05。由此证明,此孟德尔随机化分析结果不存在异质性和水平多效性,见表2。留一法检验结果显示不存在单个单核苷酸多态性对因果关系估计值产生较大影响,因此证明,此孟德尔随机化分析结果较为稳定,见图3。 2.2 椎间盘退变对肠道菌群的因果关系 通过对椎间盘退变与473种肠道菌群进行反向孟德尔随机化分析,共检测到12种肠道菌群与椎间盘退变间存在反向因果关系,见表3,分析结果显示,椎间盘退变与玫瑰巴氏菌属、地电细菌属 C、弗氏埃希菌种、弗氏丙酸杆菌种、UBA-1777种sp900319835、铜绿假单胞菌种和韦氏芽孢杆菌种呈正相关,与明串珠菌属、普雷沃氏菌种sp000434975、布劳特氏菌种-A sp000285855、CAG-194种sp002441865和CAG-590种sp000431135呈负相关,见图4。反向孟德尔随机化结果敏感性分析结果显示,均未发现存在异质性或水平多效性。"
| [1] QIN C, CHEN M, YU Q, et al. Causal relationship between the blood immune cells and intervertebral disc degeneration: univariable, bidirectional and multivariable Mendelian randomization. Front Immunol. 2023;14:1321295. [2] GAO B, JIANG B, XING W, et al. Discovery and application of postnatal nucleus pulposus progenitors essential for intervertebral disc homeostasis and degeneration. Adv Sci (Weinh). 2022;9(13):e2104888. [3] KANG L, ZHANG H, JIA C, et al. Epigenetic modifications of inflammation in intervertebral disc degeneration. Ageing Res Rev. 2023;87:101902. [4] 卢世浩,张子凡,孙柏峰,等.间充质干细胞移植治疗椎间盘退变植入途径的研究进展[J].中国脊柱脊髓杂志,2023, 33(11):1052-1056. [5] XU J, SHAO T, LOU J, et al. Aging, cell senescence, the pathogenesis and targeted therapies of intervertebral disc degeneration. Front Pharmacol. 2023;14: 1172920. [6] DING SL, ZHANG TW, ZHANG QC, et al. Excessive mechanical strain accelerates intervertebral disc degeneration by disrupting intrinsic circadian rhythm. Exp Mol Med. 2021;53(12):1911-1923. [7] MARFIA G, GUARNACCIA L, NAVONE SE, et al. Microgravity and the intervertebral disc: the impact of space conditions on the biomechanics of the spine. Front Physiol. 2023;14:1124991. [8] CHEN HH, HSU HT, LIAO MH, et al. Effects of sex and obesity on LEP variant and leptin level associations in intervertebral disc degeneration. Int J Mol Sci. 2022;23(20): 12275. [9] OU-YANG DC, KLECK CJ, ACKERT-BICKNELL CL. Genetics of intervertebral disc degeneration. Curr Osteoporos Rep. 2023; 21(1):56-64. [10] XIA Q, ZHAO Y, DONG H, et al. Progress in the study of molecular mechanisms of intervertebral disc degeneration. Biomed Pharmacother. 2024;174:116593. [11] 马玮玮,陈虹谷,李彤彤,等.基于孟德尔随机化分析肠道菌群与骨密度的因果关系[J].中国骨质疏松杂志,2023,29(12): 1780-1785. [12] MA PJ, WANG MM, WANG Y. Gut microbiota: a new insight into lung diseases. Biomed Pharmacother. 2022;155:113810. [13] FAN Y, PEDERSEN O. Gut microbiota in human metabolic health and disease. Nat Rev Microbiol. 2021;19(1):55-71. [14] RAJASEKARAN S, SOUNDARARAJAN DCR, TANGAVEL C, et al. Human intervertebral discs harbour a unique microbiome and dysbiosis determines health and disease. Eur Spine J. 2020;29(7):1621-1640. [15] NI S, HUANG X, LI X, et al. METTL3 promotes nucleus pulposus cell senescence in intervertebral disc degeneration by regulating TLR2 m6A methylation and gut microbiota. J Gerontol A Biol Sci Med Sci. 2024;79(8):glae150. [16] BIRNEY E. Mendelian Randomization. Cold Spring Harb Perspect Med. 2022;12(4): 4913-4924. [17] GILL D, WALKER VM, MARTIN RM, et al. Comparison with randomized controlled trials as a strategy for evaluating instruments in Mendelian randomization. Int J Epidemiol. 2020;49(4):1404-1406. [18] 柴金莲,李树栋,李威,等.肠道菌群与药物相关性骨坏死:两样本双向孟德尔随机化分析[J].中国组织工程研究, 2024,28(27):4325-4331. [19] LEVIN M G, BURGESS S. Mendelian randomization as a tool for cardiovascular research: a review. JAMA Cardiol. 2024; 9(1):79-89. [20] QIN Y, HAVULINNA AS, LIU Y, et al. Combined effects of host genetics and diet on human gut microbiota and incident disease in a single population cohort. Nat Genet. 2022;54(2):134-142. [21] XU J, ZHANG S, TIAN Y, et al. Genetic causal association between iron status and osteoarthritis: a two-sample mendelian randomization. Nutrients. 2022; 14(18):3683. [22] MOUNIER N, KUTALIK Z. Bias correction for inverse variance weighting Mendelian randomization. Genet Epidemiol. 2023; 47(4):314-331. [23] XIAO G, HE Q, LIU L, et al. Causality of genetically determined metabolites on anxiety disorders: a two-sample Mendelian randomization study. J Transl Med. 2022; 20(1):475.
[24] DENG Y, WONG MCS. Association between rheumatoid arthritis and osteoporosis in japanese populations: a mendelian randomization study. Arthritis Rheumatol. 2023;75(8):1334-1343. [25] LIU Z, WANG H, YANG Z, et al. Causal associations between type 1 diabetes mellitus and cardiovascular diseases: a Mendelian randomization study. Cardiovasc Diabetol. 2023;22(1):236. [26] ZHANG GZ, DENG YJ, XIE QQ, et al. Sirtuins and intervertebral disc degeneration: roles in inflammation, oxidative stress, and mitochondrial function. Clin Chim Acta. 2020;508:33-42. [27] LIN J, ZHENG X, XIONG Z, et al. DJ-1- mediated p62 degradation delays intervertebral disc degeneration by inhibiting apoptosis of nucleus pulposus cells. Apoptosis. 2023;28(9-10):1357-1371. [28] WANG D, SHANG Q, MAO J, et al. Phosphorylation of KRT8 (keratin 8) by excessive mechanical load-activated PKN (protein kinase N) impairs autophagosome initiation and contributes to disc degeneration. Autophagy. 2023;19(9): 2485-2503. [29] YAO B, CAI Y, WANG W, et al. The effect of gut microbiota on the progression of intervertebral disc degeneration. Orthop Surg. 2023;15(3):858-867. [30] LYU FJ, CUI H, PAN H, et al. Painful intervertebral disc degeneration and inflammation: from laboratory evidence to clinical interventions. Bone Res. 2021;9(1):7. [31] LIN B, WANG Y, ZHANG P, et al. Gut microbiota regulates neuropathic pain: potential mechanisms and therapeutic strategy. J Headache Pain. 2020;21(1):103. [32] WANG J, ZHU N, SU X, et al. Gut-microbiota-derived metabolites maintain gut and systemic immune homeostasis. Cells. 2023; 12(5):793. [33] ZHENG D, LIWINSKI T, ELINAV E. Interaction between microbiota and immunity in health and disease. Cell Res. 2020;30(6):492-506. [34] SONG C, ZHOU Y, CHENG K, et al. Cellular senescence - Molecular mechanisms of intervertebral disc degeneration from an immune perspective. Biomed Pharmacother. 2023;162:114711. [35] SUN Y, CHEN Q, LIN P, et al. Characteristics of Gut microbiota in patients with rheumatoid arthritis in Shanghai, China. Front Cell Infect Microbiol. 2019;9:369. [36] KRITSCHIL R, SCOTT M, SOWA G, et al. Role of autophagy in intervertebral disc degeneration. J Cell Physiol. 2022; 237(2):1266-1284. [37] FAN C, CHU G, YU Z, et al. The role of ferroptosis in intervertebral disc degeneration. Front Cell Dev Biol. 2023;11: 1219840. [38] HODGKINSON K, EL ABBAR F, DOBRANOWSKI P, et al. Butyrate’s role in human health and the current progress towards its clinical application to treat gastrointestinal disease. Clin Nutr. 2023; 42(2):61-75. [39] GENG Z, WANG J, CHEN G, et al. Gut microbiota and intervertebral disc degeneration: a bidirectional two-sample Mendelian randomization study. J Orthop Surg Res. 2023;18(1):601. [40] MOHAMMAD S, THIEMERMANN C. Role of metabolic endotoxemia in systemic inflammation and potential interventions. Front Immunol. 2020;11:594150. [41] D’AMICO D, OLMER M, FOUASSIER AM, et al. Urolithin A improves mitochondrial health, reduces cartilage degeneration, and alleviates pain in osteoarthritis. Aging Cell. 2022;21(8):e13662. [42] GARCIA-VILLALBA R, BELTRAN D, FRUTOS MD, et al. Metabolism of different dietary phenolic compounds by the urolithin-producing human-gut bacteria Gordonibacter urolithinfaciens and Ellagibacter isourolithinifaciens. Food Funct. 2020;11(8):7012-7022. [43] LIN J, ZHUGE J, ZHENG X, et al. Urolithin A-induced mitophagy suppresses apoptosis and attenuates intervertebral disc degeneration via the AMPK signaling pathway. Free Radic Biol Med. 2020;150: 109-119. [44] SHI PZ, WANG JW, WANG PC, et al. Urolithin a alleviates oxidative stress-induced senescence in nucleus pulposus-derived mesenchymal stem cells through SIRT1/PGC-1alpha pathway. World J Stem Cells. 2021;13(12):1928-1946. [45] MA L, NI Y, WANG Z, et al. Spermidine improves gut barrier integrity and gut microbiota function in diet-induced obese mice. Gut Microbes. 2020;12(1):1-19. [46] ZHENG D, WU Z, LI L, et al. Genetic analysis of the causal relationship between gut microbiota and intervertebral disc degeneration: a two-sample Mendelian randomized study. Eur Spine J. 2024;33(5): 1986-1998. [47] SHAHI SK, FREEDMAN SN, Murra AC, et al. Prevotella histicola, a human gut commensal, is as potent as COPAXONE® in an animal model of multiple sclerosis. Front Immunol. 2019;10:462. |
| [1] | Qian Kun, Li Ziqing, Sun Shui . Endoplasmic reticulum stress in the occurrence and development of common degenerative bone diseases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1285-1295. |
| [2] |
Zhao Wensheng, Li Xiaolin, Peng Changhua, Deng Jia, Sheng Hao, Chen Hongwei, Zhang Chaoju, He Chuan.
Gut microbiota and osteoporotic fractures #br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1296-1304.
|
| [3] | Li Jiatong, Jin Yue, Liu Runjia, Song Bowen, Zhu Xiaoqian, Li Nianhu . Association between thyroid function levels and phenotypes associated with sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1312-1320. |
| [4] |
Sun Guanghan, Xie Zhencong, Sun Mi, Xu Yang, Guo Dong.
Therapeutic effect and mechanism by which Trichosanthis Fructus-Allii Macrostemonis Bulbus regulates gut microbiota in a rat model of coronary heart disease #br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 917-927.
|
| [5] | Xiang Pan, Che Yanjun, Luo Zongping. Compressive stress induces degeneration of cartilaginous endplate cells through the SOST/Wnt/beta-catenin pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 951-957. |
| [6] | Ding Zhili, Huang Jie, Jiang Qiang, Li Tusheng, Liu Jiang, Ding Yu. Constructing rabbit intervertebral disc degeneration models by different methods under X-ray guidance: a comparative study [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 995-1002. |
| [7] | Wu Guangtao, Qin Gang, He Kaiyi, Fan Yidong, Li Weicai, Zhu Baogang, Cao Ying . Causal relationship between immune cells and knee osteoarthritis: a two-sample bi-directional Mendelian randomization analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1081-1090. |
| [8] | Su Yongkun, Sun Hong, Liu Miao, Yang Hua, Li Qingsong. Development of novel antioxidants and antioxidant combination carried by nano-hydrogel systems in treatment of intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7376-7384. |
| [9] | Yu Qinghe, Cai Ziming, Wu Jintao, Ma Pengfei, Zhang Xin, Zhou Longqian, Wang Yakun, Lin Xiaoqin, Lin Wenping. Vanillic acid inhibits inflammatory response and extracellular matrix degradation of endplate chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6391-9397. |
| [10] | Cui Yuena, Chen Xiaoyu, Liang Meiting, Chen Wujin, He Yi, Dilinur·Ekpa, Du Manxi, Zhu Yuqiu, Abuduwupuer·Haibier, Sun Yuping. Differences of calorie restriction and time-restricted feeding on metabolic indices and gut microbiota of mice [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6449-6456. |
| [11] | Gao Xilin, Wu Si Zhang Chao Zhu Liguo, Fu Bifeng, Wang Ping. Mechanotransduction proteins in intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 579-589. |
| [12] | Xi Haixiang, Duan Jie, Xu Ping, Fei Xi, Li Xiaoping, Cao Lei, Tang Guangping, Zhang Lei. Syringin-chitosan hydrogel suppresses intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(28): 5968-5976. |
| [13] | Ma Jikun, Wang Jianru, Qi Junjie, Liu Haifei. Mechanism by which diabetes exacerbates intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5907-5913. |
| [14] | Zeng Hao, Zou Shunyi, Li Zhengpeng, Chai Yuan, Huang Yourong, Zhang Xiaoyun. Intestinal flora regulates bone metabolism: a visual analysis of literature from the Web of Science Core Collection [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(26): 5652-5661. |
| [15] | Yu Qinghe, Cai Ziming, Tian He, Li Pian, Ruan Ye, Liang Jinzhu, Lin Shuhui, Lin Wenping. Formononetin inhibits lipopolysaccharide-induced inflammation in nucleus pulposus mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(25): 5328-5334. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||