Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (22): 4731-4739.doi: 10.12307/2025.453
Previous Articles Next Articles
Amniotic and bladder extracellular matrix materials in repairing rat endometrial injury
Kong Xiaojuan1, Ma Zhengjiao2, Tan Zhenyu1, Liu Peng1
- 1First Affiliated Hospital of Hunan University of Chinese Medicine, Changsha 410000, Hunan Province, China; 2Department of Obstetrics and Gynecology, Wancheng District Traditional Chinese Medicine Hospital, Nanyang 473000, Henan Province, China
-
Received:2024-04-09Accepted:2024-05-17Online:2025-08-08Published:2024-12-06 -
Contact:Liu Peng, Master, Associate chief physician, First Affiliated Hospital of Hunan University of Chinese Medicine, Changsha 410000, Hunan Province, China -
About author:Kong Xiaojuan, Master, Associate chief physician, First Affiliated Hospital of Hunan University of Chinese Medicine, Changsha 410000, Hunan Province, China -
Supported by:Hunan University of Chinese Medicine University-Level Scientific Research Fund Project, No. ZYYDX201753 (to KXJ)
CLC Number:
Cite this article
Kong Xiaojuan, Ma Zhengjiao, Tan Zhenyu, Liu Peng. Amniotic and bladder extracellular matrix materials in repairing rat endometrial injury[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(22): 4731-4739.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

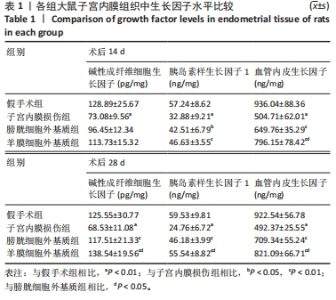
术后28 d,与假手术组相比,子宫内膜损伤组大鼠子宫内膜组织中3种生长因子水平均降低(P < 0.01);与子宫内膜损伤组相比,羊膜细胞外基质组与膀胱细胞外基质组大鼠子宫内膜组织中的3种生长因子水平均升高(P < 0.05或P < 0.01);与膀胱细胞外基质组相比,羊膜细胞外基质组大鼠子宫内膜组织中3种生长因子的浓度均升高(P < 0.05),见表1。 2.6 各组大鼠子宫内膜组织的形态观察 苏木精-伊红染色结果显示,假手术组大鼠子宫内膜组织形态正常,含有大量的腺体结构;子宫内膜损伤组大鼠子宫内膜发育不良,内膜厚度与腺体数量均明显减少;与子宫内膜损伤组相比,羊膜细胞外基质组与膀胱细胞外基质组术后14,28 d的大鼠子宫内膜形态有所恢复,内膜厚度与腺体数量较子宫内膜损伤组均增加;与膀胱细胞外基质组相比,羊膜细胞外基质组术后14,28 d的子宫内膜厚度与腺体数量增加,见图4。"

| [1] FITZGERALD HC, SCHUST DJ, SPENCER TE. In vitro models of the human endometrium: evolution and application for women’s health. Biol Reprod. 2021;104(2):282-293. [2] VILELLA F, WANG W, MORENO I, et al. Understanding the human endometrium in the 21st century.Am J Obstet Gynecol. 2021; 225(1):1-2. [3] OKOHUE JE, AMEH N, ADEWOLE A. Severity of intrauterine adhesions and pregnancy success rates after treatment: Comparison of adhesions obtained from open myomectomy versus uterine curettage. Afr J Reprod Health. 2022;26(12):90-96. [4] YONG J, WAN Y, YE M, et al. Comparative analysis of the clinical efficacy and reproductive outcomes of the hysteroscopic tissue removal system (MyoSure) and hysteroscopic electroresection in the treatment of benign intrauterine lesions. Int J Gynaecol Obstet. 2023;163(1):115-122. [5] SCHAUB AM, PISARSKA MD, WRIGHT KN. Intrauterine Adhesions After Chlamydia Infection With a Levonorgestrel-Releasing Intrauterine Device in Place. Obstet Gynecol. 2021;138(3):478-481. [6] JIN X, YE J, ZHANG L, et al. Efficacy of hysteroscopic cold knife separation on intrauterine adhesions. Am J Transl Res. 2021;13(7): 8351-8357. [7] WANG S, DUAN H, LI B, et al. Efficacy of Freeze-Dried Amnion Grafts on Cytokines in Uterine Exudates Following Hysteroscopic Adhesiolysis of Severe Intrauterine Adhesions. Int J Gen Med. 2022; 15:1703-1713. [8] ZHOU R, ZHANG X, DONG M, et al. Association between endogenous LH level prior to progesterone administration and live birth rate in artificial frozen-thawed blastocyst transfer cycles of ovulatory women. Hum Reprod. 2021;36(10):2687-2696. [9] VITALE SG, RIEMMA G, CARUGNO J, et al. Postsurgical barrier strategies to avoid the recurrence of intrauterine adhesion formation after hysteroscopic adhesiolysis: a network meta-analysis of randomized controlled trials. Am J Obstet Gynecol. 2022;226(4):487-498.e8. [10] XIE X, XU R, OUYANG H, et al. A mechanically robust and stable estradiol-loaded PHEMA-based hydrogel barrier for intrauterine adhesion treatment. J Mater Chem B. 2022;10(42):8684-8695. [11] LIU F, HU S, YANG H, et al. Hyaluronic Acid Hydrogel Integrated with Mesenchymal Stem Cell-Secretome to Treat Endometrial Injury in a Rat Model of Asherman’s Syndrome. Adv Healthc Mater. 2019;8(14):e1900411. [12] XIONG Z, MA Y, HE J, et al. Apoptotic bodies of bone marrow mesenchymal stem cells inhibit endometrial stromal cell fibrosis by mediating the Wnt/beta-catenin signaling pathway. Heliyon. 2023; 9(11):e20716. [13] WANG G, REN C, JIANG J. Effects of bone marrow mesenchymal stem cells on repair and receptivity of damaged endometrium in rats. J Obstet Gynaecol Res. 2021;47(9):3223-3231. [14] WANG Y, SUN X, YANG Q, et al. Exosomes from bone mesenchymal stem cells alleviate mifepristone-induced human endometrial stromal cell injury by inhibiting TLR3 via delivering miR-941. Physiol Int. 2022; 109(4):443-456. [15] JO H, BRITO S, KWAK BM, et al. Applications of Mesenchymal Stem Cells in Skin Regeneration and Rejuvenation. Int J Mol Sci. 2021; 22(5):2410. [16] POMATTO M, GAI C, NEGRO F, et al. Differential Therapeutic Effect of Extracellular Vesicles Derived by Bone Marrow and Adipose Mesenchymal Stem Cells on Wound Healing of Diabetic Ulcers and Correlation to Their Cargoes. Int J Mol Sci. 2021;22(8):3851. [17] LU Y, LI J, HOU N, et al. Decellularized tympanic membrane scaffold with bone marrow mesenchymal stem cells for repairing tympanic membrane perforation. Artif Organs. 2023;47(1):62-76. [18] MACHADO-PAULA MM, CORAT MAF, DE VASCONCELLOS LMR, et al. Rotary Jet-Spun Polycaprolactone/Hydroxyapatite and Carbon Nanotube Scaffolds Seeded with Bone Marrow Mesenchymal Stem Cells Increase Bone Neoformation. ACS Appl Bio Mater. 2022;5(3): 1013-1024. [19] GUAN Y, YANG B, XU W, et al. Cell-Derived Extracellular Matrix Materials for Tissue Engineering. Tissue Eng Part B Rev. 2022;28(5): 1007-1021. [20] WU J, PAN Z, ZHAO ZY, et al. Anti-Swelling, Robust, and Adhesive Extracellular Matrix-Mimicking Hydrogel Used as Intraoral Dressing. Adv Mater. 2022;34(20):e2200115. [21] SMITH MJ, DEMPSEY SG, VEALE RW, et al. Further structural characterization of ovine forestomach matrix and multi-layered extracellular matrix composites for soft tissue repair. J Biomater Appl. 2022;36(6):996-1010. [22] LACORZANA J. Amniotic membrane, clinical applications and tissue engineering. Review of its ophthalmic use. Arch Soc Esp Oftalmol(Engl Ed). 2020;95(1):15-23. [23] CHEN P, LU M, WANG T, et al. Human amniotic membrane as a delivery vehicle for stem cell-based therapies. Life Sci. 2021;272: 119157. [24] CHEN X, ZHOU Y, SUN Y, et al. Transplantation of decellularized and lyophilized amniotic membrane inhibits endometrial fibrosis by regulating connective tissue growth factor and tissue inhibitor of matrix metalloproteinase-2. Exp Ther Med. 2021;22(3):968. [25] ZHANG H, ZHANG Q, ZHANG J, et al. Urinary bladder matrix scaffolds improve endometrial regeneration in a rat model of intrauterine adhesions. Biomater Sci. 2020;8(3):988-996. [26] FU X, LIAN Q, ZHANG B, et al. Scanning Probe Microscopy Bone Marrow Determination of Steogenic Differentiation of Mesenchymal Stem Cells. Contrast Media Mol Imaging. 2022;2022:6483087 [27] LEE WL, LIU CH, CHENG M, et al. Focus on the Primary Prevention of Intrauterine Adhesions: Current Concept and Vision. Int J Mol Sci. 2021;22(10):5175. [28] XIN L, WEI C, TONG X, et al. In situ delivery of apoptotic bodies derived from mesenchymal stem cells via a hyaluronic acid hydrogel: A therapy for intrauterine adhesions. Bioact Mater. 2021;12:107-119. [29] YUAN L, CAO J, HU M, et al. Bone marrow mesenchymal stem cells combined with estrogen synergistically promote endometrial regeneration and reverse EMT via Wnt/beta-catenin signaling pathway. Reprod Biol Endocrinol. 2022;20(1):121. [30] JIANG P, TANG X, WANG H, et al. Collagen-binding basic fibroblast growth factor improves functional remodeling of scarred endometrium in uterine infertile women: a pilot study. Sci China Life Sci. 2019;62(12): 1617-1629. [31] GOLKAR S, CHEKINI Z, AMJADi F, et al. Expressions of vascular endothelial growth factor A, mucin-1, colony-stimulating factor-1, heparin-binding epidermal growth factor-like growth factor, and fibroblast growth factor 2 genes in the female reproductive tracts of women with ectopic pregnancy: A case-control study. Int J Reprod Biomed. 2023;21(10):801-808. [32] RUTANEN EM. Insulin-like growth factors and insulin-like growth factor binding proteins in the endometrium. Effect of intrauterine levonorgestrel delivery. Hum Reprod. 2000;15 Suppl 3:173-81. [33] GUPTA MB, BIGGAR KK, LI C, et al.Increased Colocalization and Interaction Between Decidual Protein Kinase A and Insulin-like Growth Factor-Binding Protein-1 in Intrauterine Growth Restriction. J Histochem Cytochem. 2022;70(7):515-530. [34] ROCHA CC, SILVA FAC, MARTINS T, et al. Culture of endometrial epithelial cells collected by a cytological brush in vivo. JDS Commun. 2022;3(3):217-221. [35] XIE Y, KONG W, ZHAO X, et al. Metformin Inhibits the Estrogen-mediated Epithelial-Mesenchymal Transition of Ectopic Endometrial Stromal Cells in Endometriosis. In Vivo. 2023;37(6):2490-2497. [36] ZHANG H, QI S, LIU Z, et al. Melatonin Inhibits 17beta-Estradiol-Induced Epithelial-Mesenchymal Transition in Endometrial Adenocarcinoma Cells via Upregulating Numb Expression. Gynecol Obstet Invest. 2022; 87(2):89-99. [37] BENJAMIN K, MARQUEZ CM, MORTA M, et al. Bisphenol S Increases Cell Number and Stimulates Migration of Endometrial Epithelial Cells. J ASEAN Fed Endocr Soc. 2023;38(1):13-22. |
| [1] | Liu Qi, Li Linzhen, Li Yusheng, Jiao Hongzhuo, Yang Cheng, Zhang Juntao. Icariin-containing serum promotes chondrocyte proliferation and chondrogenic differentiation of stem cells in the co-culture system of three kinds of cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1371-1379. |
| [2] | Zhang Zhenyu, Liang Qiujian, Yang Jun, Wei Xiangyu, Jiang Jie, Huang Linke, Tan Zhen. Target of neohesperidin in treatment of osteoporosis and its effect on osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1437-1447. |
| [3] | Yang Zhihang, Sun Zuyan, Huang Wenliang, Wan Yu, Chen Shida, Deng Jiang. Nerve growth factor promotes chondrogenic differentiation and inhibits hypertrophic differentiation of rabbit bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1336-1342. |
| [4] | Sun Xianjuan, Wang Qiuhua, Zhang Jinyi, Yang Yangyang, Wang Wenshuang, Zhang Xiaoqing. Adhesion, proliferation, and vascular smooth muscle differentiation of bone marrow mesenchymal stem cells on different electrospinning membranes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 661-669. |
| [5] | Ge Xiao, Zhao Zhuangzhuang, Guo Shuyu, Xu Rongyao. HOXA10 gene-modified bone marrow mesenchymal stem cells promote bone regeneration [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7701-7708. |
| [6] | Zhang Xiongjinfu, Chen Yida, Cheng Xinyi, Liu Daihui, Shi Qin . Exosomes derived from bone marrow mesenchymal stem cells of young rats to reverse senescence in aged rat bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7709-7718. |
| [7] | Sima Xinli, Liu Danping, Qi Hui. Effect and mechanism of metformin-modified bone marrow mesenchymal stem cell exosomes on regulating chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7728-7734. |
| [8] | Liu Chengyuan, Guo Qianping. Differential effects of kartogenin on chondrogenic and osteogenic differentiation of rat and rabbit bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7490-7498. |
| [9] | Liu Xun, Ouyang Hougan, Pan Rongbin, Wang Zi, Yang Fen, Tian Jiaxuan . Optimal parameters for physical interventions in bone marrow mesenchymal stem cell differentiation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6727-6732. |
| [10] | Zhao Yihan, Sun Xuhang, Zhao Lin, Jiang Shiqing. Effects and mechanisms of exosomal miRNA in treatment of multiple myeloma [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6743-6752. |
| [11] | Xiong Zhenghua, Zhou Jianghong, Shen Yi, Han Xuesong . Mesenchymal stem cells and extracellular vesicles in repair of endometrial injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6782-6791. |
| [12] | Zhong Min, Wang Cheng, Fan Zhenhai, Li Linyan, Yu Limei. Effect and mechanism of perinatal mesenchymal stem cells and their combination with hydrogels in treatment of intrauterine adhesions [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6792-6799. |
| [13] | Shao Xuekun, Shi Dianhua, Ding Zhiping, Qiu Zhuoya, Wang Ping, Wang Yi, Wang Cheng, Ding Xiaoyan, Sun Tiefeng. Calcined deer antler slices promote proliferation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6601-6608. |
| [14] | Lin Shuqian, Zhao Xilong, Gao Jing, Pan Xinghua, Li Zian, Ruan Guangping. Comparison of biological characteristics of mouse bone marrow mesenchymal stem cells after interference and overexpression of telomere Cajal body protein-1 [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6616-6624. |
| [15] | Liang Zhifeng, Yang Yingcai, Cheng Qiangang, Jia Yongxing, Wang Bo . Effect of stromal cell-derived factor-1 in cartilage and subchondral bone homeostasis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(25): 5422-5433. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||