Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (10): 1586-1591.doi: 10.12307/2024.364
Previous Articles Next Articles
Influence of bone cement volume and distribution on surgical and adjacent vertebral refractures after percutaneous vertebroplasty
Abuduwupuer•Haibier, Alimujiang•Yusufu, Maimaitimin•Abulimiti, Maihemuti•Yakufu, Aiben•Kayierhan, Yimuran•Abudukelimu, Alimujiang•Aximu, Lin Hang, Tuerhongjiang•Abudurexiti
- Sixth Affiliated Hospital, Xinjiang Medical University, Urumqi 830002, Xinjiang Uygur Autonomous Region, China
-
Received:2023-04-12Accepted:2023-05-19Online:2024-04-08Published:2023-08-19 -
Contact:Tuerhongjiang•Abudurexiti, Master, Chief physician, Master’s supervisor, Sixth Affiliated Hospital, Xinjiang Medical University, Urumqi 830002, Xinjiang Uygur Autonomous Region, China Maihemuti•Yakufu, Sixth Affiliated Hospital, Xinjiang Medical University, Urumqi 830002, Xinjiang Uygur Autonomous Region, China -
About author:Abuduwupuer•Haibier, Master candidate, Sixth Affiliated Hospital, Xinjiang Medical University, Urumqi 830002, Xinjiang Uygur Autonomous Region, China -
Supported by:Natural Science Foundation Youth Project of Science and Technology Department of Xinjiang Uygur Autonomous Region, No. 2022D01C821 (to MY)
CLC Number:
Cite this article
Abuduwupuer•Haibier, Alimujiang•Yusufu, Maimaitimin•Abulimiti, Maihemuti•Yakufu, Aiben•Kayierhan, Yimuran•Abudukelimu, Alimujiang•Aximu, Lin Hang, Tuerhongjiang•Abudurexiti. Influence of bone cement volume and distribution on surgical and adjacent vertebral refractures after percutaneous vertebroplasty[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(10): 1586-1591.
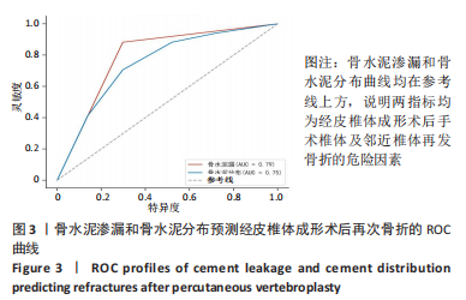
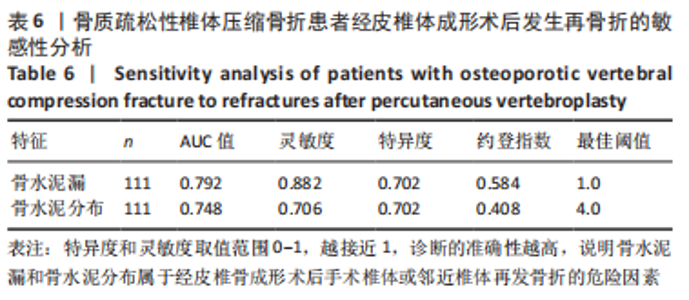
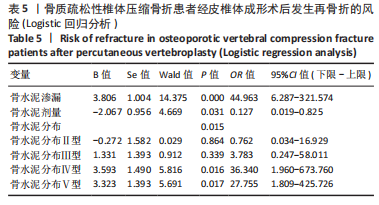
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

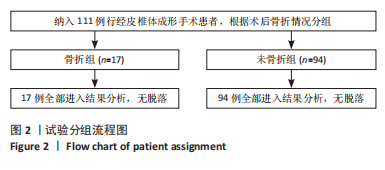
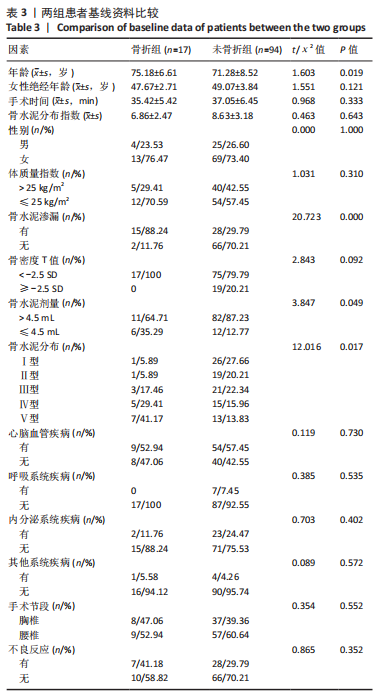
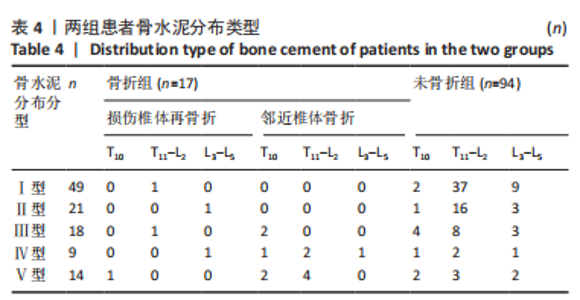
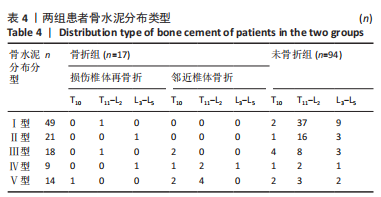
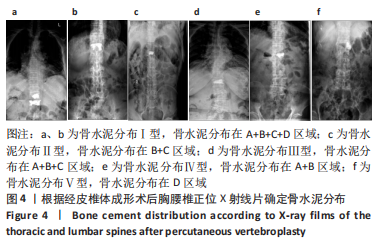
111例患者中,5例发生手术椎体再骨折,12例发生邻近椎体骨折;骨水泥分布Ⅰ型和Ⅱ型患者中再发生骨折均1例(5.89%),骨水泥分布Ⅲ型患者中再发生骨折3例(17.46%)、骨水泥分布Ⅳ型患者中再发生骨折5例(29.41%)、骨水泥分布Ⅴ型患者中再发生骨折7例(41.17%)。 2.4 二元Logistic回归分析结果 根据两组间单因素分析结果,所有有统计学意义的变量(骨水泥渗漏、骨水泥剂量、骨水泥分布位置)均纳入二元Logistic回归分析,见表5。在这些变量中,骨水泥渗漏(P=0.000)、骨水泥剂量(P=0.031)和骨水泥分布(P=0.015)为手术椎体及邻近椎体再发骨折的危险因素,见图3和表6,与骨水泥分布Ⅰ型、Ⅱ型和Ⅲ型患者相比,骨水泥分布Ⅳ型(OR=36.340,P=0.016)和骨水泥分布Ⅴ型(OR=27.755,P=0.017)的手术椎体及邻近椎体再发骨折风险较高。"
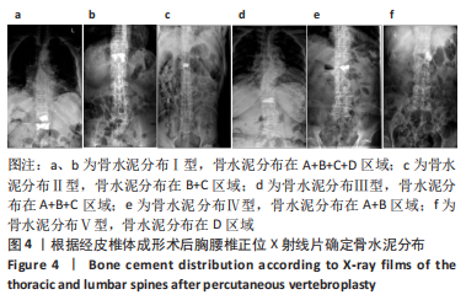
2.5 典型病例 73岁女性T12椎体压缩性骨折患者,经皮椎体成形术后正位X线射线片显示骨水泥分布在A+B+C+D区域,见图4a;79岁男性L1椎体压缩性骨折患者,经皮椎体成形术后正位X线射线片显示骨水泥分布在A+B+C+D区域,见图4b;68岁男性L1椎体压缩性骨折患者,经皮椎体成形术后正位X线射线片显示骨水泥分布在B+C区域,见图4c;82岁女性T11椎体压缩性骨折患者,经皮椎体成形术后正位X线射线片显示骨水泥分布在A+B+C区域,见图4d;81岁男性L1椎体压缩性骨折患者,经皮椎体成形术后正位X线射线片显示骨水泥分布在A+B区域,见图4e;84岁女性L2椎体压缩性骨折患者,经皮椎体成形术后正位X线射线片显示骨水泥分布在D区域,见图4f。"
| [1] LIANG L, CHEN X, JIANG W, et al. Balloon kyphoplasty or percutaneous vertebroplasty for osteoporotic vertebral compression fracture? An updated systematic review and meta-analysis. Ann Saudi Med. 2016;36(3):165-174. [2] PARREIRA PCS, MAHER CG, MEGALE RZ, et al. An overview of clinical guidelines for the management of vertebral compression fracture: a systematic review. Spine J. 2017;17(12):1932-1938. [3] LIN J, QIAN L, JIANG C, et al. Bone cement distribution is a potential predictor to the reconstructive effects of unilateral percutaneous kyphoplasty in OVCFs: a retrospective study. J Orthop Surg Res. 2018;13(1):140. [4] ZHOU C, HUANG S, LIAO Y, et al. Correlation analysis of larger side bone cement volume/vertebral body volume ratio with adjacent vertebral compression fractures during vertebroplasty. Front Endocrinol (Lausanne). 2023;14:1072087. [5] SANLI I, VAN KUIJK SMJ, DE BIE RA, et al. Percutaneous cement augmentation in the treatment of osteoporotic vertebral fractures (OVFs) in the elderly: a systematic review. Eur Spine J. 2020;29(7):1553-1572. [6] 孙育良,熊小明,何本祥,等.椎体成形骨填充材料的研究与现状[J].中国组织工程研究,2017,21(14):2285-2290. [7] LI X, LU Y, LIN X. Refracture of osteoporotic vertebral body after treatment by balloon kyphoplasty: Three cases report. Medicine (Baltimore). 2017; 96(49):e8961. [8] 沈松,徐彬.经皮椎体成形骨水泥呈弥散型分布可减少邻近椎体再骨折的发生率[J].中国组织工程研究,2022,26(4):499-503. [9] CLARK W, BIRD P, GONSKI P, et al. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2016;388(10052):1408-1416. [10] WANG Y, LIU B, SUN Z, et al. Comparative Efficacy of Three Minimally Invasive Procedures for Kümmell’s Disease: A Systematic Review and Network Meta-Analysis. Front Surg. 2022;9:893404. [11] LV B, JI P, FAN X, et al. Clinical Efficacy of Different Bone Cement Distribution Patterns in Percutaneous Kyphoplasty: A Retrospective Study. Pain Physician. 2020;23(4):E409-e416. [12] LI Q, LONG X, WANG Y, et al. Clinical observation of two bone cement distribution modes after percutaneous vertebroplasty for osteoporotic vertebral compression fractures. BMC Musculoskelet Disord. 2021;22(1): 577. [13] LI K, JI C, LUO D, et al. Role of percutaneous vertebroplasty with high-viscosity cement in the treatment of severe osteoporotic vertebral compression fractures. Sci Rep. 2021;11(1):4602. [14] GAUGHEN JR JR, JENSEN ME, SCHWEICKERT PA, et al. The therapeutic benefit of repeat percutaneous vertebroplasty at previously treated vertebral levels. AJNR Am J Neuroradiol. 2002;23(10):1657-1661. [15] ZHANG L, WANG Q, WANG L, et al. Bone cement distribution in the vertebral body affects chances of recompression after percutaneous vertebroplasty treatment in elderly patients with osteoporotic vertebral compression fractures. Clin Interv Aging. 2017;12:431-436. [16] RHO YJ, CHOE WJ, CHUN YI. Risk factors predicting the new symptomatic vertebral compression fractures after percutaneous vertebroplasty or kyphoplasty. Eur Spine J. 2012;21(5):905-911. [17] KOMEMUSHI A, TANIGAWA N, KARIYA S, et al. Percutaneous vertebroplasty for osteoporotic compression fracture: multivariate study of predictors of new vertebral body fracture. Cardiovasc Intervent Radiol. 2006;29(4):580-585. [18] MARTIKOS K, GREGGI T, FALDINI C, et al. Osteoporotic thoracolumbar compression fractures: long-term retrospective comparison between vertebroplasty and conservative treatment. Eur Spine J. 2018;27(Suppl 2): 244-247. [19] BAEK S W, KIM C, CHANG H. The relationship between the spinopelvic balance and the incidence of adjacent vertebral fractures following percutaneous vertebroplasty. Osteoporos Int. 2015;26(5):1507-1513. [20] NING L, WAN S, LIU C, et al. New Levels of Vertebral Compression Fractures after Percutaneous Kyphoplasty: Retrospective Analysis of Styles and Risk Factors. Pain Physician. 2015;18(6):565-572. [21] YI X, LU H, TIAN F, et al. Recompression in new levels after percutaneous vertebroplasty and kyphoplasty compared with conservative treatment. Arch Orthop Trauma Surg. 2014;134(1):21-30. [22] YANG W, YANG J, LIANG M. Percutaneous Vertebroplasty Does Not Increase the Incidence of New Fractures in Adjacent and Nonadjacent Vertebral Bodies. Clin Spine Surg. 2019;32(2):E99-e106. [23] KLAZEN CA, VENMANS A, DE VRIES J, et al. Percutaneous vertebroplasty is not a risk factor for new osteoporotic compression fractures: results from VERTOS II. AJNR Am J Neuroradiol. 2010;31(8):1447-1450. [24] CHEVALIER Y, PAHR D, CHARLEBOIS M, et al. Cement distribution, volume, and compliance in vertebroplasty: some answers from an anatomy-based nonlinear finite element study. Spine (Phila Pa 1976). 2008;33(16):1722-1730. [25] CHEN B, LI Y, XIE D, et al. Comparison of unipedicular and bipedicular kyphoplasty on the stiffness and biomechanical balance of compression fractured vertebrae. Eur Spine J. 2011;20(8):1272-1280. [26] 刘群,孙东东,高丽兰,等.经皮椎体后凸成形后再发骨折相关因素的Meta分析[J].中国组织工程研究,2020,24(6):976-984. [27] LIANG X, ZHONG W, LUO X, et al. Risk factors of adjacent segmental fractures when percutaneous vertebroplasty is performed for the treatment of osteoporotic thoracolumbar fractures. Sci Rep. 2020;10(1):399. [28] ZHANG Z, FAN J, DING Q, et al. Risk factors for new osteoporotic vertebral compression fractures after vertebroplasty: a systematic review and meta-analysis. J Spinal Disord Tech. 2013;26(4):E150-157. [29] 吕文,刘艺明,陈光,等.经横突根部单侧穿刺的改良PVP与PCVP技术治疗腰椎骨质疏松性骨折的疗效对比[J].颈腰痛杂志,2020,41(2):154-157. [30] 崔志远,毛兆虎,刘玉林,等.单侧PVP术对OVCF术后椎体高度恢复及疼痛程度的效果研究[J].中国医药导报,2021,18(18):92-95. [31] 罗伟斌,林勇,孙春喜,等.经皮椎体成形术术后新发椎体骨折特点及危险因素分析[J].中国医药科学,2021,11(10):210-212,224. [32] WANG D, LI Y, YIN H, et al. Three-dimensional finite element analysis of optimal distribution model of vertebroplasty. Ann Palliat Med. 2020;9(3): 1062-1072. [33] GOLDSTEIN CL, CHUTKAN NB, CHOMA TJ, et al. Management of the Elderly With Vertebral Compression Fractures. Neurosurgery. 2015;77 Suppl 4:S33-45. [34] CHEN XS, JIANG JM, SUN PD, et al. How the clinical dosage of bone cement biomechanically affects adjacent vertebrae. J Orthop Surg Res. 2020;15(1): 370. [35] MOLLOY S, MATHIS JM, BELKOFF SM. The effect of vertebral body percentage fill on mechanical behavior during percutaneous vertebroplasty. Spine (Phila Pa 1976). 2003;28(14):1549-1554. [36] NIU J, ZHOU H, MENG Q, et al. Factors affecting recompression of augmented vertebrae after successful percutaneous balloon kyphoplasty: a retrospective analysis. Acta Radiol. 2015;56(11):1380-1387. [37] HOU Y, YAO Q, ZHANG G, et al. Polymethylmethacrylate distribution is associated with recompression after vertebroplasty or kyphoplasty for osteoporotic vertebral compression fractures: A retrospective study. PLoS One. 2018;13(6):e0198407. [38] MA X, XING D, MA J, et al. Risk factors for new vertebral compression fractures after percutaneous vertebroplasty: qualitative evidence synthesized from a systematic review. Spine (Phila Pa 1976). 2013;38(12): E713-722. [39] LI YX, GUO DQ, ZHANG SC, et al. Risk factor analysis for re-collapse of cemented vertebrae after percutaneous vertebroplasty (PVP) or percutaneous kyphoplasty (PKP). Int Orthop. 2018;42(9):2131-2139. |
| [1] | Xi Jintao, Lu Qilin, Wang Yang, Wang Xiaojuan, Lyu Peng, Chen Long, Shi Zhen, Xie Wei, Zhu Yiliang, Li Xugui. Risk factors for cage retropulsion following transforaminal lumbar interbody fusion [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1394-1398. |
| [2] | Yang Cekai, Cai Zhuoyan, Chen Ming, Liu Hao, Weng Rui, Cui Jianchao, Zhang Shuncong, Yao Zhensong. Relationship between degeneration of paraspinal muscle and refractures in postmenopausal women treated by percutaneous vertebroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1414-1419. |
| [3] | Han Bing, Liu Hongbin, Wang Hehong, Zhao Hanqing, Zhao Riguang, Sun Yiyan, Zhang Yu. Correlation between lower limb alignment and risk factors of patellofemoral pain syndrome in young men [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1211-1216. |
| [4] | Tong Yibo, Li Minghui. Influencing factors of adjacent vertebral re-fracture in patients with osteoporotic vertebral fractures after percutaneous vertebroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1241-1246. |
| [5] | Wang Ji, Hu Li, Yang Zhongya, Han Peng. A cross-sectional survey on the prevalence and risk factors of sarcopenia in the elderly in some areas of the Yunnan-Guizhou Plateau [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(14): 2197-2201. |
| [6] | Liu Guangluan, Guo Zonglei, Ge Jin, Huang Dong, Wang Yehua. Anatomic risk factors for medial meniscus posterior root tears combined with anterior cruciate ligament injuries [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(5): 663-668. |
| [7] | Shen Lianwei, Zhu Hongliu, Wang Wei. Risk factor analysis of metabolic syndrome and construction of a nomogram prediction model in middle-aged and elderly people [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(5): 657-662. |
| [8] | Lu Zhaohua, Sun Tianze, Zhang Jing, Zhang Wentao, Yang Ming, Li Zhonghai. Kyphoplasty via different approaches for osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(36): 5834-5839. |
| [9] | Yu Jian, Zhou Bingqian, Wang Zhao, Li Yue, Chang Yaru, Cao Hong. Comparison of random forest model and logistic regression model in predicting the prolonged length of stay of hip fracture patients [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(34): 5413-5420. |
| [10] | Liu Jin, Xia Bin, Cai Peng, Gu Zuchao, Yang Haosen, Tang Jing. Effect of vertebral augmentation using quantitative computed tomography-based finite element analysis on biomechanical parameters of non-enhanced vertebrae in different locations [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(34): 5436-5440. |
| [11] | Meng Xiangli, Lyu Xiaohong. Effects of eccentric exercise patterns on exercise-induced muscle damage [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(32): 5132-5136. |
| [12] | Sun Lingjuan, Song Xizheng, Li Daming, Han Zhenxue, Kang Yu, Xiang Hanrui, Sheng Kai. Percutaneous vertebroplasty under distraction with external spinal fixator for vertebral osteoporotic compression fractures with posterior wall damage [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(31): 4954-4958. |
| [13] | Yuan Haibo, Li Dongya, Pan Bin, Guan Kai, Chen Feng, Yuan Feng, Wu Jibin. Sagittal related factors of upper lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(31): 4984-4989. |
| [14] | Guan Jianbin, Feng Ningning, Yu Xing, Liu Tao, Jiang Guozheng, Yang Yongdong, Zhao He. Correlation between CT value of vertebral body partition and bone cement distribution after percutaneous vertebroplasty [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(30): 4757-4762. |
| [15] | Wang Kaiyu, Hu Peng, Wei Zairong, Huang Guangtao, Zhou Jian, He Guijia, Nie Kaiyu. Use of expanders and implants in breast reconstruction complicated with infection [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 461-469. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||