Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (33): 5323-5328.doi: 10.12307/2022.724
Previous Articles Next Articles
A machine learning prediction model based on MRI radiomics for refracture of thoracolumbar segments
Liu Jin1, 2, Yin Hongkun3, Chen Guo2, Zhang Yu2, Gu Zuchao2, Tang Jing4
- 1Department of Orthopedics, Chengdu Seventh People’s Hospital, Chengdu 610041, Sichuan Province, China; 2Department of Orthopedics, Chengdu First People’s Hospital, Chengdu 610041, Sichuan Province, China; 3Beijing Infervision Technology Co., Ltd., Beijing 100080, China; 4Department of Radiology, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China
-
Received:2021-09-06Accepted:2021-10-28Online:2022-11-28Published:2022-03-31 -
Contact:Tang Jing, MD, Associate chief physician, Department of Radiology, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China -
About author:Liu Jin, MD, Attending physician, Department of Orthopedics, Chengdu Seventh People’s Hospital, Chengdu 610041, Sichuan Province, China; Department of Orthopedics, Chengdu First People’s Hospital, Chengdu 610041, Sichuan Province, China -
Supported by:Scientific Research Project of Sichuan Provincial Health Commission, No. 20PJ194 (to LJ); Scientific Research Project of Chengdu Municipal Health Commission, No. 2020133 (to LJ)
CLC Number:
Cite this article
Liu Jin, Yin Hongkun, Chen Guo, Zhang Yu, Gu Zuchao, Tang Jing. A machine learning prediction model based on MRI radiomics for refracture of thoracolumbar segments[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(33): 5323-5328.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
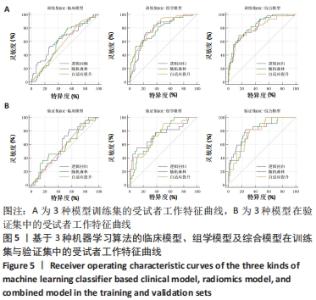
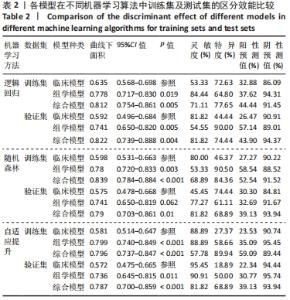
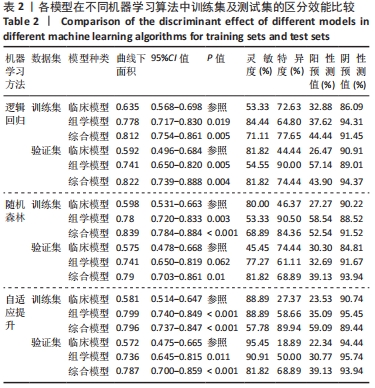
2.5 预测模型构建及效能比较 对于采用135例患者的性别、年龄及节段构建的临床模型,在训练集中,逻辑回归算法、随机森林算法及自适应提升算法中的曲线下面积分别为0.635,0.598,0.581;在验证集中,逻辑回归算法、随机森林算法及自适应提升算法中的曲线下面积分别为0.592,0.575,0.572。对于采用13个组学特征的组学模型,在训练集中,逻辑回归算法、随机森林算法及自适应提升算法中的曲线下面积分别为0.778,0.780及0.799;在验证集中,逻辑回归算法、随机森林算法及自适应提升算法中的曲线下面积分别为0.741,0.741及0.736。对于综合组学特征及临床特征构建的综合模型,在训练集中,逻辑回归算法、随机森林算法及自适应提升算法中的曲线下面积分别为0.812,0.839,0.796;在验证集中,逻辑回归算法、随机森林算法及自适应提升算法中的曲线下面积分别为0.822,0.790,0.787。各模型受试者工作特征曲线见图5,曲线下面积最佳值及对应的95%CI值、敏感度、特异度、阳性预测值和阴性预测值,见表2。"
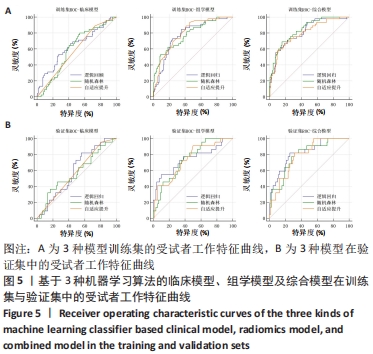
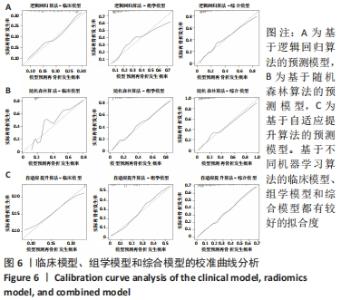
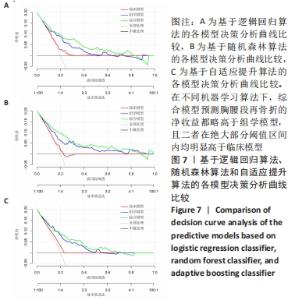
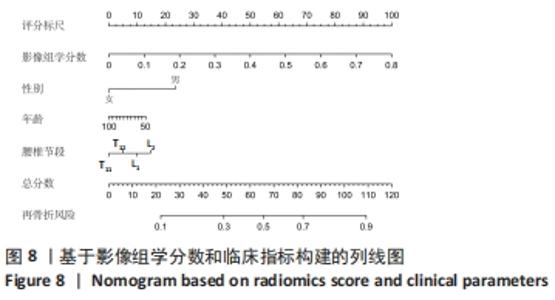
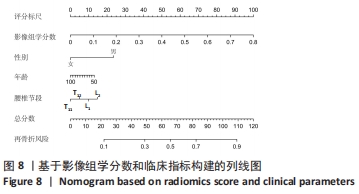
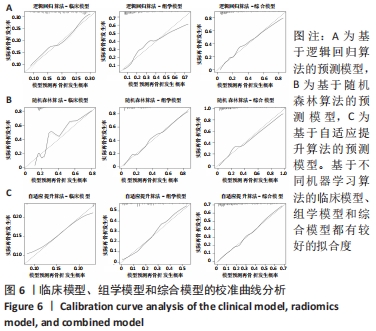
在3种机器学习算法比较上,临床模型、组学模型及综合模型各自训练集、验证集曲线下面积比较差异均无显著性意义(P > 0.05)。在3种模型比较上,Delong test检验表明,综合模型在3种算法下各曲线下面积均显著高于临床模型(P < 0.05);组学模型除随机森林算法验证集曲线下面积与临床模型比较差异无显著性意义(P=0.062)外,其余算法下各曲线下面积均显著高于临床模型(P < 0.05);综合模型各曲线下面积虽然略高于组学模型,差异无显著性意义(P > 0.05)。 校准曲线表明,基于不同机器学习算法的临床模型、组学模型和综合模型都有较好的拟合度,见图6。决策分析曲线表明,在不同机器学习算法下,综合模型预测胸腰段再骨折的净收益都略高于组学模型,且二者在绝大部分阈值区间内均明显高于临床模型,见图7。最后,基于逻辑回归算法的组学模型计算得到了每个椎体影像组学分数,并结合患者的性别、年龄和节段信息构建了列线图,见图8。"
| [1] EDIDIN AA, ONG KL, LAU E, et al. Morbidity and Mortality After Vertebral Fractures: Comparison of Vertebral Augmentation and Nonoperative Management in the Medicare Population. Spine (Phila Pa 1976). 2015;40:1228-1241. [2] HINDE K, MAINGARD J, HIRSCH JA, et al. Mortality Outcomes of Vertebral Augmentation (Vertebroplasty and/or Balloon Kyphoplasty) for Osteoporotic Vertebral Compression Fractures: A Systematic Review and Meta-Analysis. Radiology. 2020;295:96-103. [3] CLARK W, BIRD P, GONSKI P, et al. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2016;388: 1408-1416. [4] 张嘉.骨质疏松性椎体压缩骨折的微创强化治疗[J].中华骨与关节外科杂志,2021,14(5):350-354. [5] LOU S, SHI X, ZHANG X, et al. Percutaneous vertebroplasty versus non-operative treatment for osteoporotic vertebral compression fractures: a meta-analysis of randomized controlled trials. Osteoporos Int. 2019; 30:2369-2380. [6] HAN SL, WAN SL, LI QT, et al. Is vertebroplasty a risk factor for subsequent vertebral fracture, meta-analysis of published evidence? Osteoporos Int. 2015;26:113-122. [7] ZHANG H, XU CY, ZHANG TX, et al. Does Percutaneous Vertebroplasty or Balloon Kyphoplasty for Osteoporotic Vertebral Compression Fractures Increase the Incidence of New Vertebral Fractures? A Meta-Analysis. Pain Physician. 2017;20:E13-E28. [8] 庞巨涛,张新虎,孙建华,等.经皮球囊扩张椎体后凸成形后椎体再骨折的危险:回顾性多因素分析[J].中国组织工程研究,2019, 23(8):1182-1187. [9] LAMBIN P, RIOS-VELAZQUEZ E, LEIJENAAR R, et al. Radiomics: extracting more information from medical images using advanced feature analysis. Eur J Cancer. 2012;48(4):441-446. [10] 胡杉,梁长虹,刘再毅,等.纹理分析及影像组学在非肿瘤病变的研究应用及进展[J].中华放射学杂志,2019,53(6):526-529. [11] SONG J, SHI J, DONG D, et al. A New Approach to Predict Progression-free Survival in Stage IV EGFR-mutant NSCLC Patients with EGFR-TKI Therapy. Clin Cancer Res. 2018;24(15):3583-3592. [12] HUANG Y, LIU Z, HE L, et al. Radiomics Signature: A Potential Biomarker for the Prediction of Disease-Free Survival in Early-Stage (I or II) Non-Small Cell Lung Cancer. Radiology. 2016;281(3):947-957. [13] MUEHLEMATTER UJ, MANNIL M, BECKER AS, et al. Vertebral body insufficiency fractures: detection of vertebrae at risk on standard CT images using texture analysis and machine learning. Eur Radiol. 2019;29(5):2207-2217. [14] ARPITHA A, RANGARAJAN L. Computational techniques to segment and classify lumbar compression fractures. Radiol Med. 2020;125(6):551-560. [15] ZAIA A, ROSSI R, GALEAZZI R, et al. Fractal lacunarity of trabecular bone in vertebral MRI to predict osteoporotic fracture risk in over-fifties women. The LOTO study. BMC Musculoskelet Disord. 2021;22(1):108. [16] FERIZI U, HONIG S, CHANG G. Artificial intelligence, osteoporosis and fragility fractures. Curr Opin Rheumatol. 2019;31(4):368-375. [17] LIU J, TANG J, GU ZC, et al. Fracture-free probability and predictors of new symptomatic fractures in sandwich, ordinary-adjacent, and non-adjacent vertebrae: a vertebra-specific survival analysis. J Neurointerv Surg. 2021;13(11):1058-1062. [18] BOUSSON V, BERGOT C, SUTTER B, et al. Trabecular bone score (TBS): available knowledge, clinical relevance, and future prospects. Osteoporos Int. 2012;23(5):1489-1501. [19] FERIZI U, BESSER H, HYSI P, et al. Artificial Intelligence Applied to Osteoporosis: A Performance Comparison of Machine Learning Algorithms in Predicting Fragility Fractures From MRI Data. J Magn Reson Imaging. 2019;49(4):1029-1038. [20] BIVER E, DUROSIER-IZART C, CHEVALLEY T, et al. Evaluation of Radius Microstructure and Areal Bone Mineral Density Improves Fracture Prediction in Postmenopausal Women. J Bone Miner Res. 2018;33(2):328-337. [21] SAMELSON EJ, BROE KE, XU H, et al. Cortical and trabecular bone microarchitecture as an independent predictor of incident fracture risk in older women and men in the Bone Microarchitecture International Consortium (BoMIC): a prospective study. Lancet Diabetes Endocrinol. 2019;7(1):34-43. [22] LORENTZON M. The Importance and Possible Clinical Impact of Measuring Trabecular and Cortical Bone Microstructure to Improve Fracture Risk Prediction. J Bone Miner Res. 2020;35(5):831-832. [23] 李生鋆,范顺武,赵凤东.Micro-CT在椎体微结构扫描中的应用[J].中华骨科杂志,2016,36(4):241-247. [24] SHARMA AK, TOUSSAINT ND, ELDER GJ, et al. Magnetic resonance imaging based assessment of bone microstructure as a non-invasive alternative to histomorphometry in patients with chronic kidney disease. Bone. 2018;114:14-21. [25] MUSCHITZ C, KOCIJAN R, KOCIJAN R, et al. TBS reflects trabecular microarchitecture in premenopausal women and men with idiopathic osteoporosis and low-traumatic fractures. Bone. 2015;79:259-266. [26] LESLIE WD, SHEVROJA E, JOHANSSON H, et al. Risk-equivalent T-score adjustment for using lumbar spine trabecular bone score (TBS): the Manitoba BMD registry. Osteoporos Int. 2018;29(3):751-758. [27] 余卫,管文敏.腰椎骨小梁分数临床应用[J].中华骨质疏松和骨矿盐疾病杂志,2019,12(1):82-93. [28] POUILLÈS JM, GOSSET, A, GOSSET A, et al. TBS in early postmenopausal women with severe vertebral osteoporosis. Bone. 2021;142:115698. [29] MAZZETTI G, BERGER C, LESLIE WD, et al. Densitometer specific differences in the correlation between body mass index and lumbar spine trabecular bone score. J Clin Densitom. 2017;20:233-238. [30] BURIAN E, SUBBURAJ K, MOOKIAH MRK, et al. Texture analysis of vertebral bone marrow using chemical shift encoding-based water-fat MRI: a feasibility study. Osteoporos Int. 2019;30(6):1265-1274. [31] DIECKMEYER M, JUNKER D, JUNKER D, et al. Vertebral Bone Marrow Heterogeneity Using Texture Analysis of Chemical Shift Encoding-Based MRI: Variations in Age, Sex, and Anatomical Location. Front Endocrinol (Lausanne). 2020;11:555931. [32] NARDONE V, TINI P, CARBONE SF, et al. Bone texture analysis using CT-simulation scans to individuate risk parameters for radiation-induced insufficiency fractures. Osteoporos Int. 2017;28(6):1915-1923. [33] VOKES T, LAUDERDALE D, MA SL, et al. Radiographic Texture Analysis of Densitometric Calcaneal Images: Relationship to Clinical Characteristics and to Bone Fragility. J Bone Miner Res. 2010;25(1):56-63. |
| [1] | Yu Chengxiang, Liu Lehong, Li Wenbo, Chen Jinshi, Ran Chunlei, Wang Zhongping. Correlation between spine-pelvic sagittal parameters and prognosis of vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1412-1417. |
| [2] | Shen Song, Xu Bin. Diffuse distribution of bone cement in percutaneous vertebroplasty reduces the incidence of refracture of adjacent vertebral bodies [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 499-503. |
| [3] | Hou Wanxing, Li Hongwei, Zheng Xin, Zhu Xianren. Correlation between preoperative magnetic resonance imaging findings and bone cement leakage after percutaneous vertebral augmentation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 504-509. |
| [4] | Wang Zhiqiang, Lin Lu, Chen Xiaolin, Ke Zhenyong. Percutaneous vertebral augmentation for osteoporotic vertebral compression fractures: navigation, fracture reduction system, bone cement leakage, and material modification [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 631-636. |
| [5] | Li Youwen, Zheng Xingping, Zeng Jianhong, Chen Yu. Percutaneous kyphoplasty and percutaneous vertebroplasty for osteoporotic vertebral compression fractures: relationship of bone cement leakage with postoperative pain, Cobb angle of injured vertebrae, and gait recovery [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(28): 4494-4499. |
| [6] | Li Yang, Du Yibin, Liu Yiming, Li Fanjie. Risk factors of recurrent fracture after injection of calcium phosphate cement in kyphoplasty: advanced age and stress change [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(28): 4507-4513. |
| [7] | Xue Guang, Yang Xinming, Zhang Ying. Percutaneous vertebroplasty in treatment of osteoporotic vertebral compression fracture by two different approaches: bone cement leakage and safety [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(28): 4514-4518. |
| [8] | Ye Linqiang, Lu Guoliang, Jiang Xiaobing, Li Zhen, Weng Rui, Liang De, Huang Xuecheng, Feng Yonghong. Biomechanical effects of cement filling location on osteoporotic vertebral compression fracture: a three-dimensional finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(28): 4435-4440. |
| [9] | Li Shiwen, Xi Chunyang, Wang Xiaoyan, Chen Jianbai, You Changcheng, Qiao Wentao, Xu Gongping. Embedded percutaneous kyphoplasty and percutaneous vertebroplasty for treating post-traumatic vertebral osteonecrosis: finite element analysis of bone cement displacement [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(27): 4360-4366. |
| [10] | Wang Qian, Dong Junfeng. Influencing factors and precautions of new vertebral fractures after vertebroplasty for osteoporotic vertebral fractures [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(27): 4401-4405. |
| [11] | Yang Liu, Du Jianwei. Measures to reduce the leakage rate of bone cement during vertebral augmentation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(22): 3598-3601. |
| [12] | Wang Hailong, Li Long, Yilihamu Tuoheti, Liu Xu, Nacikedaoerji, Chen Hongtao, Cui Yong. Molecular network of miR-106b-5p regulating osteoporotic fracture in the elderly [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(2): 239-244. |
| [13] | Che Yanjun, Hu Dan, Si Weibing, Gu Xueping, Hao Yuefeng. Bone cement interval perfusion in hyperextension position for treatment of senile osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(10): 1483-1489. |
| [14] | Li Wenle, Wang Haosheng, Ning Lijun, Zhang Wenshi, Gao Sen, Sun Lijun, Hu Zhaohui. Analysis of the risk for bone cement leakage after percutaneous vertebroplasty in osteoporosis patients and model verification [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(10): 1477-1482. |
| [15] | Chen Chaofeng, He Dadong, Liang Jincheng, He Zhijun. Predicting the possibility of blood transfusion after total knee arthroplasty based on machine learning algorithm [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(36): 5792-5797. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||