Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (9): 1945-1952.doi: 10.12307/2025.280
Previous Articles Next Articles
Effect of neuromuscular exercise for knee osteoarthritis pain and function: a meta-analysis
Sun Yundi1, Cheng Lulu1, 2, Wan Haili3, Chang Ying1, Xiong Wenjuan1, Xia Yuan3
- 1School of Sports Medicine, Wuhan Sports University, Wuhan 430079, Hubei Province, China; 2Anhui University of Chinese Medicine, Anhui 230012, Anhui Province, China; 3The Affiliated Hospital of Hubei Provincial Government, Wuhan 430000, Hubei Province, China
-
Received:2023-12-25Accepted:2024-02-24Online:2025-03-28Published:2024-10-11 -
Contact:Xia Yuan, Master, Primary rehabilitation therapist, The Affiliated Hospital of Hubei Provincial Government, Wuhan 430000, Hubei Province, China -
About author:Sun Yundi, Master candidate, School of Sports Medicine, Wuhan Sports University, Wuhan 430079, Hubei Province, China -
Supported by:Key Program of Natural Science Research in Colleges and Universities in Anhui Province, No. 2023AH050725 (to CLL)
CLC Number:
Cite this article
Sun Yundi, Cheng Lulu, Wan Haili, Chang Ying, Xiong Wenjuan, Xia Yuan. Effect of neuromuscular exercise for knee osteoarthritis pain and function: a meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1945-1952.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
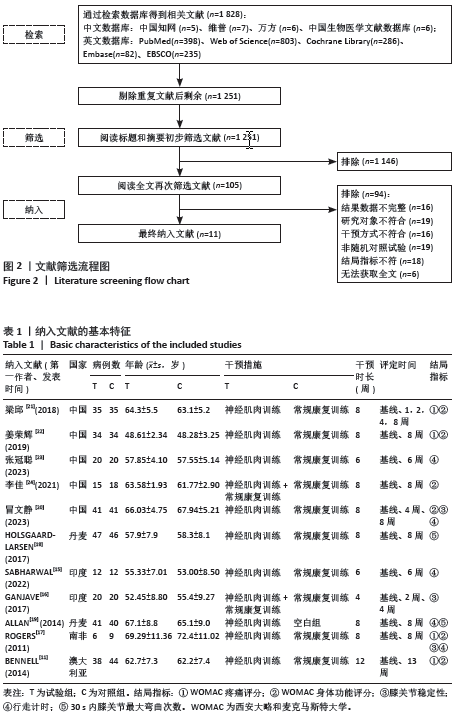
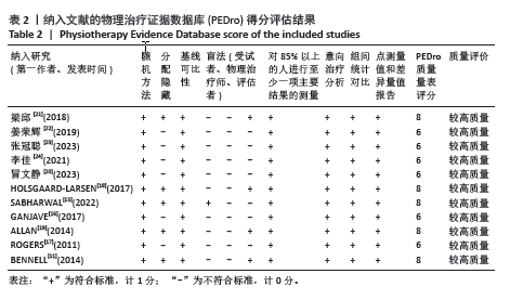
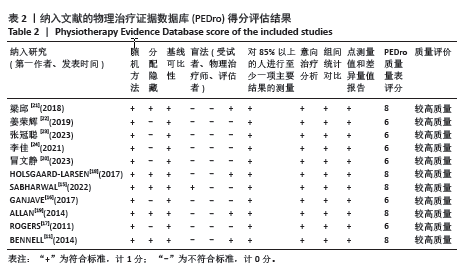
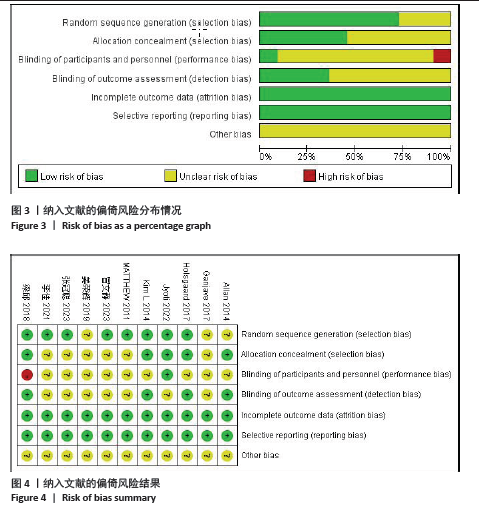
2.2 纳入文献的质量评价 纳入的11篇文献中全部提及“随机”或“随机对照试验”,8篇提及采用随机数字表或计算机随机生成数字等具体随机方法[11,15,17-18,20-21,23-24];有5篇文献提到具体的分配隐藏措施[11,15,18-19,21],其中1篇文献对试验受试者采用盲法[15],4篇文献结局指标评估者进行盲法评估[11,18-19,21]。所有文献均无选择性报告和数据不完整,均未提到其他偏倚的来源。各研究的偏倚风险所占情况和研究结果分别见图3,4。依据PEDro量表评分标准,在纳入的文献中,11篇均为大于6分的较高质量文献。纳入的文献整体质量较高,集中在6-8分之间,PEDro量表评分结果见表2。"

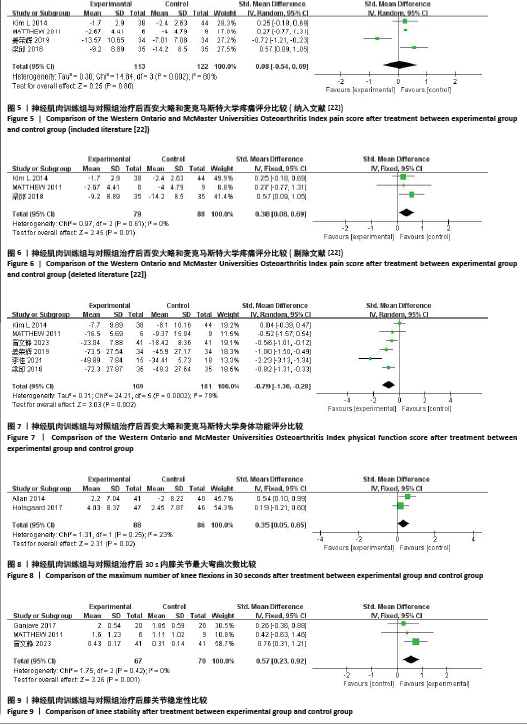
2.3 Meta分析结果 2.3.1 WOMAC评分 (1)WOMAC疼痛评分:共纳入4个随机对照试验[11,17,21-22],计算基线与末次随访WOMAC疼痛评分变化值,各研究异质性显著(I2=80%,P=0.002),见图5。剔除姜荣辉[22]的文献后,I2=0%,提示异质性可能来源该文献。由于研究间对WOMAC量表的赋值不同,故采用SMD进行合并。结果显示,两组间WOMAC疼痛评分相比差异有显著性意义,提示神经肌肉训练可改善膝骨关节炎患者WOMAC疼痛评分(SMD=0.38,95%CI:0.08-0.69,P=0.01),见图6。 (2)WOMAC身体功能评分:共纳入6个随机对照试验[11,17,20-22,24], 计算基线与末次随访WOMAC身体功能评分变化值,各研究异质性较大(I2=79%,P=0.000 2),逐一剔除文献后I2仍> 50%,采用随机效应模型。结果显示,两组间WOMAC身体功能评分相比差异有显著性意义(SMD=-0.79,95%CI:-1.30至-0.28,P=0.002),神经肌肉训练可改善膝骨关节炎患者WOMAC身体功能评分,见图7。 2.3.2 30 s内膝关节最大弯曲次数 共纳入2个随机对照试验[18-19],提示试验组对膝关节屈曲活动功能改善情况优于对照组,差异有显著性意义(SMD=0.35,95%CI:0.05-0.65,P=0.02) 。各研究异质性较小(I2=23%,P=0.25),提示神经肌肉训练可增加膝骨关节炎患者膝关节30 s内弯曲次数,提高膝关节功能,见图8。 2.3.3 膝关节稳定性 共纳入3个随机对照试验[16-17,20],提示试验组对膝关节稳定性的改善优于对照组,差异有显著性意义(SMD=0.57,95%CI:0.23-0.92,P=0.001) 。各研究同质性较好(I2=0%,P=0.42),提示神经肌肉训练可改善膝骨关节炎患者膝关节稳定性,见图9。"
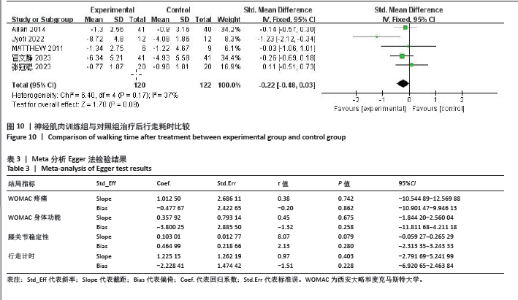
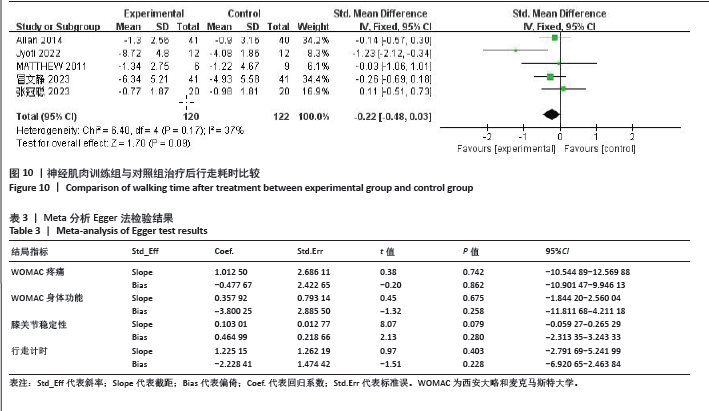
2.3.4 行走计时 共纳入5个随机对照试验[15,17,19-20,23],计算基线与末次随访膝关节行走计时的变化值,各研究异质性在可接受范围内(I2=37%,P=0.17)。由于研究间设定的行走距离不同,故采用SMD进行合并。结果显示,两组均可提高膝骨关节炎患者行走速度,改善行走能力,但差异无显著性意义(SMD=-0.22,95%CI:-0.48-0.03,P=0.09),见图10。 2.4 发表偏倚风险评价 通过Egger法运算评价纳入研究的发表偏倚,结果见表3。WOMAC疼痛(P=0.862)、WOMAC身体功能(P=0.258)、膝关节稳定性(P=0.280)、行走计时(P=0.228)的P值均> 0.05,表明结局指标所纳入的研究不存在明显的发表偏倚,纳入文献结果较为稳定。"
| [1] YE J, ZHENG Q, ZOU L, et al. Mindful Exercise (Baduanjin) as an Adjuvant Treatment for Older Adults (60 Years Old and Over) of Knee Osteoarthritis: A Randomized Controlled Trial. Evid Based Complement Alternat Med. 2020;2020:9869161. [2] 程露露, 李冬静, 李梦醒,等. 针灸治疗膝骨性关节炎作用机制研究概况[J]. 中国骨质疏松杂志,2022,28(10):1514-1517,1540. [3] 陈鉴冰, 叶倩云, 朱晓峰. 膝骨关节炎致病危险因素的meta分析[J]. 暨南大学学报(自然科学与医学版),2023,44(4):406-415. [4] SUN X, ZHEN X, HU X, et al. Osteoarthritis in the Middle Aged and Elderly in China: Prevalence and Influencing Factors. Int J Environ Res Public Health. 2019;16(23):4701. [5] AGEBERG E, ROOS EM. Neuromuscular exercise as treatment of degenerative knee disease. Exerc Sport Sci Rev. 2015;43(1):14-22. [6] PRIMEAU CA, BIRMINGHAM TB, MOYER RF, et al. Trajectories of perceived exertion and pain over a 12-week neuromuscular exercise program in patients with knee osteoarthritis. Osteoarthritis Cartilage. 2020;28(11):1427-1431. [7] CLAUSEN B, HOLSGAARD-LARSEN A, ROOS EM. An 8-Week Neuromuscular Exercise Program for Patients With Mild to Moderate Knee Osteoarthritis: A Case Series Drawn From a Registered Clinical Trial. J Athl Train. 2017;52(6):592-605. [8] JUHL C, CHRISTENSEN R, ROOS EM, et al. Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials. Arthritis Rheumatol. 2014;66(3):622-636. [9] HOLM PM, PETERSEN KK, WERNBOM M, et al. Strength training in addition to neuromuscular exercise and education in individuals with knee osteoarthritis-the effects on pain and sensitization. Eur J Pain. 2021;25(9):1898-1911. [10] GANJAVE PD, DABHOLKAR T. Efficacy of Neuromuscular Training on Pain, Balance and Function in Patients with Grade I and II Knee Osteoarthritis. J Exerc Sci Physiother. 2017;13(2):27-40. [11] BENNELL KL, KYRIAKIDES M, METCALF B, et al. Neuromuscular versus quadriceps strengthening exercise in patients with medial knee osteoarthritis and varus malalignment: a randomized controlled trial. Arthritis Rheumatol. 2014;66(4):950-959. [12] ALTMAN R, ASCH E, BLOCH D, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29(8):1039-1049. [13] 中华医学会骨科学分会关节外科学组. 骨关节炎诊疗指南(2018年版)[J]. 中华骨科杂志,2018,38(12):705-715. [14] MAHER CG, SHERRINGTON C, HERBERT RD, et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713-721. [15] SABHARWAL J, JOSHI S. Neuromuscular exercise with neuromuscular electrical stimulation in knee osteoarthritis: a randomised controlled pilot trial. 2022; 36(4):8‐16. [16] GANJAVE PRANITA D, TWINKLE D. Efficacy of Neuromuscular Training on Pain, Balance and Function in Patients with Grade I and II Knee Osteoarthritis. Exerc Sci Physiother. 2017;13(2):27-40. [17] ROGERS MW, TAMULEVICIUS N, COETSEE MF, et al. Knee Osteoarthritis and the Efficacy of Kinesthesia, Balance & Agility Exercise Training: A Pilot Study. Int J Exerc Sci. 2011;4(2):124-132. [18] HOLSGAARD-LARSEN A, CLAUSEN B, SØNDERGAARD J, et al. The effect of instruction in analgesic use compared with neuromuscular exercise on knee-joint load in patients with knee osteoarthritis: a randomized, single-blind, controlled trial. Osteoarthritis Cartilage. 2017;25(4):470-480. [19] VILLADSEN A, OVERGAARD S, HOLSGAARD-LARSEN A, et al. Immediate efficacy of neuromuscular exercise in patients with severe osteoarthritis of the hip or knee: a secondary analysis from a randomized controlled trial. J Rheumatol. 2014;41(7):1385-1394. [20] 冒文静, 丁彬鸿, 吴素青. 神经肌肉训练对老年膝骨关节炎患者关节稳定性及下肢运动功能的影响[J]. 海军医学杂志, 2023,44(1):74-78. [21] 梁邱, 何成奇, 姜俊良,等. 神经肌肉运动训练对膝骨关节炎患者的疼痛与功能恢复的临床疗效观察[J]. 华西医学,2018, 33(10):1247-1251. [22] 姜荣辉. 神经肌肉运动训练对膝骨关节炎患者的疼痛与功能恢复的临床疗效观察[J]. 世界最新医学信息文摘,2019,19(97): 40-41. [23] 张冠聪, 黄秋晨, 顾蕊,等. 不同神经肌肉训练方法对早期膝骨关节炎患者疼痛和运动功能效果的比较[J]. 中国康复理论与实践,2023,29(9):1090-1097. [24] 李佳, 张鸿悦, 刘晓磊,等. 神经肌肉训练对重度膝骨关节炎患者膝关节功能和姿势控制的影响[J]. 中国临床医生杂志, 2021,49(3):315-317. [25] 李志霞, 康玉闻, 刘永裕,等. 经筋灸法联合神经肌肉运动训练治疗膝骨关节炎的临床观察[J]. 中国医学创新,2021, 18(15):90-93. [26] BLALOCK D, MILLER A, TILLEY M, et al. Joint instability and osteoarthritis. Clin Med Insights Arthritis Musculoskelet Disord, 2015;8:15-23. [27] ZENG CY, ZHANG ZR, TANG ZM, et al. Benefits and Mechanisms of Exercise Training for Knee Osteoarthritis. Front Physiol. 2021;12:794062. [28] MICHAEL JW, SCHLüTER-BRUST KU, EYSEL P. The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee. Dtsch Arztebl Int. 2010;107(9):152-162. [29] BENNELL K, DOBSON F. Neuromuscular exercise for degenerative knees: can we optimize the treatment effect? Exerc Sport Sci Rev. 2015;43(1):3-4. [30] THORSTENSSON CA, HENRIKSSON M, VON PORAT A, et al. The effect of eight weeks of exercise on knee adduction moment in early knee osteoarthritis-a pilot study. Osteoarthritis Cartilage. 2007;15(10):1163-1170. [31] 胡浩宇. 神经肌肉训练技术对髌股疼痛综合症(PFPS)患者的疗效及其影响研究[D]. 上海:上海体育学院,2019. [32] GLASS NA, TORNER JC, FREY LAW LA, et al. The relationship between quadriceps muscle weakness and worsening of knee pain in the MOST cohort: a 5-year longitudinal study. Osteoarthritis Cartilage. 2013;21(9):1154-1159. [33] RASHID SA, MOIZ JA, SHARMA S, et al. Comparisons of Neuromuscular Training Versus Quadriceps Training on Gait and WOMAC Index in Patients With Knee Osteoarthritis and Varus Malalignment. J Chiropr Med. 2019;18(1):1-8. [34] BECKWéE D, VAES P, CNUDDE M, et al. Osteoarthritis of the knee: why does exercise work? A qualitative study of the literature. Ageing Res Rev. 2013;12(1):226-236. [35] DAINESE P, WYNGAERT KV, DE MITS S, et al. Association between knee inflammation and knee pain in patients with knee osteoarthritis: a systematic review. Osteoarthritis Cartilage. 2022;30(4):516-534. [36] HUNTER DJ, BEAVERS DP, ECKSTEIN F, et al. The Intensive Diet and Exercise for Arthritis (IDEA) trial: 18-month radiographic and MRI outcomes. Osteoarthritis Cartilage. 2015;23(7):1090-1098. [37] LESNAK JB, SLUKA KA. Mechanism of exercise-induced analgesia: what we can learn from physically active animals. Pain Rep. 2020;5(5):e850. [38] STEIDLE-KLOC E, RABE K, ECKSTEIN F, et al. Is muscle strength in a painful limb affected by knee pain status of the contralateral limb -Data from the Osteoarthritis Initiative. Ann Anat. 2019;221:68-75. [39] SANCHEZ-RAMIREZ DC, VAN DER LEEDEN M, KNOL DL, et al. Association of postural control with muscle strength, proprioception, self-reported knee instability and activity limitations in patients with knee osteoarthritis. J Rehabil Med. 2013;45(2):192-197. [40] ZENG Z, SHAN J, ZHANG Y, et al. Asymmetries and relationships between muscle strength, proprioception, biomechanics, and postural stability in patients with unilateral knee osteoarthritis. Front Bioeng Biotechnol. 2022;10:922832. [41] AGEBERG E, NILSDOTTER A, KOSEK E, et al. Effects of neuromuscular training (NEMEX-TJR) on patient-reported outcomes and physical function in severe primary hip or knee osteoarthritis: a controlled before-and-after study. BMC Musculoskelet Disord. 2013;14:232. [42] BREMANDER AB, DAHL LL, ROOS EM. Validity and reliability of functional performance tests in meniscectomized patients with or without knee osteoarthritis. Scand J Med Sci Sports. 2007;17(2):120-127. [43] URITANI D, KODA H, YASUURA Y, et al. Factors associated with subjective knee joint stiffness in people with knee osteoarthritis: A systematic review. Int J Rheum Dis. 2023; 26(3):425-436. [44] ROOS EM, DAHLBERG L. Positive effects of moderate exercise on glycosaminoglycan content in knee cartilage: a four-month, randomized, controlled trial in patients at risk of osteoarthritis. Arthritis Rheum. 2005;52(11):3507-3514. [45] ALESSANDRO C, PRASHARA A, TENTLER DP, et al. Inhibition of knee joint sensory afferents alters covariation across strides between quadriceps muscles during locomotion. J Appl Physiol (1985). 2023; 134(4):957-968. [46] 李永杰, 扈盛. 水中运动训练对脑卒中患者下肢肢体功能和日常生活能力影响的meta分析[J]. 中国康复医学杂志, 2019,34(10):1209-1215. [47] CHAHARMAHALI L, GANDOMI F, YALFANI A, et al. The effect of mindfulness and motivational interviewing along with neuromuscular exercises on pain, function, and balance of women affected by knee osteoarthritis: a rater-blinded randomized controlled clinical trial. Disabil Rehabil. 2023:1-12. [48] BELLAMY N, BUCHANAN WW, GOLDSMITH CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol.1988;15(12):1833-1840. [49] PENG YL, JOHNSON AE, GRIFFIN L. Sex differences in neuromuscular control of quadriceps. Eur J Appl Physiol. 2020; 120(10):2193-2202. [50] AMAN JE, ELANGOVAN N, YEH IL, et al. The effectiveness of proprioceptive training for improving motor function: a systematic review. Front Hum Neurosci. 2014;8:1075. [51] IRISH SE, MILLWARD AJ, WRIDE J, et al. The effect of closed-kinetic chain exercises and open-kinetic chain exercise on the muscle activity of vastus medialis oblique and vastus lateralis. J Strength Cond Res. 2010;24(5):1256-1262. [52] SLOBODOVÁ L, ORESKÁ Ľ, SCHÖN M, et al. Effects of Short- and Long-Term Aerobic-Strength Training and Determinants of Walking Speed in the Elderly. Gerontology. 2022;68(2):151-161. [53] SAZO-RODRÍGUEZ S, MÉNDEZ-REBOLLEDO G, GUZMÁN-MUÑOZ E, et al. The effects of progressive neuromuscular training on postural balance and functionality in elderly patients with knee osteoarthritis: a pilot study. J Phys Ther Sci. 2017;29(7):1229-1235. |
| [1] | Li Jiagen, Chen Yueping, Huang Keqi, Chen Shangtong, Huang Chuanhong. The construction and validation of a prediction model based on multiple machine learning algorithms and the immunomodulatory analysis of rheumatoid arthritis from the perspective of mitophagy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-15. |
| [2] | Ma Chi, Wang Ning, Chen Yong, Wei Zhihan, Liu Fengji, Piao Chengzhe. Application of 3D-printing patient-specific instruments combined with customized locking plate in opening wedge high tibial osteotomy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1863-1869. |
| [3] | Zhang Xinxin, Gao Ke, Xie Shidong, Tuo Haowen, Jing Feiyue, Liu Weiguo. Network meta-analysis of non-surgical treatments for foot and ankle ability and dynamic balance in patients with chronic ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1931-1944. |
| [4] | Liu Yan, Wang Kai, Wu Min. Relationship between coronal angle fluctuation of ankle point and recovery of joint function after ankle fracture [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1820-1826. |
| [5] | Wang Peiguang, Zhang Xiaowen, Mai Meisi, Li Luqian, Huang Hao. Generalized equation estimation of the therapeutic effect of floating needle therapy combined with acupoint embedding on different stages of human knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1565-1571. |
| [6] | Wang Yida, Liu Jun, Wang Xiaoling, Wang Liyan, Yang Chengru, Zhang Xuexiao. Effects of wearable electronic device-based interventions on physical activity and sedentary behavior in healthy adolescents: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1693-1704. |
| [7] | Zhang Zixian, Xu Youliang, Wu Shaokui, Wang Xiangying. Effects of blood flow restriction training combined with resistance training on muscle indicators in college athletes: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1705-1713. |
| [8] | Wang Juan, Wang Guanglan, Zuo Huiwu. Efficacy of exercise therapy in the treatment of anterior cruciate ligament reconstruction patients: #br# a network meta-analysis #br# [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1714-1726. |
| [9] | Zheng Huakun, Yin Mingyue, Liu Qian. Effects of interval and continuous training on the quality of life in physically inactive adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1727-1740. |
| [10] | He Guanghui, Yuan Jie, Ke Yanqin, Qiu Xiaoting, Zhang Xiaoling. Hemin regulates mitochondrial pathway of oxidative stress in mouse chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1183-1191. |
| [11] |
Liang Xiaoxiao, Zheng Jiejiao, Duan Linru, Chen Xi, Zhang Tingyu.
Characterization of postural stability in elderly patients with idiopathic normal pressure hydrocephalus #br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1208-1213.
|
| [12] | Ma Haoyu, Qiao Hongchao, Hao Qianqian, Shi Dongbo. Causal effects of different exercise intensities on the risk of osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1305-1311. |
| [13] | Li Jiatong, Jin Yue, Liu Runjia, Song Bowen, Zhu Xiaoqian, Li Nianhu . Association between thyroid function levels and phenotypes associated with sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1312-1320. |
| [14] | Wang Rongrong, Huang Yushan, Li Xiangmiao, Bai Jinzhu. Prostaglandin E1 regulates vascular-related factors and protects microcirculatory function during the acute phase of traumatic spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 958-967. |
| [15] | Wu Guangtao, Qin Gang, He Kaiyi, Fan Yidong, Li Weicai, Zhu Baogang, Cao Ying . Causal relationship between immune cells and knee osteoarthritis: a two-sample bi-directional Mendelian randomization analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1081-1090. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||