Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (13): 2690-2697.doi: 10.12307/2025.039
Previous Articles Next Articles
miR-212-3p regulates senescence of bone marrow mesenchymal stem cells by targeting MAPK3
Zhong Liying, Li Shundong, Wang Cong
- Department of Geriatrics, Third Hospital of Changsha, Changsha 410015, Hunan Province, China
-
Received:2023-11-28Accepted:2024-03-07Online:2025-05-08Published:2024-09-11 -
Contact:Li Shundong, MD, Chief physician, Department of Geriatrics, Third Hospital of Changsha, Changsha 410015, Hunan Province, China -
About author:Zhong Liying, Master, Associate chief physician, Department of Geriatrics, Third Hospital of Changsha, Changsha 410015, Hunan Province, China -
Supported by:Natural Science Foundation of Changsha, No. kq2208460 (to ZLY); Natural Science Foundation of Hunan Province, No. 2021JJ70055 (to LSD)
CLC Number:
Cite this article
Zhong Liying, Li Shundong, Wang Cong. miR-212-3p regulates senescence of bone marrow mesenchymal stem cells by targeting MAPK3[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(13): 2690-2697.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

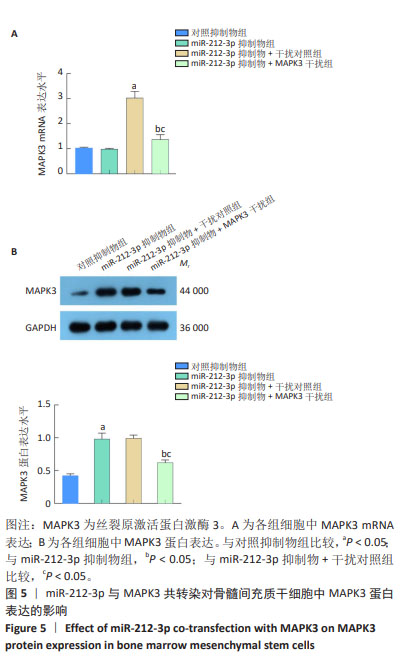
2.1 骨髓间充质干细胞形态观察及鉴定 原代分离的骨髓间充质干细胞培养24 h后细胞数量少,形态呈短纺锤状;5 d后细胞明显增殖,体积变大,形态多呈梭形;10 d后细胞融合度达90%。P3代细胞传代后两三天细胞融合度可达100%,见图1A。流式细胞表面抗原检测结果显示,CD44、CD90表达阳性,阳性率分别为(93.52±2.56)%,(98.38±2.12)%;CD31和CD45表达阴性,阳性率仅为(1.97±0.21)%,(0.55±0.06)%,见图1B。茜素红和油红O染色结果显示,骨髓间充质干细胞经定向成骨、成脂诱导分化后可形成明显矿化结节和脂滴,见图1C,D。以上结果提示分离培养的细胞为大鼠骨髓间充质干细胞。 2.2 H2O2促进骨髓间充质干细胞衰老及p16和p21蛋白表达 β-半乳糖苷酶染色结果显示,与对照组比较,模型组阳性着色细胞数显著增加(P < 0.05),见图2A。Western blot结果显示,与对照组比较,模型组骨髓间充质干细胞中p16和p21蛋白表达升高(P < 0.05),见图2B。以上结果提示,骨髓间充质干细胞衰老模型建立成功。 2.3 miR-212-3p及MAPK3在衰老骨髓间充质干细胞中的表达水平 qRT-PCR检测结果显示,与对照组比较,模型组骨髓间充质干细胞中miR-212-3p mRNA表达升高(P < 0.05),MAPK3 mRNA表达降低(P < 0.05),见图3A,B。Western blot检测结果显示,与对照组比较,模型组骨髓间充质干细胞中MAPK3蛋白表达降低(P < 0.05),见图3C。 2.4 MAPK3是miR-212-3p下游靶基因 TargetScanHuman 7.1在线数据库预测结果显示,miR-212-3p与MAPK3存在靶向结合位点,见图4A。双荧光素酶结果显示,与对照模拟物组比较,miR-212-3p模拟物组细胞中野生型MAPK3 3’UTR荧光素酶活性明显降低(P < 0.05),而突变型MAPK3 3’UTR荧光素酶活性无明显变化(P > 0.05),见图4B。 qRT-PCR检测结果显示,与对照组或对照抑制物组比较,miR-212-3p抑制物组细胞中miR-212-3p表达降低(P < 0.05),MAPK3 mRNA表达升高(P < 0.05),见图4C,D。Western blot结果显示,与对照组或对照抑制物组比较,miR-212-3p抑制物组细胞中MAPK3蛋白表达升高(P < 0.05),见图4E。"
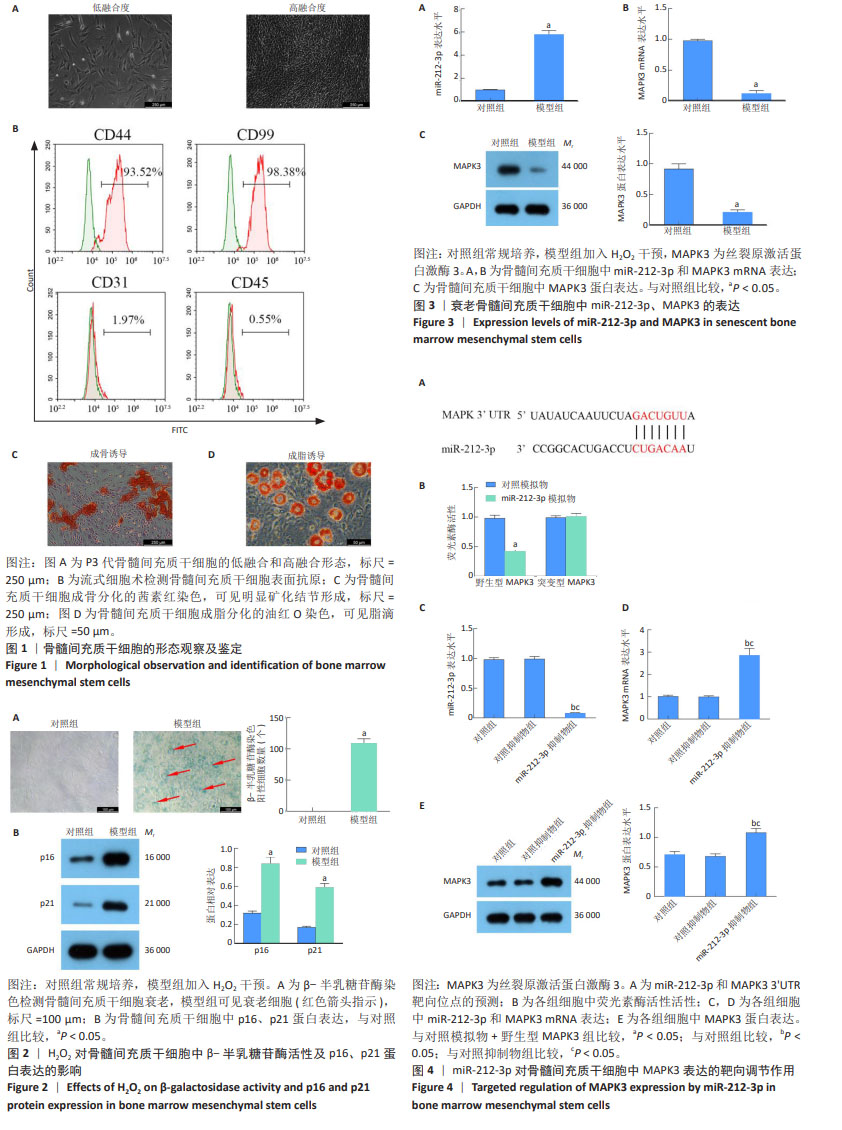

β-半乳糖苷酶染色结果显示,与H2O2+对照抑制物组比较,H2O2+miR-212-3p抑制物组细胞阳性着色细胞数明显减少(P < 0.05);与H2O2+miR-212-3p抑制物组或H2O2+miR-212-3p抑制物+干扰对照组比较,H2O2+miR-212-3p抑制物+MAPK3干扰组阳性着色细胞数明显增加(P < 0.05),见图6A。Western blot检测结果显示,与H2O2+对照抑制物组比较,H2O2+miR-212-3p抑制物组细胞中p16和p21蛋白表达降低(P < 0.05);与H2O2+miR-212-3p抑制物组或H2O2+miR-212-3p抑制物+干扰对照组比较,H2O2+miR-212-3p抑制物+MAPK3干扰组细胞中p16和p21蛋白表达升高(P < 0.05),见图6B。"

| [1] QADIR A, LIANG S, WU Z, et al. Senile osteoporosis: The involvement of differentiation and senescence of bone marrow stromal cells. Int J Mol Sci. 2020;21(1):349. [2] 李小云,林青,王昊宇,等.骨髓间充质干细胞衰老与骨质疏松症的研究进展[J].中国病理生理杂志,2023,39(10):1898-1903. [3] 刘少斐,许冰冰.骨髓间充质干细胞的分离、培养、鉴定及其在关节软骨损伤修复中的相关应用[J].中国比较医学杂志,2023, 33(9):149-154. [4] XU W, YANG Y, LI N, et al. Interaction between mesenchymal stem cells and immune cells during bone injury repair. Int J Mol Sci. 2023; 24(19):14484. [5] JIANG Y, ZHANG P, ZHANG X, et al. Advances in mesenchymal stem cell transplantation for the treatment of osteoporosis. Cell Prolif. 2021;54(1):e12956. [6] LIU F, YUAN Y, BAI L, et al. LRRc17 controls BMSC senescence via mitophagy and inhibits the therapeutic effect of BMSCs on ovariectomy-induced bone loss. Redox Biol. 2021;43:101963. [7] PI C, MA C, WANG H, et al. MiR-34a suppression targets Nampt to ameliorate bone marrow mesenchymal stem cell senescence by regulating NAD+-Sirt1 pathway. Stem Cell Res Ther. 2021;12(1):271. [8] LI Y, NIE J, WU Q, et al. Circ-Sirt1 promotes osteoblast differentiation by activating Sirt1 and Wnt/β-catenin pathway. Acta Biochim Pol. 2023; 70(1):51-57. [9] HAN Y, YANG Q, HUANG Y, et al. Long non-coding RNA SNHG5 promotes the osteogenic differentiation of bone marrow mesenchymal stem cells via the miR-212-3p/GDF5/SMAD pathway. Stem Cell Res Ther. 2022;13(1):130. [10] 杨春丽,陆金芝,刘贝贝,等.大鼠骨髓间充质干细胞的原代培养及鉴定[J].现代生物医学进展,2023,23(18):3425-3430. [11] YANG Q, ZOU Y, WEI X, et al. PTP1B knockdown alleviates BMSCs senescence via activating AMPK-mediated mitophagy and promotes osteogenesis in senile osteoporosis. Biochim Biophys Acta Mol Basis Dis. 2023;1869(7):166795. [12] QADIR A, LIANG S, WU Z, et al. Senile Osteoporosis: The Involvement of Differentiation and Senescence of Bone Marrow Stromal Cells. Int J Mol Sci. 2020;21(1):349. [13] SHMULEVICH R, KRIZHANOVSKY V. Cell senescence, DNA mamage, and metabolism. Antioxid Redox Signal. 2021;34(4):324-334. [14] GROSSE L, WAGNER N, EMELYANOV A, et al. Defined p16High senescent cell types are indispensable for mouse healthspan. Cell Metab. 2020;32(1):87-99.e6. [15] RITZENTHALER JD, TORRES-GONZALEZ E, ZHENG Y, et al. The profibrotic and senescence phenotype of old lung fibroblasts is reversed or ameliorated by genetic and pharmacological manipulation of Slc7a11 expression. Am J Physiol Lung Cell Mol Physiol. 2022;322(3):L449-L461. [16] LIU ZZ, HONG CG, HU WB, et al. Autophagy receptor OPTN (optineurin) regulates mesenchymal stem cell fate and bone-fat balance during aging by clearing FABP3. Autophagy. 2021;17(10):2766-2782. [17] XING X, TANG Q, ZOU J, et al. Bone-targeted delivery of senolytics to eliminate senescent cells increases bone formation in senile osteoporosis. Acta Biomater. 2023;157:352-366. [18] LU J, ZHANG Y, LIANG J, et al. Role of exosomal microRNAs and their crosstalk with oxidative stress in the pathogenesis of osteoporosis. Oxid Med Cell Longev. 2021;2021:6301433. [19] ALKAN AH, AKGÜL B. Endogenous miRNA sponges. Methods Mol Biol. 2022;2257:91-104. [20] BAI WY, XIA JW, RONG XL, et al. Integrative analysis of genomic and epigenomic data reveal underlying superenhancer-mediated microRNA regulatory network for human bone mineral density. Hum Mol Genet. 2021;30(22):2177-2189. [21] ZHANG Y, JIANG Y, LUO Y, et al. Interference of miR-212 and miR-384 promotes osteogenic differentiation via targeting RUNX2 in osteoporosis. Exp Mol Pathol. 2020;113:104366. [22] ZHANG L, XU L, WANG Y, et al. Histone methyltransferase Setdb1 mediates osteogenic differentiation by suppressing the expression of miR-212-3p under mechanical unloading. Cell Signal. 2023;102:110554. [23] XIAO F, PENG J, LI Y, et al. Small noncoding RNAome changes during human bone marrow mesenchymal stem cells senescence in bitro. Front Endocrinol (Lausanne). 2022;13:808223. [24] DUAN L, ZHAO Y, JIA J, et al. Myeloid-restricted CD68 deficiency attenuates atherosclerosis via inhibition of ROS-MAPK-apoptosis axis. Biochim Biophys Acta Mol Basis Dis. 2023; 1869(5):166698. [25] MARTINA JA, JEONG E, PUERTOLLANO R. p38 MAPK-dependent phosphorylation of TFEB promotes monocyte-to-macrophage differentiation. EMBO Rep. 2023;24(2):e55472. [26] 张玲莉,雷乐,吴伟. MAPK信号通路在骨髓间充质干细胞向成骨细胞分化中的作用[J].中华骨质疏松和骨矿盐疾病杂志,2021, 14(1):75-81. [27] LIU YQ, XU YC, SHUAI ZW. Mir-142-3P regulates MAPK protein family by inhibiting 14-3-3η to enhance bone marrow mesenchymal stem cells osteogenesis. Sci Rep. 2023;13(1):22862. [28] ZHANG Y, DONG Y, WEI Q, et al. miR-126 mitigates the osteogenic differentiation of human bone marrow-derived mesenchymal stem cells by targeting the ERK1/2 and Bcl-2 pathways. Acta Biochim Biophys Sin (Shanghai). 2023;55(3):449-459. [29] LIMRAKSASIN P, NATTASIT P, MANOKAWINCHOKE J, et al. Application of shear stress for enhanced osteogenic differentiation of mouse induced pluripotent stem cells. Sci Rep. 2022;12(1):19021. [30] XU C, LIU H, HE Y, et al. Endothelial progenitor cells promote osteogenic differentiation in co-cultured with mesenchymal stem cells via the MAPK- dependent pathway. Stem Cell Res Ther. 2020;11(1):537. [31] YAN Z, OHUCHIDA K, FEI S, et al. Inhibition of ERK1/2 in cancer-associated pancreatic stellate cells suppresses cancer-stromal interaction and metastasis. J Exp Clin Cancer Res. 2019;38(1):221. [32] CHEN J, CHEN Z, YUAN P, et al. ERK1 loss accelerates the progression of osteoarthritis in aged mice via NRF2/BACH1 signaling. Biochem Biophys Res Commun. 2022;622:129-135. [33] FATHI E, VIETOR I. Mesenchymal stem cells promote caspase expression in Molt-4 leukemia cells via GSK-3α/Β and ERK1/2 signaling pathways as a therapeutic strategy. Curr Gene Ther. 2021;21(1):81-88. |
| [1] | Yang Zhihang, Sun Zuyan, Huang Wenliang, Wan Yu, Chen Shida, Deng Jiang. Nerve growth factor promotes chondrogenic differentiation and inhibits hypertrophic differentiation of rabbit bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1336-1342. |
| [2] | Liu Qi, Li Linzhen, Li Yusheng, Jiao Hongzhuo, Yang Cheng, Zhang Juntao. Icariin-containing serum promotes chondrocyte proliferation and chondrogenic differentiation of stem cells in the co-culture system of three kinds of cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1371-1379. |
| [3] | Zhang Zhenyu, Liang Qiujian, Yang Jun, Wei Xiangyu, Jiang Jie, Huang Linke, Tan Zhen. Target of neohesperidin in treatment of osteoporosis and its effect on osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1437-1447. |
| [4] | Sun Xianjuan, Wang Qiuhua, Zhang Jinyi, Yang Yangyang, Wang Wenshuang, Zhang Xiaoqing. Adhesion, proliferation, and vascular smooth muscle differentiation of bone marrow mesenchymal stem cells on different electrospinning membranes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 661-669. |
| [5] | Ge Xiao, Zhao Zhuangzhuang, Guo Shuyu, Xu Rongyao. HOXA10 gene-modified bone marrow mesenchymal stem cells promote bone regeneration [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7701-7708. |
| [6] | Zhang Xiongjinfu, Chen Yida, Cheng Xinyi, Liu Daihui, Shi Qin . Exosomes derived from bone marrow mesenchymal stem cells of young rats to reverse senescence in aged rat bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7709-7718. |
| [7] | Sima Xinli, Liu Danping, Qi Hui. Effect and mechanism of metformin-modified bone marrow mesenchymal stem cell exosomes on regulating chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7728-7734. |
| [8] | Liu Chengyuan, Guo Qianping. Differential effects of kartogenin on chondrogenic and osteogenic differentiation of rat and rabbit bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7490-7498. |
| [9] | Liu Xun, Ouyang Hougan, Pan Rongbin, Wang Zi, Yang Fen, Tian Jiaxuan . Optimal parameters for physical interventions in bone marrow mesenchymal stem cell differentiation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6727-6732. |
| [10] | Zhao Yihan, Sun Xuhang, Zhao Lin, Jiang Shiqing. Effects and mechanisms of exosomal miRNA in treatment of multiple myeloma [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6743-6752. |
| [11] | Shao Xuekun, Shi Dianhua, Ding Zhiping, Qiu Zhuoya, Wang Ping, Wang Yi, Wang Cheng, Ding Xiaoyan, Sun Tiefeng. Calcined deer antler slices promote proliferation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6601-6608. |
| [12] | Lin Shuqian, Zhao Xilong, Gao Jing, Pan Xinghua, Li Zian, Ruan Guangping. Comparison of biological characteristics of mouse bone marrow mesenchymal stem cells after interference and overexpression of telomere Cajal body protein-1 [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6616-6624. |
| [13] | Liang Zhifeng, Yang Yingcai, Cheng Qiangang, Jia Yongxing, Wang Bo . Effect of stromal cell-derived factor-1 in cartilage and subchondral bone homeostasis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(25): 5422-5433. |
| [14] | Liu Chenyang, Wang Jin, Zhang Wenting, Wang Liqing, Yin Xiaoxiao, Zhao Junnan, Jiao Xiangying. Inhibitory effect of angiotensin II on the brown fat differentiation of rat bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(23): 4859-4867. |
| [15] | Feng Qiang, Pi Yihua, Huang Huasheng, Huang Delun, Zhang Yan. Bone marrow mesenchymal stem cell transplantation for myocardial infarction in rats: effects of acute and chronic exercises [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(23): 4868-4877. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||